Survey of glaucoma surgical preferences and post-operative care in the United Kingdom
Abstract
Background
To evaluate the spectrum of glaucoma surgery and the post-operative follow-up regimes undertaken among glaucoma specialists in the United Kingdom.
Design
National survey.
Participants
Seventy-five glaucoma specialists (consultants and fellows).
Methods
An eight-question survey was emailed to all glaucoma subspecialists members of the United Kingdom and Eire Glaucoma Society.
Main Outcome Measures
Surgery undertaken, post-operative management, awareness of intervention tariff and handling of the follow-up burden generated through surgery.
Results
Almost all the participants (74/75: 99%) routinely performed trabeculectomy, 54 responders (72%) undertook tube surgery and Minimally Invasive Glaucoma Surgery (MIGS) was more frequently undertaken (33.0%) than non-penetrating surgery (23%).
In general, for patients with advanced glaucoma requiring a low target intraocular pressure (IOP), the most frequent primary intervention was trabeculectomy (99%), followed by tubes (64%). Similarly, in patients with less advanced glaucoma requiring moderate target IOP, participants preferred trabeculectomy (99%), followed by MIGS (60%). By the first 6 months after the procedure, trabeculectomy and Baerveldt tube implant required a larger number of postoperative visits (9 and 7, respectively), than iStent® and non-penetrating deep sclerectomy (3 and 5, respectively).
The majority of participants were not aware of the costs of their interventions.
Conclusions
A wide variety of glaucoma surgery techniques are undertaken. Post-operative follow-up regimes are variable between techniques and for surgeons using the same technique. Trabeculectomy requires more follow-up than any other intervention. For patients requiring low IOP, trabeculectomy is the operation of choice for most surgeons.
Introduction
In 2012 over 7500 incisional glaucoma surgeries were undertaken in the United Kingdom (UK), the vast majority were trabeculectomy and glaucoma drainage devices.1 Recently, a new generation of glaucoma surgery interventions has been developed. These add further options to the surgical choices available to treat glaucoma and are currently being adopted in the UK and elsewhere. Profiling interventions at a defined time point provides valuable insights into the variety of interventions being used, their frequency of use and the indications dictating their use, thus establishing a bench mark of current practice and setting a reference point against which future comparisons may be made. Several previous UK national surveys on aspects of glaucoma care have provided valuable insight into the attitudes and treatments undertaken by glaucoma specialists, and these have informed opinion and provided baseline observations for future reference.2, 3 To our knowledge, no previous survey has attempted to evaluate the spectrum and frequency with which glaucoma surgery interventions have been undertaken by individual surgeons. In addition, there is little information about the follow-up regimes adopted by surgeons for these interventions and how they manage the burden of intensive post-operative follow-up associated with glaucoma surgery. There is a realistic possibility that service delivery pressures and new innovations may change the landscape of glaucoma surgery delivery, and we believe this is a good time to generate a profile of current practice of the types, frequency and indications used for glaucoma surgery, not only to inform opinion but also to act as a comparator for future investigations of glaucoma surgery habits in the UK and elsewhere.
Methods
An eight-question survey was designed using a commercial website (http://www.surveymonkey.com) (Appendix 1). The survey collected information about the grade of respondents, types of glaucoma surgery they undertook and approaches to management of patients with advanced or non-advanced disease. Post-operative follow-up frequency, strategies to manage this frequency burden and clinician insight into the intervention tariff for each intervention were also explored.
The questionnaire was circulated to the members of the UK and Eire Glaucoma Society (UKEGS) (http://www.glaucoma-societyuke.org) in December 2015. The membership of UKEGS comprises of clinical glaucoma specialists (Consultants and Fellows), specialist opticians, ophthalmology trainees and nurses. All members received the survey and were asked to indicate which group they belonged to. After 6 weeks, a reminder was sent to capture the non-responders.
Data was analysed using surveymonkey.com analysis tools and Microsoft Excel (Microsoft Corporation, Redmond, WA, USA). Where responders skipped questions, they were omitted from percentage calculations for that particular question. All percentage values were rounded to the nearest whole number from presentation.
Results
A total of 75 glaucoma specialists, 64/116 (55%) glaucoma consultants and 11/11 (100%) glaucoma fellows, responded, of which 65 (87%) completed all questions in the survey.
