The role of psychosocial factors and treatment need in dental service use and oral health among adults in Norway
Abstract
Objectives
This study aimed to explore whether population characteristics were associated with the use of dental services, individual's personal oral health practices, dental caries and oral health-related impacts using the revised Andersen's behavioural model as the theoretical framework.
Methods
This cross-sectional study included participants from a Norwegian general population (N = 1840; 20-79 years) included in the Tromstannen—Oral Health in Northern Norway (TOHNN) study. The variables included in the model were social structure (income, education, urbanization), sense of coherence (SOC), enabling resources (difficulties accessing the dentist, declined treatment, dental anxiety), treatment need, use of dental services, toothbrushing frequency, sugary soda drink consumption, decayed teeth and oral health-related impacts (OHIP-14). Structural equation modelling was used to test the direct and indirect effects within Andersen's behavioural model of access and health outcomes.
Results
Andersen's behavioural model fit the data well and explained a large part of the variance in use of dental services (58%), oral health-related impacts (48%) and, to a lesser extent, decayed teeth (12%). More social structures and a stronger SOC was associated with more enabling resources, which in turn, was associated with more use of dental services. Social structures were not directly associated with use of dental services or decayed teeth but were predictive of oral health-related impacts. A stronger SOC was associated with more frequent toothbrushing, less soda drink consumptions, fewer decayed teeth and less oral health-related impacts. Self-perceived need did not predict dental attendance but was associated with decayed teeth. A less frequent use of dental services, less frequent toothbrushing and more frequent sugary soda drink consumption were associated with more decayed teeth. Decayed teeth were not associated with oral health-related impacts.
Conclusion
The findings suggests that, in addition to focusing on reducing socioeconomic inequalities in relation to oral health in the Norwegian population, it is also important to consider how people perceive their own resources (eg financial, psychological, social) as well as their access to dental care in order to support regular dental attendance and potentially, in turn, enhance oral health.
1 INTRODUCTION
Regular dental attendance has been shown to have a positive impact on oral health.1, 2 Despite this, both access to oral health care and regular dental attendance have been shown to vary considerably within and between populations.3, 4 Why people do not regularly attend dental services is complex, and there is probably an interplay between psychosocial, material, cultural and behavioural aspects as well as the perceived need for treatment. Factors found to be associated with less use of dental health services are lower socioeconomic status (SES),4-6 dental fear,7-9 distant geographic location and distance to dental care services10, 11 and fatalistic beliefs.12
Understanding why people do not seek regular dental care is an essential requirement for developing effective health-policy interventions to reduce inequalities in oral health outcomes in any population. It is well known for example that dental attendance is related to dental caries.1, 13, 14 Dental caries is also a result of a complex interplay of other factors including an individual's behaviour, nutrition, SES, genetics and local oral environment.15 It is a diet-mediated disease and free sugars seems to be the primary determining factor.15 In addition, SES explains variations in dental caries between people. In a systematic review by Costa et al16 the authors found that an individual's educational level, income and/or occupation status were all associated with a greater prevalence of dental caries. In addition to SES indicators, psychological factors such as dental anxiety and sense of coherence are possible mediators of dental caries.7, 17 Sense of coherence (SOC) is a salutogenic construct relating to the way an individual makes sense of the world (comprehensibility), has the required resources to respond to life events (manageability) and feels that these responses are meaningful and make sense (meaningfulness).18 A stronger SOC has been associated with greater dental attendance, more frequent toothbrushing and fewer oral health-related impacts.19-22 The research to date would suggest that salutogenic factors—such as SOC—could play an important role in improving dental access and oral health-related behaviours and outcomes in adults.
To gain knowledge of the complex inter-relationship between the many determinants associated with the use of dental services, dental status and oral health impacts, biopsychosocial models have been shown to be useful tools to guide the selection of variables. One such theoretical model is Andersen's behavioural model for health services’ use.23, 24 Andersen23 originally developed the model to predict and explain why and how people use health care services by integrating predisposing/social structure factors (eg education, physical environment), enabling resources (eg having the means to use available health services) and need for health care (eg how people view their need for care). These different population characteristics have been used to explain why some people are more likely to seek health care. The model has, during the last three decades, been further extended and developed. Personal health practices and health outcomes/status (both self-perceived and clinically evaluated) have been added (Figure S1 in supporting information).24 The model has been tested to explore which factors determine dental care use and self-reported oral health in two different general populations in the UK.25, 26 Baker25 and Marshman et al26 found, in line with Andersen's model, that the impact of predisposing characteristics on treatment need and the use of dental services were mediated by enabling resources. That is, whilst there were individuals who were more predisposed to seek dental care, there had to be the means, meaning, the enabling resources for them to do so. Furthermore, in both studies, they found that people with higher perceived need were less likely to attend regular dental appointments and reported increased oral health impacts.
