Diagnostic potential of TERT promoter and FGFR3 mutations in urinary cell-free DNA in upper tract urothelial carcinoma
Abstract
Most upper tract urothelial carcinomas (UTUC) are muscle invasive at the time of diagnosis. Current standard methods for the diagnosis of UTUC are invasive. Urine cytology is the only non-invasive test for detecting UTUC, but its sensitivity is low. A novel non-invasive assay for UTUC detection would improve patient outcome. This study aimed to investigate the mutation of cell-free DNA (cfDNA) in urine supernatant to develop a reliable diagnostic biomarker for UTUC patients. We studied urinary cfDNA from 153 individuals, including 56 patients with localized UTUC, and carried out droplet digital PCR assay for TERT promoter and FGFR3 hotspot mutations. We could detect mutations of TERT C228T in 22/56 (39.3%), TERT C250T in 4/56 (7.1%), and FGFR3 S249C in 9/56 (16.1%) patients. FGFR3 mutation was detected only in ≤pT1 tumors (positive predictive value: 100.0%). In combination with cytology results, the sensitivity was 78.6%, and the specificity was 96.0%. Although these data need to be validated in a larger-scale cohort, mutation analysis of TERT promoter and FGFR3 in urinary cfDNA has the potential to be a non-invasive diagnostic marker and reliable factor for tumor staging.
Abbreviations
-
- cfDNA
-
- cell-free DNA
-
- CI
-
- confidence interval
-
- ctDNA
-
- cell-free tumor DNA
-
- ddPCR
-
- droplet digital polymerase chain reaction
-
- FFPE
-
- formalin-fixed paraffin-embedded
-
- FGFR
-
- fibroblast growth factor receptor
-
- HR
-
- hazard ratio
-
- MAF
-
- mutant allele frequency
-
- NGS
-
- next-generation sequencing
-
- NMIBC
-
- non-muscle-invasive bladder cancer
-
- NPV
-
- negative predictive value
-
- OR
-
- odds ratio
-
- PPV
-
- positive predictive value
-
- RNU
-
- radical nephroureterectomy
-
- TERT
-
- telomerase reverse transcriptase
-
- TURBT
-
- transurethral resection of bladder tumor
-
- UBC
-
- urothelial bladder cancer
-
- UC
-
- urothelial carcinoma
-
- UTUC
-
- upper tract urothelial carcinoma
1 INTRODUCTION
Upper tract urothelial carcinoma arising from the renal pelvis or ureter is a relatively uncommon malignancy, accounting for 5% of UC.1 Fifty-five to fifty-nine percent of UTUC are muscle invasive at the time of diagnosis.2, 3 Patients suspected of having UTUC need to receive invasive procedures such as computed tomography (CT) urography, retrograde pyelography, or ureteroscopy for a definitive diagnosis. Many researchers have tried to develop useful urinary markers to detect UTUC,4, 5 but urine cytology still remains the only non-invasive diagnostic marker recommended by many guidelines6, 7 although its sensitivity for detection of UTUC is as low as 40%.8
Cell-free DNA in bodily fluids has huge potential in disease diagnosis.9-11 Cell-free tumor DNA is shed into the urine or circulation along with DNA from normal cells. Even though ctDNA constitutes a small fraction of the total DNA, ctDNA is thought to be a promising diagnostic biomarker. Christensen et al12 reported the prognostic utility of urinary and plasma ctDNA extracted from patients with UBC.
Next-generation sequencing has shown genomic alterations and transcriptional subtypes in UTUC and UBC tissue.13-16 Hotspot mutations of TERT promoter and FGFR3 (S249C) are frequently identified in UTUC specimens. Mutations in the upstream promoter of the TERT gene predominantly affect two hotspots, g.1295228 C>T and g.1295250 C>T,17, 18 hereafter referred to as C228T and C250T, respectively. The mutant TERT promoter allele alters the binding site, recruits transcription factor GABPA, and engages in long-range chromatin interactions, subsequently stimulating increased TERT promoter activity and enabling tumors to overcome the end-replication problem and avoid senescence.19-21 Springer et al16 reported the clinical potential of mutant DNA derived from urinary cells (pellets) by targeted sequencing in patients with UBC or UTUC for cancer detection and surveillance. In UBC patients, urinary cfDNA has a higher tumor genomic burden and greater detection potential as a genomic biomarker than urinary pellets.22 To our knowledge, there is no research on the relationship between urinary cfDNA alteration of UTUC and clinical utility. In the present study, we developed ddPCR assays for the detection of hotspot mutations of the TERT promoter region and FGFR3 and analyzed the diagnostic potential of urine supernatant cfDNA collected from patients with localized UTUC.