Types of glaucoma surgery
Of the 75 respondents, 74 (99%) (Fig. 1) performed trabeculectomy augmented with mitomycin C. One participant did not and only performed glaucoma drainage implant (GDI) surgery.
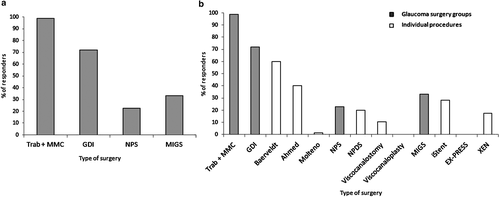
Fifty-four responders (72%) (Fig. 1) indicated they performed glaucoma device implants (GDI). Baerveldt implant was the most frequently performed, undertaken by 83% of responders in GDI group.
Seventeen responders (23%) (Fig. 1) indicated that they performed non-penetrating surgery (NPS). Non-penetrating deep sclerectomy (NPDS) was the most frequently performed undertaken by 88% of responders in NPS group.
Twenty-five responders (33%) (Fig. 1) indicated that they implanted at least one type of minimally invasive glaucoma surgery (MIGS) device and nine (36% of MIGS group) performed at least two of them. iStent® was the most commonly undertaken MIGS performed by 84% of responders in MIGS group. Thirteen responders (52% of responders in the MIGS group) performed XEN® and none performed EX-PRESS®. Table 1 summarizes the frequency of the different procedures undertaken.
| Consultants | Fellows | Total | |
|---|---|---|---|
| Trabeculectomy + MMC | 63 (98) | 11 (100) | 74 (99) |
| GDI | 43 (67) | 11 (100) | 54 (72) |
| Baerveldt implant | 34 (53) | 11 (100) | 45 (60) |
| Ahmed valve | 26 (41) | 4 (36) | 30 (40) |
| Molteno implant | 1 (2) | 0 (0) | 1 (1) |
| NPS | 15 (23) | 2 (18) | 17 (25) |
| Deep sclerectomy | 13 (20) | 2 (18) | 15 (20) |
| Viscocanalostomy | 7 (11) | 1 (9) | 8 (11) |
| Viscocanaloplasty | 0 (0) | 0 (0) | 0 (0) |
| MIGS | 17 (27) | 8 (73) | 25 (33) |
| iStent® | 15 (23) | 6 (55) | 21 (28) |
| EXPRESS® | 0 (0) | 0 (0) | 0 (0) |
| XEN® | 9 (14) | 4 (36) | 13 (17) |
- GDI, glaucoma drainage implants; MIGS, minimally invasive glaucoma surgery; MMC, mitomycin C; NPS, non-penetrating surgery.
Table 2 shows the frequency of interventions undertaken by consultants and fellows and combinations undertaken. Just over 33% of surgeons undertook both GDI and trabeculectomy surgery and 21.3% undertook GDI, trabeculectomy and MIGS. Seventeen percent (17%) of glaucoma subspecialists performed only trabeculectomy and 1.3% performed only GDI, none undertook NPS or MIGS in isolation.
| Procedure | N | % |
|---|---|---|
| Trabeculectomy alone | 13 | 17 |
| GDI alone | 1 | 1 |
| Trabeculectomy + GDI | 25 | 33 |
| Trabeculectomy + NPS | 5 | 7 |
| Trabeculectomy + MIGS | 3 | 4 |
| Trabeculectomy + GDI + NPS | 6 | 8 |
| Trabeculectomy + GDI + MIGS | 16 | 21 |
| Trabeculectomy + GDI + NPS + MIGS (all the studied groups) | 6 | 8 |
- GDI, glaucoma drainage implants; MIGS, minimally invasive glaucoma surgery; NPS, non-penetrating surgery.
Six responders (8.0%) (four consultants and two fellows) performed surgery from each of the groups of glaucoma surgery presented in this survey (Table 2). All fellows (n = 11) performed trabeculectomy and tubes, of which two (18%) also performed NPS and MIGS.
Types of surgery for different target intraocular pressure
Seventy-three respondents indicated their preferences in patients with advanced glaucoma (Fig. 2a). Trabeculectomy with MMC (71 respondents) was always considered as the primary glaucoma intervention by 56 responders (79%) and sometimes by 14 responders (20%) and never by one respondent. Tubes (36 respondents) were always used as the first surgical option by one responder (3%), and sometimes by 22 responders (61%) and never by 13 (36%) respondents. NPS (30 respondents) was always considered as the primary intervention by one responder (3%) nine (30%) sometimes used it and 20 (67%) never used it. None of the respondents (29 respondents) always used MIGS devices as the first option to manage advanced glaucoma while six responders (20.7%) sometimes used them.