Andersen's behavioural model was recently utilized to explore how individual characteristics (psychosocial factors, enabling resources and treatment need) were associated with dental attendance, smoking habits, toothbrushing frequency, periodontitis and oral health-related impacts in a Norwegian adult population.27 In this study, SOC was also included in the model to examine key associations with adults’ oral health as well as other key determinants. In line with the two previous UK studies,25, 26 the relationship between predisposing characteristics (income, education and urbanization) and use of dental services was mediated by enabling resources. In contrast, however, need was not associated with use of dental services or oral health impacts. Instead, SOC, predisposing characteristics and the severity of periodontitis were the main predictors of oral health-related impacts. Severity of periodontitis was linked to smoking and predisposing characteristics (eg income).
In order to further extend our understanding of the oral health of the Norwegian population, in particular, the association of key individual characteristics with the use of dental services and oral health impacts, the present study utilized Andersen's behavioural model with dental caries as the clinically evaluated outcome. In addition, the frequency of soda drink consumption—as a behavioural factor commonly associated with dental caries—was examined.
As discussed by Costa et al16 in their recent systematic review, the majority of previous research on the socioeconomic factors related to dental caries have employed bivariate and/or multivariate analysis including a handful of factors whilst controlling for potential confounders. Yet, given the complex range of clinical, psychological and social factors important in dental caries, it is necessary to study the inter-relationships between all of these potential factors at the same time.28 Currently, one way to explore the inter-relationship between several contributing factors simultaneously is to apply theoretically driven structural equation modelling (SEM). The aim of the present study therefore was to employ SEM to examine how population characteristics (predisposing factors; enabling resources; perceived need) were associated with the use of dental services, oral health practices, dental caries and self-reported oral health impacts using Andersen's behavioural model for health services’ use as the theoretical framework.
2 METHODS
2.1 Study design and participants
Andersen's behavioural model was tested in a general adult population with data from the Tromstannen —Oral Health in Northern Norway (TOHNN) study utilizing dental caries (decayed teeth) as the clinical outcome.29 The TOHNN-study was a cross-sectional study in an adult population in Troms County.29 Details of the invitation procedure have been described in a previous publication.29 In brief, a randomly selected sample of 3,000 individuals was drawn from the 112 253 20-79 year-olds residing in Troms County in January 2013 by Statistics Norway. The sample size was based on a hypothesized 10% prevalence of severe periodontitis with a 95% confidence level and margin of error of 1.5%, accounting for a response rate of about 50%. A letter of invitation was sent by mail to 2901 persons (the remaining 91 persons had either moved out of the county or were deceased). Of those invited, 1986 individuals agreed to participate in the study, completing a dental examination and questionnaire. In this secondary analysis, all edentulous individuals were excluded (50 individuals) and participants with extensive missing data (see statistical analysis). Dental examinations were performed in five different dental offices by 11 examiner teams (dentist with assistant nurse). Data were collected between October 2013 and November 2014. The study was approved by the regional committee for medical and health research ethics of UiT the Arctic University of Norway (2013/348/REC North).
2.2 Measures
The variables in the study were chosen to reflect the constructs in Andersen's revised behavioural model24 and with reference to the findings of two previous studies that tested the model in relation to oral health.25, 26 Nine constructs comprising 18 different variables were included in the model of which 14 variables were represented by five latent variables. Table S1 in the supplementary materials details each construct, together with its operationalization and associated measure(s). In summary:
Predisposing characteristics were measured with two latent variables: social structures and SOC. The three measured (indicator) variables for social structures were education, annual household income and urbanization. Education was categorized as middle school, high school or university level. For income, there were four categories; (a) <300 000 NOK, (b) 300 001-450 000 NOK, (c) 450 001-900 000 NOK and (d) >900 000 NOK. Urbanization was used as an indicator of the number of inhabitants and availability of dentists as a ratio of inhabitants per dentist. The municipality with the larger town had the highest dentist availability and was categorized as urban; two municipalities with smaller towns had the second highest availability and were categorized as suburban; and the remaining municipalities without towns and with lowest availability were classified as rural. The second latent variable, SOC, was assessed with the Norwegian version of the previously validated ‘Orientation to life questionnaire’, which is comprised of 13 items.30, 31 Indicator variables were represented by the three SOC dimensions: comprehensibility (five items), manageability (four items) and meaningfulness (four items).