2 MATERIALS AND METHODS
2.1 Urine samples
We investigated voided urine samples from four cohorts of patients: those with localized UTUC (UTUC cohort); those with microscopic or macroscopic hematuria without UC (hematuria cohort); those who were treated with TURBT or RNU and had no evidence of disease recurrence for at least 1 year (UC surveillance cohort); and a healthy control cohort (HC cohort) that included kidney transplantation donors, healthy volunteers, benign disease patients (ie, benign prostate hyperplasia or acute cystitis), and patients with urological carcinoma other than UC. All patients were treated at Osaka University Hospital, Osaka General Medical Center, or Osaka Police Hospital from 2013 to 2019. All patients provided written informed consent, and the study was approved by the appropriate ethics committee. All patients in the UTUC cohort were histologically diagnosed as having UC, and urine samples were collected from patients within 4 days before RNU or transurethral biopsy. We excluded UTUC patients with concurrent bladder cancer. In 12 of the patients in the UTUC cohort, post-treatment urine samples were also collected approximately 1 week after RNU.
2.2 Pathological diagnosis
Histological diagnosis was determined by experienced pathologists. Tumor stage and grade were determined according to the 8th edition of the AJCC stage classification,23 and tumors were graded according to the World Health Organization 2016 criteria.24 Urine cytology was also evaluated by specialists according to our institutional criteria, in which negative urine cytology is defined to be no more than class III and positive urine cytology to be class IV and class V. We used the highest urine cytology class for data analysis if patients received several cytology tests before treatment.
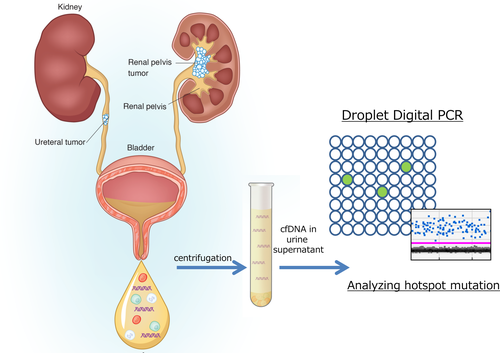
2.3 Urinary cfDNA purification
After collection from the patients, urine was centrifuged at 2000 g for 30 minutes, and urine supernatants were stored at −80°C. Urine was thawed in a water bath at 27°C, and 4-32 mL (median: 12 mL) supernatants was used for cfDNA purification after centrifugation at 16 000 g for 10 minutes. Urinary cfDNA extraction was carried out with a QIAamp Circulating Nucleic Acid Kit (QIAGEN, Hilden, Germany) according to the manufacturer's protocol, and cfDNAs were eluted by 50 μL AVE buffer. DNA concentration was measured by a Qubit dsDNA High Sensitivity Assay Kit (Thermo Fisher Scientific, Waltham, MA, USA).
2.4 Droplet digital PCR assay
For mutation detection, we used the ddPCR platform QX100 Droplet Digital PCR System (Bio-Rad Laboratories, Hercules, CA, USA), including primers and probes (FAM, mutant type; HEX, wild type), and ddPCR Supermix for Probes (No dUTP) according to the manufacturer's protocol. For every experiment, we used a positive control corresponding to each mutation. Primers and probes for ddPCR were TERT promoters C228T/C250T, FGFR3 S249C, and PIK3CA E545K (S1). Droplets were generated using a droplet generator (Bio-Rad Laboratories). The PCR cycle for FGFR3 included a 10-minute incubation at 95°C followed by 40 cycles at 94°C for 30 seconds and at 55°C for 1 minute, one cycle at 98°C for 10 minutes, and a 12°C hold; and that for the TERT promoter included a 10-minute incubation at 95°C followed by 50 cycles at 94°C for 30 seconds and at 55°C for 1 minute, one cycle at 98°C for 10 minutes, and a 12°C hold. We used 5.7 ng (range: 1.5-30.7 ng) of urinary cfDNA for each ddPCR analysis. Droplet fluorescence was assessed in a droplet reader. Analysis of ddPCR data for allele calling and calculation of absolute copy numbers were done using QuantaSoft software version 1.7.4 (Bio-Rad Laboratories). The samples were considered positive for targeted mutations when they met two criteria: (i) they contained at least three droplets in the positive area of the FAM signal; and (ii) the MAF was >0.1%. MAF was defined as the proportion of copies of the mutant type relative to the sum of copies of the mutant and wild type obtained by the ddPCR platform.