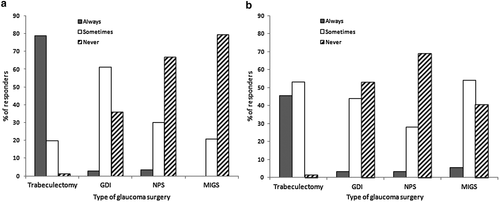
Seventy-two respondents indicated their preferences in patients with non-advanced glaucoma (Fig. 2b). Trabeculectomy with MMC (66 respondents) was always considered as the primary intervention by 30 (46%) responders and sometimes by 35 responders (53%). One participant (2%) indicated that they would never do a trabeculectomy. Tubes (32 respondents) were always used as the first surgical option by one responder (3%), and sometimes by 14 responders (44%). NPS (32 respondents) was always performed by one (3%) respondent and nine (28%) sometimes did. MIGS (37 respondents) were always chosen by two participants (5%), while 20 responders (54%) considered them sometimes.
Post-operative management
Figure 3 shows the follow-up intervals adopted for each of the interventions. The times until the first post-operative checks varied amongst the different techniques and amongst responders doing the same procedure. Many respondents (n = 75) reviewed their patients on the first day for, Molteno tube 100%, trabeculectomy 95%, XEN® implant 93%, Baerveldt tube 90% and Ahmed valve 88%; first day review was less for viscocanalostomy 75%, NPDS 69% and iStent® implant 60%. A second routine follow-up visit after 7 days varied from 67% for iStent® to 95% for trabeculectomy. Regardless of the surgical technique, the majority of responders (62%) checked their patients at 1 day and 1 week after surgery.
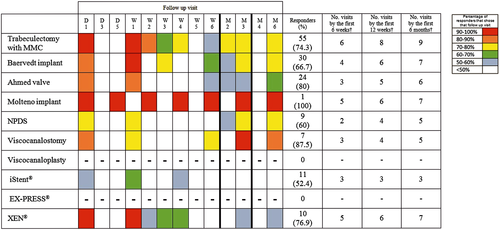
Post-operative visit burden
The burden of follow-up was greatest for trabeculectomy, at the 6 and 12 weeks and 6 months follow-up time points. Trabeculectomy required one visit more than the next nearest (Molteno) at 6 weeks and two more than the next nearest (Beareldt, Molteno and XEN®) at 12 weeks and 6 months. The follow-up burden by 6 weeks was least with NPDS and at 12 weeks and 6 months was least with iStent. The difference in follow-up burden between the interventions requiring the most and least frequent follow-up was four visits at 6 weeks, five visits at 12 weeks and six visits at 6 months.
In all (n = 75), 69% of responders took the frequency of routine post-operative outpatient department (OPD) follow-up into consideration, at least occasionally (always, most of times and occasionally), 40% doing it on a regular basis (always and most of times). However 36.8% of them roughly never or never did it (Fig. 4a).
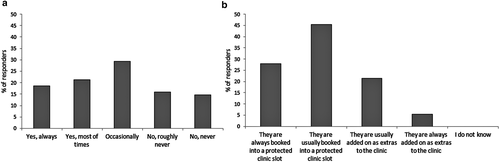
In all (n = 75), 73% of responders systematically booked their routine postoperative follow-ups into a protected clinic slot, while 27% of them added patients as extras to the clinic (Fig. 4b).
Surgery re-imbursement
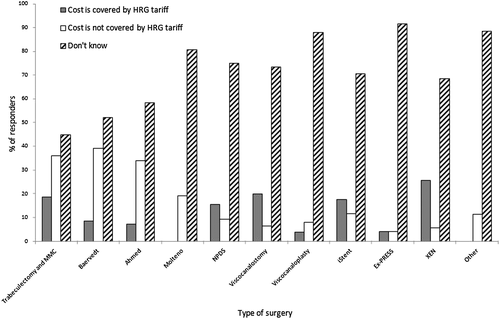
In general, responders (n = 73) did not know if the Healthcare Resource Group (HRG) national tariff received by the hospital was sufficient to cover the cost (Fig. 5). However for those that did have an opinion, for trabeculectomy (n = 69) more thought that cost was not covered (Not covered: 36% vs. Covered: 19%) similarly for Baerveldt tube (n = 46) (Not covered: 39% vs. Covered: 9%) and other tubes. However, more responders thought that the tariff did cover NPDS (n = 32) (Covered: 16% vs. Not covered: 9%), viscocanalostomy (n = 30) (Covered: 20% vs. Not covered: 7%), iStent® (n = 34) (Covered: 18% vs. Not covered: 12%) and XEN® (n = 35) (Covered: 26% vs. Not covered: 6%) costs (Fig. 5). The results were similar for consultants and fellows regarding every type of glaucoma surgery (data not shown).