Enabling resources were measured with one latent variable. The three indicators for this latent variable were declined treatment due to costs, perceived difficulty accessing a dentist (each assessed with one question), and dental anxiety. Dental anxiety was assessed with the previously validated Norwegian version of Corah's Dental Anxiety Scale (DAS).32, 33 For analysis, the DAS-score was reversed so higher scores represented less dental anxiety.
Treatment need within the model was assessed with one observed variable: “If you saw a dentist tomorrow, do you think you would need treatment’? (yes/no)”.
Oral health-related behaviours were represented by personal oral health practices and use of dental services. Personal oral health practices included frequency of toothbrushing and of sugary soda drink consumption. Each of these was measured with one item (observed variables). Use of dental services was measured as a latent variable with two indicators: attendance orientation and frequency of attendance. The response options for these, and all variables, can be seen in Table 1.
| Variable | N/Mean | %/SD | Min-max |
|---|---|---|---|
| Predisposing factors | |||
| Social Structure (Latent variable) | |||
| Education | |||
| Secondary/middle school | 254 | 13.8 | |
| High school | 813 | 44.2 | |
| University | 773 | 42.0 | |
| Income (household annually) | |||
| NOK ≤ 300 000 | 254 | 13.8 | |
| NOK > 300 001-450 000 | 276 | 15.0 | |
| NOK > 450 001-900 000 | 948 | 51.5 | |
| NOK > 900 000 | 362 | 19.7 | |
| Urbanization (Availability to dentists) | |||
| Rural | 432 | 23.5 | |
| Suburban (small towns) | 572 | 31.1 | |
| Urban (larger town) | 836 | 45.4 | |
| Salutogenic Resources | |||
| Sense of Coherence (SOC) (Latent variable) | 68.6 | 10.5 | 25-90 |
| Comprehensibility | 25.5 | 4.8 | 5-35 |
| Manageability | 20.9 | 3.8 | 4-28 |
| Meaningfulness | 22.1 | 3.6 | 8-28 |
| Enabling resources (Latent variable) | |||
| Refrained from dental check-up due to lack of money | |||
| Yes | 358 | 19.5 | |
| No | 1482 | 80.5 | |
| Difficult accessing routine care | |||
| Yes/ Don't know | 319 | 17.3 | |
| No | 1521 | 82.7 | |
| Dental Anxiety Scale* | 16.3 | 3.3 | 4-20 |
| Need (Observed variable) | |||
| Self-perceived treatment need | |||
| Would not need treatment | 469 | 25.5 | |
| Don't know | 702 | 38.2 | |
| Would need treatment | 669 | 36.4 | |
| Oral health-related behaviours | |||
| Toothbrushing | |||
| Less than once a day | 70 | 3.8 | |
| Once a day | 442 | 24.0 | |
| Twice a day | 1328 | 72.2 | |
| Frequency of sugary soda drink intake (Observed variable) | |||
| Seldom | 1094 | 59.5 | |
| A few times every week | 650 | 35.3 | |
| Several times a week to daily | 96 | 5.2 | |
| Use of dental health services (Latent variable) | |||
| Reason for attending dentist | |||
| Do not attend/attend seldom | 284 | 15.4 | |
| When problem (pain, lost fillings) | 367 | 19.9 | |
| Having routine recall/check-up | 1189 | 64.6 | |
| Attendance to dental health care services | |||
| Only when having problems | 412 | 22.4 | |
| Longer intervals than 2 y | 204 | 11.1 | |
| Every second year | 246 | 13.4 | |
| Every year | 978 | 53.2 | |
| Oral health outcomes | |||
| Clinically evaluated outcome | |||
| Number of decayed teeth (Observed variable) | 1.1 | 1.7 | 0-13 |
| Person-reported oral health-related impacts | |||
| OHIP-14 (Latent variable) | 19.4 | 6.54 | 14-70 |
| OHIP physical | 8.7 | 2.9 | 6-30 |
| OHIP psychological | 6.0 | 2.9 | 4-20 |
| OHIP social | 4.7 | 1.8 | 4-20 |
- * For comparison to other studies where higher scores represent more dental anxiety, the mean score for this population was 7.7.