2.5 Statistical analysis
Statistical analysis was carried out using JMP Pro 14.0.0 (SAS Institute Inc., Cary, NC, USA). Patient characteristics were compared using the Mann-Whitney U test. Multiple regression analyses were done to assess the relative contributions of factors (age, gender and urine cytology) and the mutations in cfDNA. Differences were considered statistically significant when P < 0.05.
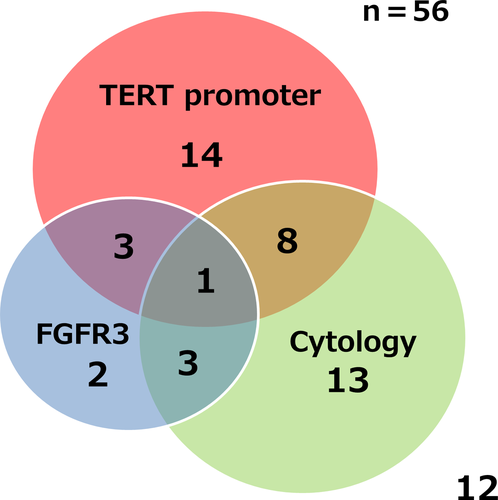
3 RESULTS
Table 1 shows the clinical characteristics and mutational status of the cohort. Fifty-six UTUC patients (UTUC cohort), 50 patients with microscopic or macroscopic hematuria caused by other than UC (hematuria cohort), 21 patients with no evidence of disease for at least 1 year after TURBT or RNU (UC surveillance cohort), and 26 healthy controls (HC cohort) were included in this study. Median age was 74.5 years (range: 55-92 years) in the UTUC cohort, 68 years (range: 33-89 years) in the hematuria cohort, 70 years (range: 47-89 years) in the UC surveillance cohort, and 57 years (range: 31-81 years) in the HC cohort. Median follow-up time was 13 months (range: 1-60 months). Of the 56 UTUC patients, 54 (96.4%) received RNU, one (1.8%) received Bacillus Calmette-Guérin therapy for carcinoma in situ of UTUC, and one (1.8%) received platinum-based chemotherapy for clinical T4 UTUC. Nineteen UTUC patients (33.9%) experienced non-invasive bladder recurrence, 12 (21.4%) progressed to metastatic disease including one patient with pT1pN1 at the time of RNU, and three (5.4%) patients died from UTUC during follow up. Hotspot mutation analysis of cfDNA in urine supernatant extracted from all of these patients was carried out (Figure 1). The amount of cfDNA extracted from the UC surveillance cohort and HC cohort was significantly lower than that from the UTUC patients (Figure S1A). No significant difference was observed in the amount of cfDNA between high stage and low stage or high grade and low grade (Figure S1B,C). There was no association between mutant copy number and pathological grade or stage (Figure S1D,E). Fractions of UTUC patients harboring a mutation were 22/56 (39.3%) for TERT C228T, 4/56 (7.1%) for TERT C250T, 9/56 (16.1%) for FGFR3 S249C, 5/56 (8.9%) for PIK3CA E545K, and 32/56 (57.1%) for any mutation (Table 2, Figure 2). Because the detection rate of mutant PIK3CA was very low and overlapped with other mutations, hereafter, we focus on the analysis of FGFR3 and TERT promoters (C228T and C250T). There was no association between the rate of mutation detection and smoking history, but more mutations were detected in older patients (75%, 21/28) than in younger ones (35.7%, 10/28; P = 0.031; Figure 2). Multivariate logistic regression analysis showed that after adjustment for age, gender and urine cytology, both mutation of TERT promoter and FGFR3 were significant predictors of the presence of UTUC (TERT promoter: OR 23.24, 95% CI 5.66-134.43, P-value <0.0001; FGFR3: OR 1.06E+9, 95% CI 2.77–infinity, P-value = 0.006). Urine cytology was positive in 25 (44.6%) of the UTUC patients. Of these 25 cytology-positive patients, 48.0% (12/25) had at least one mutation, whereas 19 of 31 (61.3%) cytology-negative patients harbored at least one mutation (Figure 3). After analyzing the hematuria cohort as the control group, in combination with the cytology test results, sensitivity was 78.6% (44/56), specificity was 96.0% (48/50), PPV was 95.7%, and NPV was 80.0% for detecting UTUC (Table 3).