Discussion
Glaucoma is a major and lifelong chronic disease which frequently requires surgical intervention. Until recently, the range of glaucoma surgery undertaken in the UK has been limited and dominated by trabeculectomy.1 In recent years, the indications for and popularity of tube surgery have increased.1 However, the introduction on minimally invasive glaucoma surgery over the last 3 years threatens to further alter to landscape of surgery in the future.
Trabeculectomy augmented with MMC remains the most frequent glaucoma procedure undertaken in the UK. This has been the gold standard glaucoma operation for the last 50 years4, 5 and is the primary surgery recommended by National Institute for Health and Care Excellence (NICE),6 the European Glaucoma Society guidelines7 and Preferred Practice Patterns of the American Academy of Ophthalmology.8 and has a large evidence base supporting its success and safety.9, 10 Its position may also reflect an experienced cohort of surgeons who have been undertaking trabeculectomy for many years and a reluctance to change what they are comfortable with. NPS is undertaken by only a small proportion of glaucoma specialists despite being used for over 20 years; in our survey, all of these also undertook trabeculectomy suggesting that they are selective about its use, possibly related to uncertainty regarding intraocular pressure (IOP) lowering compared with trabeculectomy.11 A relatively large proportion of respondents are now undertaking MIGS especially in the glaucoma fellow group, even though these interventions are only a recent development with a limited evidence base supporting their use. Neither EX-PRESS® shunt, trabectome or viscocanaloplasty seems to have been adopted in the UK.
For patients with advanced glaucoma four-fifths of responders routinely performed trabeculectomy as the primary intervention. This may reflect recognition of successful outcomes and low IOP potentially achieved by augmented trabeculectomy,9, 12 particularly in cases of advanced glaucoma.13 However, trabeculectomy is not universally considered for all advanced glaucoma patients as two-thirds of responders sometimes considered performing GDI surgery for such patients. Unfortunately, we are not sure what indication would lead surgeons to use GDI in patients with advanced POAG, although it is possible following the results of the Tube versus Trabeculectomy study that some may prefer to use a tube in eyes with a higher risk of failure.14 Both NPS and MIGS usage are uncommon for advanced glaucoma. For NPS, this may reflect the perception of less effective IOP lowering11 whereas for MIGS it may either reflect insufficient lowering of IOP reported thus far in the literature, insufficient experience of those using them to be confident of a good IOP lowering effect or experience suggesting that they do not sufficiently lower IOP for this group of patients.
The pattern of choice of surgery intervention was different in patients with less advanced glaucoma requiring moderate IOP lowering, and while augmented trabeculectomy remained the most popular ‘always’ choice at about 45% of responders, there was a slight increase in the use of both the NPS and GDI group. MIGS features more frequently in this group perhaps reflecting less concern about achieving low IOP levels for these patients and perhaps also reflecting their advantage as less surgically challenging interventions than trabeculectomy and less follow-up requirement. This maybe an indication of the position of MIGS interventions in the future.
Frequent follow-up after trabeculectomy is found with routine monitoring, at least weekly for the first month.15 (Fig. 3). This frequency is to allow proactive and reactive management of the bleb.9, 15-17 Similar frequencies of follow-up have been noted before.16, 18-20 Trabeculectomy required more total follow-up and more follow-up visits by 6 weeks, 12 weeks and 6 months than any other type of surgery. Most respondents expect to review their patients 8 times in the first 3 months and 9 times by 6 months. This requirement is resource intensive and inconvenient for patients and is in the author's opinion likely to be unsustainable with an ageing population where demand for glaucoma care is expanding.