The clinically evaluated outcome, dental caries, was measured with one observed variable: number of decayed teeth. Decayed teeth was radiographically and clinically assessed for all tooth surfaces in all teeth, except third molars, using four bite-wing radiographs and a dental explorer (Hu-Friedy EXS9), mouth mirror and compressed air. Decayed teeth were recorded on a five-grade diagnostic scale.34 In this grading scale, caries Grades 1-2 are denoted as enamel caries and Grades 3-5 as dentine caries. In this study, teeth with only enamel lesions (Grades 1-2) were defined as healthy. Teeth with dentine caries (Grade 3-5) were defined as decayed, independently of severity. Two calibration tests were conducted during the study period with a 3-month interval. A set of bite-wing radiographs was examined by all examiners, and congruency towards the gold standard using proportion of agreement and Cohen's kappa (κ) was evaluated with an acceptable agreement (per cent agreement: 75%-100% and 81%-92%, respectively; median κ-values: 0.73 and 0.77, with quartile deviations between 0.5-0.85 and 0.74-0.79, respectively).29 For more information on the distribution of caries and caries experience for this Norwegian population sample see Oscarson et al.35
Subjective oral health-related impacts were measured as a latent variable and assessed by using the short-form of the previously validated Norwegian version of the Oral Health Impact Profile (OHIP-14).36, 37 Cronbach's Alpha for OHIP-14 was 0.89. In line with similar SEM studies using the OHIP-14,25 the scale was represented in the model as a latent variable with the three sub-scales—psychological, physical and social impacts—as indicator variables. Cronbach's Alpha for physical function was 0.73, psychological function 0.89 and social function 0.88, respectively.
2.3 Data analysis
In order to assure the estimated minimum sample size for the structural equation model, a power calculation was conducted with an effect size of 0.1, power of 0.8, five latent variables, four observed variables and a probability set at .05. The minimum sample size needed was 1599 participants.
IBM® SPSS® Statistics, Version 24 and AMOS 24 were used for the data analysis. Missing data occurred at a very low frequency (0%-5.8%) with the exception of sugary soda drink consumption (8.2%). An analysis of missing data patterns, computed by SPSS, showed that missing values appeared to be at random and at a low rate (1.9% of the total values used in the present analysis). Missing variables were replaced as follows: All one-item variables were replaced with the median. Individuals with more than three missing SOC items were excluded from analysis. If three or fewer items were missing, they were replaced by the median value of the remaining SOC items for that individual.38 Individuals with more than two missing OHIP-items were excluded from analysis. When two or less items were missing, they were replaced with the sample median of the relevant OHIP-item.39 Individuals with more than one missing item in the DAS-scale were excluded from analysis. Single missing items were replaced with the median value of the remaining DAS items for that individual. Re-analysis of data excluding individuals with any missing items did not change mean scores by more than two decimal places or frequency distributions by more than one percentage point, except for income and soda drink consumption that changed 2.4 and 3.4 percentage points, respectively (not reported). The excluded individuals did not differ significantly on key outcomes (decayed teeth and OHIP-14 sum mean score) compared with those that remained in the analysis.
In Step 1 of the analysis, to identify whether the indicators chosen to measure the five latent constructs were acceptable, confirmatory factor analysis (CFA) was used. CFA is the first in the two-stage process of SEM (the measurement model).40 CFA provides information on how indicator items (eg income, education, urbanization) measure underlying (latent) constructs (eg social structures). The initial step of the analysis was to test a first order CFA with social structures, SOC, enabling resources, attendance and oral health impacts (OHIP14) as the five latent constructs. Scale items (indicators) representing each of the five latent constructs are detailed in Table 1. Items were not allowed to load on more than one construct nor were error terms allowed to correlate, with the exception of the three domains of the SOC construct.