| UTUC cohort (n = 56) | Hematuria cohort (n = 50) | UC surveillance cohort (n = 21) | HC cohort (n = 26) | |
|---|---|---|---|---|
| Age, y, median (range) | 74.5 (55-92) | 68 (33-89) | 70 (47-89) | 57 (31-81) |
| Gender (male/female) | 46/10 | 37/13 | 17/4 | 12/14 |
| FGFR3 S249C | 9/56 (16.1%) | 0/50 (0.0%) | 0/21 (0.0%) | 0/26 (0.0%) |
| TERT C228T | 22/56 (39.3%) | 0/50 (0.0%) | 1/21 (4.8%) | 0/26 (0.0%) |
| TERT C250T | 4/56 (7.1%) | 0/50 (0.0%) | 1/21 (4.8%) | 1/26 (3.8%) |
| PIK3CA E545K | 5/56 (8.9%) | 0/44 (0.0%) | 1/17 (5.9%) | 0/12 (0.0%) |
- HC, healthy control; UC, urothelial carcinoma; UTUC, upper tract urothelial carcinoma.
| Overall (n = 56) | FGFR3 S249C (n = 9) | TERT C228T (n = 22) | TERT C250T (n = 4) | PIK3CA E545K (n = 5) | Wild type (n = 24) | |
|---|---|---|---|---|---|---|
| Age, y, median (range) | 74.5 (55-92) | 77 (55-82) | 78.5 (55-92) | 78.5 (67-89) | 76 (67-83) | 72.5 (58-88) |
| Gender | ||||||
| Male/female | 46/10 | 7/2 | 17/5 | 4/0 | 5/0 | 20/4 |
| Smoking history (%) | ||||||
| Yes | 37 (66.1) | 7 (77.8) | 13 (59.1) | 2 (50.0) | 4 (80.0) | 17 (70.8) |
| No | 14 (25.0) | 1 (11.1) | 6 (27.3) | 2 (50.0) | 0 (0.0) | 5 (20.8) |
| Unknown | 5 (8.9) | 1 (11.1) | 3 (13.6) | 0 (0.0) | 1 (20.0) | 2 (8.3) |
| UBC history (%) | ||||||
| Former | 10 (17.9) | 1 (11.1) | 4 (18.2) | 2 (50.0) | 0 (0.0) | 3 (12.5) |
| Never | 46 (82.1) | 8 (88.9) | 18 (81.8) | 2 (50.0) | 5 (100.0) | 21 (87.5) |
| Side (%) | ||||||
| Right | 23 (41.1) | 4 (44.4) | 9 (40.9) | 3 (75.0) | 3 (60.0) | 8 (33.3) |
| Left | 33 (58.9) | 5 (55.6) | 13 (59.1) | 1 (25.0) | 2 (40.0) | 16 (66.7) |
| Cytology (%) | ||||||
| ≤3 | 31 (55.4) | 5 (55.6) | 14 (63.6) | 3 (75.0) | 3 (60.0) | 12 (50.0) |
| ≥4 | 25 (44.6) | 4 (44.4) | 8 (36.4) | 1 (25.0) | 2 (40.0) | 12 (50.0) |
| T stage (%) | ||||||
| Ta or Tis | 17 (30.4) | 5 (55.6) | 6 (27.3) | 1 (25.0) | 1 (20.0) | 7 (29.2) |
| T1 | 11 (19.6) | 4 (44.4) | 5 (22.7) | 1 (25.0) | 1 (20.0) | 3a (12.5) |
| ≥T2 | 28 (50.0) | 0 (0.0) | 11 (50.0) | 2 (50.0) | 3 (60.0) | 14 (58.3) |
| Grade (%) | ||||||
| Low | 7 (12.5) | 4 (44.4) | 4 (18.2) | 0 (0.0) | 2 (40.0) | 1 (4.2) |
| High | 47 (83.9) | 5 (55.6) | 18 (81.8) | 3 (75.0) | 3 (60.0) | 22 (91.7) |
| Unknown | 2 (3.6) | 0 (0.0) | 0 (0.0) | 1 (25.0) | 0 (0.0) | 1 (4.2) |
| Tumor site (%) | ||||||
| Renal pelvis | 17 (30.4) | 3 (33.3) | 8 (36.4) | 1 (25.0) | 0 (0.0) | 7 (29.2) |
| Ureter | 33 (58.9) | 6 (66.7) | 10 (45.5) | 3 (75.0) | 4 (80.0) | 15 (62.5) |
| Both | 6 (10.7) | 0 (0.0) | 4 (18.2) | 0 (0.0) | 1 (20.0) | 2 (8.3) |
| Hydronephrosis (%) | ||||||
| Yes | 36 (64.3) | 7 (77.8) | 13 (59.1) | 3 (75.0) | 4 (80.0) | 15 (62.5) |