Early interventions following GDI surgery are usually limited to monitoring IOP and either adjusting glaucoma medications or removing a suture stent or releasing a tube ligature in non-valved GDI. Panarelli et al.21 proposed careful postoperative planning with frequent follow-up visits to improve long-term outcomes of GDI. In general, Baerveldt surgery required an additional visit over Ahmed implants, presumably as the IOP control is achieved immediately with valved devices there is no routine monitoring of a hypertensive post-operative period. Both interventions required fewer visits than trabeculectomies at all time points.
The lower early complication rate for NPS techniques compared with trabeculectomy11, 22-25 may explain the reduced visit frequency. A previous report suggests postoperative evaluation after NPDS of: day 1, day 7 and 1, 3 and 6 months.25, 26 This regime is consistent with the results of the presented survey (Fig. 3). Thus, non-penetrating surgery required fewer follow-up visits than trabeculectomy.
More than 50% of responders routinely implanting iStent® reviewed their patients on day 1, day 7 and month 1 (Fig. 3). XEN® implant seems to require more follow-up visits than iStent®. These two devices have very different mechanisms of action with XEN® aiming to mimic trabeculectomy, and this may be reflected in the higher post-operative follow-up frequency suggesting that there may be need for similar post-operative manipulations to trabeculectomy and this may influence its widespread adoption.
There is wide variation in the follow-up regimes adopted for the same techniques by different surgeons. No evidence base exists to support the optimum follow-up regimes for any form of glaucoma surgery; further research to evaluate optimum follow-up frequency for the different forms of glaucoma surgery may eliminate this variation and ensure more efficient use of outpatient resources.
The need for frequent postoperative visits was taken into account when deciding what surgery to undertake by only one-third of the responders, suggesting they are making decisions based on their perceived efficacy of interventions chosen rather than OPD follow-up requirement. Almost three-quarters of the responders reported routinely booking their follow-ups into a protected clinic slot rather that adding them on as extras to their clinics. These results show most consultants are planning for the post-operative burden surgery generates. However, as OPD capacity becomes challenged by the demands of an ageing population, pressure to reduce post-operative care burden may increase and this may influence surgery choices in the future.
Most responders were not aware about the current costs of glaucoma surgeries. This may reflect the delivery of care through the national health service in the UK. Insight into the costs of surgery and the effectiveness of tarrifs for covering costs may further influence the choices of surgery undertaken especially in cases where the costs of surgery are not covered by the national tarrif. Over 50% of respondents were aware of the tariff for trabeculectomy, the most commonly undertaken procedure. However, most were unaware of the tariffs for other procedures. The tarrif for glaucoma surgery intervention in the UK is set by the department of health and is applied nationwide as a national tariff, as such a lack of knowledge by respondents may be expected as they have no influence on re-imbursement levels for specific interventions. However, different interventions attract different tarrifs and a better knowledge of tarrifs may lead to a change in pattern of surgical delivery resulting from an incentive to maximize income for a department either by choosing to undertake fewer high tariff (time consuming) procedures or many lower tarrif (less time consuming) procedures that increase subsequent income return.
A weakness of this study is the relatively poor response rate of 55% achieved. This is similar to the response rate of a previous UK wide survey on cyclodiode practise2 which achieved a response rate of 53.6%. While there is no suggestion that the response rate may reflect a response bias this cannot be ruled out. It is possible that the response rate may simply reflect that for consultants working in a busy and overstretched environment completion of a questionnaire on their surgical practise takes a low priority.
Several aspects of our survey could inform the future direction to glaucoma surgery. First, the fellows in this survey are more surgically versatile than established consultants with all undertaking both trabeculectomy and tube surgery and a high proportion using MIGS. This surgical versatility is a consequence of the opportunities that exist in fellowship training programmes where fellows can be taught these newer techniques in a safe environment under supervision of a trained and competent senior surgeon. This ‘safe environment’ training opportunity means that many departments will only acquire surgical versatility when these trainess are appointed as consultants. Many established consultants may be reluctant to learn new techniques in an unsupervised fashion and because they do not undertake a procedure may be unaware of the potential value of that procedure in their practice. Second, in stressed health care systems there may be a tendency to undertake surgery which generates the least follow-up burden and this would also be popular with patients. Third, hospital may only permit surgery where the tarrif covers the cost of surgery, and finally although not covered in this survey ease of surgery and surgery time may also be considered in this. If these factors are considered important, it would suggest a swing away from trabeculectomy surgery towards MIGS. Clearly, in the future years an evidence base supporting the efficacy and safety and optimum follow-up frequency requirements of newer interventions would be helpful is supporting this possible change.