In Step 2 of the analysis, structural equation modelling (SEM) was used to examine the direct and indirect relationships between the constructs as hypothesized in our revised Andersen's behavioural model. In accordance with the model and with SOC as an additional predisposing factor based on findings by Gupta et al,41 24 direct pathways were hypothesized (Figure S2 in supporting information). It was hypothesized that predisposing characteristics; more of social structures and stronger SOC would predict more enabling resources, both predisposing and enabling would predict need (more resources would relate to less perceived treatment need). Predisposing, enabling and need would predict use of dental services and toothbrushing and soda drink consumption (more predisposing and enabling resources and less treatment need would be associated with more frequent dental attendance and more favourable health behaviour), which would, in turn, predict decayed teeth and oral health-related impacts. Decayed teeth would predict oral health impacts, with more decayed teeth relating to more oral health-related impacts. In addition, predisposing, enabling and need would predict decayed teeth and oral health impacts.
AMOS estimates the total effects, made up of both direct effects (a path directly from one variable to another, eg social structure→enabling) and indirect effects (a path mediated through other variables, eg social structure→need via enabling resources). Because of the presence of both non-normal and categorical data, the model was estimated using bootstrapping wherein multiple samples (n = 900+) are randomly drawn from the original sample; the CFA model is then estimated in each data set, and the results averaged. The ML bootstrap estimates and standard errors [together with bias-corrected 95% confidence intervals (CIs)] are then compared with the results from the original sample to examine stability of parameters and test statistics.42
As recommended, model fit was evaluated using a range of indices from the three fit classes; absolute, parsimony adjusted and comparative. A χ2/df ratio of <3.0, RMSEA values <0.06, CFI and TLI of 0.9 or above and an SRMR <0.08 were taken to indicate an acceptable model fit.42, 43
3 RESULTS
In the final analysis, 1840 participants (934 women, mean age 47.2 ± 15.3 years) were included. Regarding number of decayed teeth, 971 participants (52.8%) had none, 600 (32.6%) had one or two and 269 (14.6%) had three or more. The median value for decayed teeth was 0 (1st quartiles = 0, 3rd = 2). There was a correlation between OHIP-14 mean scores and mean number of decayed teeth (r = .215, P < .01): participants with a greater number of decayed teeth reported more oral health-related impacts. Proportions, mean values and range for each variable used in the model are presented in Table 1.
The indicators chosen to measure the five latent constructs were an acceptable fit on four of the five a priori indices (χ2 ⁄ df 4.659 (P < .001); RMSEA: 0.043 (90% CI: 0.039-0.048); CFI: 0.971; TLI: 0.959, SRMR: 0.034). The CFA can be seen in Figure S3 in supporting information with the factors (latent variables) shown in ellipses, items (indicator variables) in rectangles and residual error terms in circles. All item loadings were significant (<0.001) and in the expected direction. The correlations between the five latent factors ranged between −0.53 and 0.70, indicating an acceptable discriminant validity (ie <0.85).
The revised Andersen's behavioural model was an acceptable fit to the data meeting four of the five a priori criteria (χ2 ⁄ df 5.427 (P < .001); RMSEA: 0.049 (90% CI: 0.045-0.053); CFI: 0.944; TLI: 0.923, SRMR: 0.051). Seven of the hypothesized bootstrapped paths were nonsignificant (Table 2). In this model, 53%, 27%, 58%, 12% and 48% of the bootstrapped variance was accounted for in enabling resources, need, use of dental services, number of decayed teeth and oral health-related impacts, respectively (Figure 1).