| No | 20 (35.7) | 2 (22.2) | 9 (40.9) | 1 (25.0) | 1 (20.0) | 9 (37.5) |
| Prognosis (%) | ||||||
| NMIBC recurrence | 19 (33.9) | 3 (33.3) | 8 (36.4) | 1 (25.0) | 3 (60.0) | 8 (33.3) |
| Metastasis | 12 (21.4) | 1 (11.1) | 4 (18.2) | 0 (0.0) | 1 (20.0) | 8 (33.3) |
- NMIBC, non-muscle-invasive bladder cancer; UTUC, upper tract urothelial carcinoma.
- a Including N+ (1 sample).

| Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | |
|---|---|---|---|---|
| TERT promoter mutation | 46.4 | 100.0 | 100.0 | 62.5 |
| FGFR3 mutation | 16.1 | 100.0 | 100.0 | 51.5 |
| TERT promoter and FGFR3 mutations | 55.4 | 100.0 | 100.0 | 66.7 |
| Cytology | 44.6 | 96.0 | 92.6 | 60.8 |
| Combined (TERT, FGFR3 and cytology) | 78.6 | 96.0 | 95.7 | 80.0 |
- NPV, negative predictive value; PPV, positive predictive value.
A TERT promoter mutation was detected in two of the 21 patients in the UC surveillance cohort. One of the patients who had a TERT C228T mutation experienced recurrence of non-invasive bladder tumor approximately 2 years after collection of this urine. The other patient who had a TERT C250T mutation experienced no bladder recurrence over a 30-month observation period. Of the 26 individuals in the HC cohort, only one person was determined to be positive for a TERT C250T mutation. She is a kidney transplantation donor and had not experienced UC during her 17-month observation period. A TERT C228T mutation was detected in 35.2% (6/17) of pTa or Tis tumors, in 45.5% (5/11) of pT1 tumors, and in 39.3% (11/28) of ≥pT2 tumors. An FGFR3 S249C mutation was detected in 29.4% (5/17) of pTa or Tis tumors and in 36.4% (4/11) of pT1 tumors, but it was not detected in any of the muscle-invasive tumors (≥pT2) (0/28) (Table 2). Sensitivity and PPV for detecting ≤T1 tumor by FGFR3 S249C were 32.1% and 100.0%, respectively.
After excluding two patients who, respectively, received BCG therapy or platinum-based chemotherapy without RNU, we analyzed 54 UTUC patients for survival. However, no significant difference was observed in prognosis (bladder recurrence-free survival or overall survival) between TERT promoter mutation and wild type (Figure 4A,B). UTUC patients with high MAF of the TERT C228T mutation in urinary cfDNA had shorter overall survival than those with low MAF (P = 0.040) (Figure S2A). In contrast, MAF of TERT C228T mutation was not associated with bladder recurrence-free survival among patients with TERT C228T mutation (P = 0.110) (Figure S2B). There was no association between overall survival and tumor copies in urine in the overall cohort (P = 0.899) (Figure S2C).