This study provides a snap shot in time of current practice of glaucoma surgery in the UK. It gives perspective to current practice and provides a reference point for future comparisons. This study shows a wide variation in the types of glaucoma surgery undertaken, the indication for their use, the frequency with which they are undertaken and follow-up frequency variation. In future, more versatile surgery training with greater surgery options, pressure to minimize post-operative follow-up, consideration of tarrif value and further evidence of the safety and effectiveness of the newer glaucoma interventions may further change the spectrum of practice reported here.
Appendix A: Postoperative Regime for Glaucoma Surgery
- Select your grade of responsibility:
- Consultant
- Fellow
- Trainee
- Other (please specify)
- What types of glaucoma surgery do you routinely undertake? Please, choose more than one box if applicable.
- Trabeculectomy + MMC
- Tube implant: Baervedt
- Tube implant: Ahmed
- Tube implant: Molteno
- Non-penetrating deep sclerectomy
- Viscocanalostomy
- Viscocanaloplasty
- Minimally Invasive Glaucoma Surgery (MIGS): iStent®
- Minimally Invasive Glaucoma Surgery (MIGS): EX-PRESS®
- Minimally Invasive Glaucoma Surgery (MIGS): XEN®
- Other
- In general for POAG patients with advanced glaucoma requiring a low target IOP, which is your primary intervention?
Always Sometimes Never Trabeculectomy ◯ ◯ ◯ Tube ◯ ◯ ◯ Non-penetrating surgery ◯ ◯ ◯ MIGS ◯ ◯ ◯ - In general for patients with less advanced glaucoma requiring moderate target IOP, which is your primary intervention?
Always Sometimes Never Trabeculectomy ◯ ◯ ◯ Tube ◯ ◯ ◯ Non-penetrating surgery ◯ ◯ ◯ MIGS ◯ ◯ ◯ - What is your routine postoperative clinic follow-up following glaucoma surgery? Please answer for all types of surgery that you undertake (tick on as many boxes as you require).
Day 1 Day 3 Day 5 Week 1 Week 2 Week 3 Week 4 Week 5 Week 6 Month 2 Month 3 Month 4 Month 6 Trabeculectomy + MMC □ □ □ □ □ □ □ □ □ □ □ □ □ Tube implant: Baervedt □ □ □ □ □ □ □ □ □ □ □ □ □ Tube implant: Ahmed □ □ □ □ □ □ □ □ □ □ □ □ □ Tube implant: Molteno □ □ □ □ □ □ □ □ □ □ □ □ □ Non-penetrating deep sclerectomy □ □ □ □ □ □ □ □ □ □ □ □ □ Viscocanalostomy □ □ □ □ □ □ □ □ □ □ □ □ □ Viscocanaloplasty □ □ □ □ □ □ □ □ □ □ □ □ □ MIGS: iStent® □ □ □ □ □ □ □ □ □ □ □ □ □ MIGS: EX-PRESS □ □ □ □ □ □ □ □ □ □ □ □ □ MIGS: XEN® □ □ □ □ □ □ □ □ □ □ □ □ □ - Do you take the frequency of routine OPD follow up following surgery into consideration before deciding what surgery to undertake?
- Yes, always.
- Yes, most of times.
- Occasionally.
- No, roughly never.
- No, never.
- For your routine follow-ups, are they booked into a protected clinic slot or are they added on as extras to the clinic?
- They are always booked into a protected clinic slot.
- They are usually booked into a protected clinic slot.
- They are usually added on as extras to the clinic.
- They are always added on as extras to the clinic.
- I do not know.
- In your opinion, does the current HRG tariff cover the cost of surgery?
Yes No Don't know Trabeculectomy + MMC ○ ○ ○ Tube implant: Baervedt ○ ○ ○ Tube implant: Ahmed ○ ○ ○ Tube implant: Molteno ○ ○ ○ Non-penetrating deep sclerectomy ○ ○ ○ Viscocanalostomy ○ ○ ○ Viscocanaloplasty ○ ○ ○ MIGS: iStent® ○ ○ ○ MIGS: EX-PRESS ○ ○ ○ MIGS: XEN® ○ ○ ○ Other ○ ○ ○