| Effect | β | Bootstrap SE | Bias-corrected 95% CI | P |
|---|---|---|---|---|
| Direct effects | ||||
| Social structure – enabling | 0.198 | 0.056 | 0.085/0.307 | .002 |
| SOC - enabling | 0.699 | 0.065 | 0.573/0.837 | .001 |
| Enabling – need | −0.518 | 0.024 | −0.565/−0.465 | .003 |
| Need - DCS use | −0.068 | 0.037 | −0.113/0.008 | .077 |
| DCS use – toothbrushing | 0.112 | 0.030 | 0.051/0.166 | .002 |
| DCS use – sugary soda drinks | −0.093 | 0.030 | −0.149/−0.031 | .005 |
| DCS use – decayed teeth | −0.115 | 0.032 | −0.181/−0.056 | .001 |
| DCS use – oral health impacts | 0.017 | 0.044 | −0.063/0.112 | .635 |
| Toothbrushing – decayed teeth | −0.102 | 0.029 | −0.156/−0.044 | .004 |
| Sugary soda drinks – decayed teeth | 0.083 | 0.027 | 0.027/0.136 | .001 |
| Decayed teeth - oral health impacts | 0.056 | 0.038 | −0.017/0.113 | .135 |
| Social structure - DCS use | −0.057 | 0.053 | −0.175/0.031 | .213 |
| Social structure – toothbrushing | 0.264 | 0.037 | 0.190/0.336 | .001 |
| Social structure – sugary soda drinks | −0.057 | 0.037 | −0.131/0.016 | .116 |
| Social structure – decayed teeth | −0.062 | 0.040 | −0.136/0.024 | .138 |
| Social structure – oral health impacts | −0.186 | 0.040 | −0.265/−0.108 | .001 |
| SOC – DCS use | −0.412 | 0.150 | 0.764/−0.222 | .001 |
| SOC – toothbrushing | 0.098 | 0.042 | 0.021/0.179 | .018 |
| SOC – sugary soda drinks | −0.160 | 0.041 | −0.235/−0.080 | .003 |
| SOC – decayed teeth | −0.121 | 0.055 | −0.242/−0.016 | .017 |
| SOC – oral health impacts | −0.634 | 0.060 | −0.757/−0.517 | .001 |
| Enabling – DCS use | 0.963 | 0.152 | 0.764/1.372 | .002 |
| Need – decayed teeth | 0.123 | 0.028 | 0.064/0.172 | .002 |
| Need – oral health impacts | 0.054 | 0.037 | −0.020/0.129 | .121 |
| Indirect effects | ||||
| Social structure - need | −0.102 | 0.030 | −0.162/−0.045 | .002 |
| Social structure – DCS use | 0.197 | 0.064 | 0.088/0.340 | .002 |
| Social structure – toothbrushing | 0.016 | 0.006 | 0.007/0.033 | .002 |
| Social structure – sugary soda drinks | −0.013 | 0.006 | −0.028/−0.005 | .003 |
| Social structure – decayed teeth | −0.063 | 0.013 | −0.093/−0.041 | .001 |
| Social structure – oral health impacts | −0.010 | 0.010 | −0.032/0.007 | .253 |
| SOC – need | −0.362 | 0.039 | −0.446/−0.292 | .001 |
| SOC – DCS use | 0.698 | 0.162 | 0.479/1.186 | .001 |
| SOC – toothbrushing | 0.032 | 0.010 | 0.015/0.059 | .001 |
| SOC – sugary soda drinks | −0.027 | 0.009 | −0.049/−0.011 | .002 |
| SOC – decayed teeth | −0.106 | 0.015 | −0.140/−0.080 | .001 |
| SOC - oral health impacts | −0.027 | 0.019 | −0.056/0.016 | .179 |
| Enabling – DCS use | 0.035 | 0.018 | −0.004/0.067 | .079 |
| Enabling – toothbrushing | 0.112 | 0.035 | 0.053/0.192 | .001 |
| Enabling – sugary soda drinks | −0.093 | 0.031 | −0.158/−0.031 | .005 |
| Enabling – decayed teeth | −0.198 | 0.035 | −0.274/−0.113 | .001 |
| Enabling - oral health impacts | −0.022 | 0.051 | −0.110/0.088 | .684 |
| Need – toothbrushing | −0.008 | 0.005 | −0.019/0.000 | .052 |
| Need – sugary soda drinks | 0.006 | 0.004 | 0.000/0.016 | .048 |
| Need – decayed teeth | 0.009 | 0.005 | 0.000/0.022 | .047 |
| Need - oral health impacts | 0.006 | 0.007 | −0.006/0.021 | .304 |
| DCS use – decayed teeth | −0.019 | 0.006 | −0.033/−0.008 | .002 |
| DCS use – oral health impacts | −0.008 | 0.006 | −0.021/0.021 | .095 |
Note
- Significant pathways in bold.
- Abbreviations: β, bootstrapped standardized estimate; CI, confidence interval; DCS, dental care services; SE, standard error; SOC, sense of coherence.