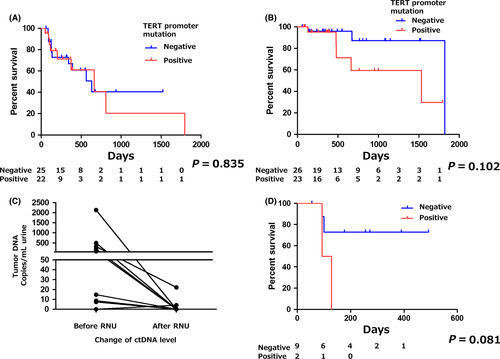
Of the 12 patients in whom both pre- and post-surgery urinary cfDNA could be analyzed, clearance of ctDNA after RNU was confirmed in seven (58.3%) patients, but in two patients (16.7%), ctDNA persisted even after RNU (Figure 4C). The patients in whom ctDNA persisted tended to have a worse prognosis for recurrence of non-muscle-invasive urothelial bladder carcinoma compared with those who experienced clearance of ctDNA (P = 0.081) (Figure 4D). In six samples, we also investigated DNA of matched samples from FFPE specimens by ddPCR. We were able to confirm the same genetic status in the urinary cfDNA, which was consistent with the DNA from the FFPE specimens.
4 DISCUSSION
In this proof-of-concept study, we showed the diagnostic potential of the TERT promoter and FGFR3 mutations detected by ddPCR of cfDNA extracted from urine supernatant of patients with localized UTUC.
There have been several studies on urinary pellet DNA and urine supernatant cfDNA from UBC patients. Various mutations could be detected in urinary pellet DNA,25-27 and in urinary cfDNA12, 22 from UBC. Russo et al26 reported that 92% of urinary cfDNA analyzed by ddPCR showed the same mutational result as that from the matched tumor tissue analyzed by NGS. Togneri et al22 reported that urinary cfDNA of UBC patients has a higher tumor genomic burden and greater detection potential as a genomic biomarker (90%) than urinary pellet DNA (61%). Moreover, some researchers have reported that circulating cfDNA in the blood of patients with advanced cancer was filtrated through glomeruli and detected in urine as “trans-renal cfDNA.”28 Urinary cfDNA may have the potential to allow observation of the sequential genetic change of UC, from detecting the disease at an early stage to monitoring the response of systemic therapy, even if there is no evidence of disease in the urinary tract.10
Springer et al16 reported that mutant DNA in urinary pellets from UTUC patients in Taiwan could be detected by NGS at rates of 25.0% (TERT C228T), 7.1% (TERT C250T), 10.7% (FGFR3 S249C), and 5.4% (PIK3CA E545K). In the current study, we could detect mutations at rates of 39.3% (TERT C228T), 7.1% (TERT C250T), 16.1% (FGFR3 S249C), and 8.9% (PIK3CA E545K) in urinary cfDNA in Japanese patients. The difference in detection rates may be due to differences of the cohorts investigated because as Springer et al reported, the Taiwanese cohort was highly exposed to aristolochic acid, a known carcinogenic and nephrotoxic agent in Aristolochia herbs, whereas our Japanese cohorts were not.