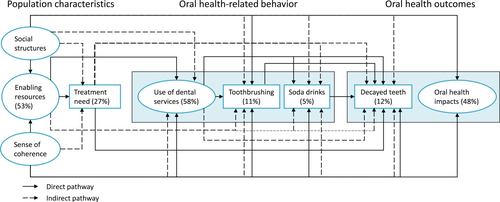
The direct effects can be seen in Table 2 and Figure 1. As hypothesized, more of the predisposing social structures and a stronger SOC were linked to more enabling resources. More of the enabling resources were, in turn, linked to less perceived treatment need and a greater use of dental services. A greater use of dental services was linked to more frequent toothbrushing, less sugary soda drink consumption and fewer decayed teeth. Less frequent toothbrushing and more frequent sugary soda drink consumption were associated with a greater number of decayed teeth. In addition, more social structures were linked to more frequent toothbrushing and fewer oral health-related impacts (lower OHIP-14 scores). Stronger SOC was linked to less use of dental services, more frequent toothbrushing, less frequent sugary soda drink consumption, fewer decayed teeth and fewer oral health-related impacts. As hypothesized, more perceived treatment need was linked to more decayed teeth.
There were sixteen significant indirect paths (Table 2 and Figure 1). More social structures were associated with less treatment need, more use of dental services, more frequent toothbrushing, less sugary soda drink consumption and fewer decayed teeth. A stronger SOC was associated with less treatment need, more use of dental services, more frequent toothbrushing, less sugary soda drink consumption and fewer decayed teeth. More enabling resources were linked to more frequent toothbrushing, less sugary soda drink consumption and fewer decayed teeth. More treatment need was linked to more sugary soda drink consumption and more decayed teeth. Finally, more use of dental services was linked to fewer decayed teeth. These are total indirect paths and can consist of a single potential effect or a multitude of potential effects. For example, greater social structures were linked to a greater perceived treatment need via a single effect: more enabling resources. On the other hand, more social structures were linked to fewer decayed teeth via two effects: more enabling resources and greater use of dental services.
4 DISCUSSION
In the present study, we found support for Andersen's behavioural model of access and health outcomes when applied to the oral health of a Norwegian adult general population sample. These findings therefore lend further support to the use of this as a conceptual framework for understanding the key determinants for dental health service use, self-reported oral health impacts and tooth decay in adults.
The findings regarding use of dental services were in line with our previous analysis testing Andersen's behavioural model with periodontitis as the clinically evaluated outcome.27 In relation to both tooth decay and periodontitis, enabling resources seemed to be a key factor associated with regular dental attendance. Those people without dental anxiety, who perceived no or few economic or practical difficulties accessing dental care were more likely to visit the dentist regularly regardless of educational level, household income or indeed the availability of dentists (ie social structures). In the present analysis, we found that these social structures were mediated through enabling resources suggesting that having a lower socioeconomic status does not necessarily mean that people do not attend dental services regularly. This is in contrast to previous studies4-6 but supports the findings by Grytten et al44 who found that income had little impact on the use of dental services in a Norwegian population; despite people in Norway having to pay almost all dental treatment costs themselves.
When comparing our results to findings from two studies with British populations25, 26 both with a similar study design and using similar constructs from Andersen's behavioural model, the main difference appeared to be that in the Norwegian population, perceived treatment need was not associated with use of dental services. Instead, the use of dental services appeared to be linked to factors other than people's perceived need. These results support key hypotheses in Andersen's model24; namely, that dental care is more likely to be associated with social structures (eg income, availability of services) and enabling factors (eg dental anxiety) rather than to needs. However, it is important to bear in mind that how participants in this study understood the term ‘treatment’ could have had an impact on the results. This was because the question was not specific to dental caries treatment need per se but rather a generic question about dental treatment. Nevertheless, the present findings do highlight the importance for dental professionals to explore how their patients experience dental care visits, what they perceive as obstacles as well as enabling factors in order to help facilitate regular dental attendance. In this regard, previous studies have suggested that action planning and coping planning can increase dental attendance rates45 and brief Motivational Interviewing may be a useful method to reduce avoidance to dental care when contacting patients.46