Because hematuria has high sensitivity for detecting urothelial carcinoma, it is useful for mass screening. However, as a result of the low specificity of hematuria, an additional specific test is necessary to make a definitive diagnosis of UTUC. Urine cytology is a non-invasive test and is often chosen because of its high specificity as a primary approach by the physician to differentiate urological malignancies from benign diseases such as hematuria or dysuria. However, its sensitivity for diagnosis is relatively low, 16%-84% in UBC29 and 40% in UTUC.8 In the present study, we could detect the three targeted gene mutations (TERT C228T, TERT C250T, and FGFR3 S249C) in 55.4% of urine samples from UTUC patients. In combination with urine cytology, our non-invasive method could have high sensitivity (78.6%) for the detection of UTUC and be useful in making a definitive diagnosis. To some extent, UTUC shares the same gene alterations as UBC, so this method might also be a useful tool for detecting UBC for bladder surveillance after RNU. In bladder tumors, the TERT promoter mutation occurs frequently in precancerous lesions and in low-grade UBC, high-grade UBC, squamous cell carcinoma of the urinary bladder, adenocarcinoma of the urinary bladder, micropapillary urothelial carcinoma and plasmacytoid urothelial carcinoma.18, 30-35 Thus, the TERT promoter mutation has been established as a common genetic alteration in UC. We could detect TERT promoter mutation at any stage of UTUC, and this finding also supports the fact that TERT promoter mutation occurs as an early genetic event in carcinogenesis. Moreover, several researchers reported that TERT promoter mutation is associated with bladder recurrence and survival in UBC.36-38 Isharwal et al reported that the TERT promoter mutation was associated with overall survival (HR: 2.31, 95% CI: 1.46-3.65), disease-specific survival (HR: 2.23, 95% CI: 1.41-3.53), and metastasis-free survival (HR 1.63, 95% CI: 1.05-2.53).38 Christensen et al12 showed a significant association between ctDNA level and tumor grade and also that the amount of ctDNA from patients whose DNA extracted from bladder tumor tissue was mutation positive was significantly associated with progression-free survival or recurrence-free survival. However, in the present study, we could not find a significant association between ctDNA level and prognosis. This may be a result of the small sample cohort and short observation period. In this study, a post-RNU TERT promoter mutation tended to be associated with worse prognosis for bladder recurrence in UTUC. Larger-scale studies are necessary to confirm these findings in UTUC.
Besides TERT promoter mutation, we selected FGFR3 mutation as an additional biomarker candidate. Sfakianos et al reported that 30.4% of tissue from UTUC harbors a FGFR3 S249C hotspot mutation, and most of the FGFR3 mutations were detected in non-muscle-invasive UTUC.15 Consistent with a previous report, in the present study, all FGFR3 S249C mutations were detected at the early stage (at most pT1) of UTUC. It is difficult to accurately diagnose the pathological stage with CT or magnetic resonance imaging, especially in ureteral tumors, because the muscle layer of the ureter is very thin. Guidelines of the European Association of Urology recommend carrying out ureteroscopy for pathological staging6 and to offer ureteroscopic nephron-sparing surgery for patients with low-risk UTUC. In this study, the sensitivity and PPV for detecting ≤T1 tumor by FGFR3 S249C were 32.1% and 100.0%, respectively. Although the sensitivity is relatively low, a positive result of an FGFR3 mutation in urinary cfDNA could help to predict a low-stage tumor as a liquid biopsy not requiring tissue examination. This assay for FGFR3 mutation may have the potential to become an alternative for ureteroscopy and a reliable factor for deciding whether to carry out ureteroscopic nephron-sparing surgery.
This study has several limitations because of its small population size and short follow-up period. The median age of the hematuria cohort is significantly younger than that of the UTUC cohort. Because there was an association between age and the prevalence of mutation in the UTUC cohort, the difference in age between the UTUC and hematuria cohorts could have influenced the positive rate of detecting mutant cfDNA. However, there are no reports of an increased rate of TERT promoter mutation in healthy elderly compared with healthy young persons. Further prospective large-scale studies and a longer follow-up period are warranted to confirm our findings. TP53 is well known as one of the key players in carcinogenesis and is frequently mutated in UC. Although our urinary cfDNA ddPCR assay targeting three hotspot mutations has low sensitivity for detecting UTUC, massive parallel sequencing of multiple genes could be applicable to the analysis of urinary cfDNA and might increase sensitivity, thus providing more benefit to patients.16 In combination with the results of cytology, our assay for urinary cfDNA may lead to an earlier diagnosis of UTUC and optimized follow-up strategy and may help the physician avoid an invasive procedure to determine a definitive diagnosis. In conclusion, we could detect TERT promoter and FGFR3 hotspot mutations in urinary cfDNA from UTUC patients. In combination with cytology results, the sensitivity of our non-invasive urinary test was high enough to apply this assay to the clinical setting. Liquid biopsy analysis of TERT promoter and FGFR3 mutations in urinary cfDNA could be a novel diagnostic biomarker and a reliable factor for staging UTUC.
CONFLICTS OF INTEREST
Authors declare no conflicts of interest for this article.