As this was the first study to use dental caries as the clinically evaluated outcome in Andersen's behavioural model, comparison to other studies was not possible. The relatively small amount of variance in the decayed teeth outcome measure explained by the model could be expected since other well-known factors associated with dental caries (eg fluoride supplement, diet) were not included in the current analysis. Unexpectedly, however, social structures (education, income, urbanization) were not directly associated with decayed teeth as has been previously reported in many cross-sectional studies.16 Rather, in a population with a relatively high educational level, socioeconomic factors appeared to be linked to tooth decay through people's enabling resources (dental anxiety, treatment costs, access to dental services) or increased toothbrushing frequency. One interesting difference between the present analysis and our previous research20 was that here regular dental attendance was associated with less disease—that is fewer decayed teeth whilst in relation to periodontitis, more frequent use of dental services was associated with higher likelihood of having periodontitis. As expected, less frequent toothbrushing and more sugary soda drink consumption were associated with decayed teeth. Furthermore, there seemed not only to be a direct relationship between SOC and number of decayed teeth, SOC also appeared to be linked to oral health-related behaviour, which in turn predicted dental caries, as has been suggested in previous studies.19, 47
Number of decayed teeth was not associated with impaired oral health-related quality of life, in contrast to findings from other studies.48-50 The studies are however, not directly comparable due to age differences between study populations. Also, in the present study several factors were analysed simultaneously in an a priori theoretical model and variables that were correlated in bivariate analysis were no longer associated when all other variables were added. When all variables were tested together, lower education, lower income and low availability to dentists were associated with impaired oral health-related quality of life. In our study, SOC was the factor with the strongest association to self-reported oral impacts. This adds to existing literature on the important role of SOC, as a key psychosocial factor, associated with oral health practices and oral health outcomes.19, 22 Interestingly, a strong SOC was directly associated with less use of dental services but to more use when mediated through enabling resources. It is difficult to interpret such contrary findings from the present cross-sectional data; in order to understand the pathway from SOC to health service use, longitudinal studies are now needed. This would, in turn, add to the literature on the effectiveness of a salutogenic approach—based on enhancing SOC—to oral health promotion.51
Although the study has reported interesting findings on the key predictors associated with dental caries in this Norwegian adult population and is the first to examine these predictors simultaneously based on a theoretical model, there are a number of limitations that should be noted. The most important limitation is the cross-sectional study design. As all variables were measured at the same point in time, the present analysis does not attempt to identify cause and effect relationships but was rather an exploratory theory-driven analysis that aimed to examine the complex relationship between several contributing factors. Whilst the level of decayed teeth in the current sample was comparable to reports from European and US studies,52-54 findings regarding use of dental services should be cautiously extrapolated to other regions and countries, as the structure of dental services might only apply for this Norwegian region. The possible impact of non-responses should also be considered. Nonresponders were somewhat older (mean age 51.4 ± 16.6 years) and comprised a higher proportion of men (54%) compared to participants included in the analysis (49%).29 Under-representation of older adults could affect the generalization to the older population in Troms County. Participants also had a higher level of education compared with countywide estimates, indicating an over-representation of persons with a higher education level. Despite these limitations, the proposed model can be considered a good contribution to the understanding of not only which socioeconomics and psychosocial factors predict use of dental services, having decayed teeth and oral health-related impacts but also how different factors are related by assessing these with complex statistical methods that allow for testing of both direct and indirect effects. Interestingly, the proportion of irregular dental attendees was higher compared to previous reports of dental attendance in Norway,44, 55 indicating that people who do not use dental health services regularly is not underrepresented. This can be considered a strength of the study when exploring use of dental services in the Norwegian population.
In conclusion, the findings suggests that, in addition to focusing on reducing socioeconomic inequalities in relation to oral health in the Norwegian population, it is also important to consider how people perceive their own resources (eg financial, psychological, social) as well as their access to dental care in order to support regular dental attendance and potentially, in turn, enhance oral health.
ACKNOWLEDGEMENTS
Thanks to Dr Nils Oscarson and Dr Anders Tillberg who together with the first and second author carried out the TOHNN-study. Thanks to all dental teams at the public dental clinics for helping with the data collection. The TOHNN study was funded by the Troms County Council and The Norwegian Directorate of Health. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
CONFLICT OF INTERESTS
The authors have stated explicitly that there are no conflicts of interest in connection with this article.
AUTHOR CONTRIBUTIONS
All authors have made substantial contributions to conception and design of the study. BJ and GEH planned and did the data collection. All authors have been involved in data analysis and interpretation, drafting the manuscript and revising it critically and have given final approval of the version to be published.