Double-edged sword of mesenchymal stem cells: Cancer-promoting versus therapeutic potential
Funding Information
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT & Future Planning (NRF-2016R1C1B2009351).
Abstract
Mesenchymal stem cells (MSCs) derived from adipose tissue, bone marrow, cord blood, and other tissues, have recently attracted much attention as potential therapeutic agents in various diseases because of their trans-differentiation capacity. However, recent studies have suggested that MSCs also appear to contribute to tumor pathogenesis by supporting tumor microenvironments, increasing tumor growth, and eliciting antitumor immune responses. Although some studies suggest that MSCs have inhibitory effects on tumor development, they are overwhelmed by a number of studies showing that MSCs exert stimulatory effects on tumor pathogenesis. In the present review, we summarize a number of findings to provide current information about the therapeutic potential of MSCs in various diseases. We then discuss the potential roles of MSCs in tumor progression.
Despite tremendous efforts made in many countries to improve current treatment and diagnosis strategies, many malignant tumors still remain unresponsive to conventional treatments such as chemotherapy and radiation. Former therapeutic strategies for most cancers have focused on the cancer cell itself. However, many recent studies have suggested that coordinated communications between cancer cells and their surrounding microenvironment exert a more profound effect on the development of malignancy than has previously been appreciated.1 The tumor environment is made up of cancer cells as well as a number of cellular components, including endothelial cells, fibroblasts, mesenchymal stem cells (MSCs), and various inflammatory cell types.2 Cancer cells release regulatory molecules that stimulate the surrounding stromal cells to proliferate and migrate into the tumor. These stromal cells, in turn, release various cytokines that promote tumor growth, invasion, and resistance to chemotherapy or radiation.
The ability of tumor-associated MSCs to modulate the tumor microenvironment has been the subject of intense investigation in the fields of cancer research. Although some studies suggest that MSCs have inhibitory effects on cancer cell growth and metastasis,3-5 they are overwhelmingly outnumbered by a number of studies showing that MSCs have the ability to migrate into tumor sites6 and exert stimulatory effects on tumor development.7 In the present review, we summarize a number of results to provide a detailed overview of therapeutic implications of MSCs in regenerative medicine and the potential roles of MSCs in tumor development as the constituents of the tumor microenvironment.
Characterization of MSCs
In early 1970's, Friedenstein et al.8 were the first to identify the presence of mouse BM-derived fibroblast-like cells (now known as MSCs) that had the capacity to give rise to multiple cell lineages, including osteoblast and chondrocyte. Over the years, a large number of studies have provided evidence in support of their potential applications in tissue engineering and regenerative medicine. MSCs are classically defined by their potential to differentiate into three different mesodermal lineages, namely adipocytes, chondrocytes, and osteoblasts.9, 10 Under appropriate culture conditions MSCs have also been differentiated into endodermal (epithelial cells and hepatocytes) and ectodermal (neuronal cells) cells; hence, their differentiation potential is not limited to mesodermal derivatives.11-14 Commonly, MSCs were further characterized by the expression of a range of cell positive (CD29, CD44, CD49, CD73, CD90, CD105, CD106, CD140b, CD166 and STRO-1) and negative (CD11b, CD14, CD19, CD31, CD34, CD45 and CD133) surface antigens.10 Using these cell surface markers, we were able to isolate MSCs from multiple human tissues, including adipose tissue, amniotic fluid, BM, peripheral blood, fetal liver, and UCB.15-18
In vivo Niche for MSCs
It was previously thought that MSCs primarily reside in the BM in so-called niches. MSCs are considered to be an essential constituent of the BM microenvironment where they support basal hematopoiesis. However, many recent studies suggest that they have also been identified in other tissues, such as adipose tissue, lung, muscle, periodontal ligament, salivary glands, skin, and UCB.19 Accumulating evidence has revealed that MSCs can repair injured tissue through direct differentiation toward mesoderm/mesenchyme lineages.20 Furthermore, they may also be able to repair damaged tissues through paracrine actions.21 Besides these tissue repair functions, increasing evidence from recent studies demonstrates that MSCs are capable of suppressing the immune response through direct cell–cell contact and/or secreted soluble factor.22
Therapeutic Potential of MSCs in Regenerative Medicine
Mesenchymal stem cells represent one of the few multipotent adult stem cells that are already widely clinically used for tissue repair/regeneration. Besides the traditional mesoderm/mesenchymal differentiation potential, MSCs can differentiate into extra-mesenchymal lineages, such as ectodermal and endodermal lineage cells. Recent studies have suggested that MSCs have trans-differentiation capacity and may thus be a promising therapeutic resource for regenerative medicine. Furthermore, MSCs are easily accessible from donors and expandable in vitro on a large scale without posing significant ethical problems, making them a reliable cell source for many clinical applications. As well as providing scaffolding architecture, MSCs themselves are critical for niche formation and maintenance in BM by secreting various cytokines that influence hematopoiesis.23 Indeed, MSCs have previously been shown to accelerate healing and hematopoietic recovery in breast cancer patients receiving chemotherapy.24 Furthermore, MSCs have long been reported to have immune privilege status with low MHC I and no MHC II expression; this property is thought to enable MSCs transplantation with a low risk of cellular rejection.25 The immunosuppressive properties of MSCs are achieved through paracrine inhibition of T- and B-cell proliferation and differentiation.26 Currently, MSCs have also been used to treat a variety of bone-related diseases. The osteogenic differentiation potential of MSCs has been used to treat and manage bone fractures alone or in combination with scaffolds with a high clinical success rate.27 In clinical studies, Stamm et al.28 have also shown that autologous BM-derived MSCs are effective in treating myocardial infarction. Consistent with this study, it was observed that MSCs can differentiate into functional myocardial-like cells in vitro, although the underlying pathophysiological mechanisms remain to be elucidated.29, 30 Systemically injected MSCs into animals with traumatic brain injury has also been shown to preferentially migrate to the site of injury and improve recovery, although whether these therapeutic effects are a result of secretion of neuromodulatory factors or direct differentiation into neural cells remains to be elucidated.31, 32 Therefore, MSCs are one of the most interesting areas of stem cell research demanding further investigation into their clinical use.
Potential Tumorigenicity of MSCs-Based Therapies
Mesenchymal stem cells have been discovered in multiple adult tissues including bone, cartilage, fat, muscle, and tendon and exhibit extensive self-renewal ability and wide multi-lineage differentiation potential.33 Indeed, a number of non-clinical studies and clinical trials have reported promising beneficial effects of MSCs transplantation.34-37 However, several studies have observed potential adverse effects of MSCs, including tumor growth, metastasis, and transformation into cancer cells.38-40 Recently, it was reported that human pulmonary tissue-derived MSCs exhibit high proliferative capacity with unbalanced chromosomal rearrangements, but there was no evidence of malignant transformation.41 Moreover, Houghton et al.42 demonstrated that bone marrow-derived MSCs progressed to gastric epithelial cancer in mice experimentally infected with Helicobacter hepaticus. These adverse effects may be explained by a heterogeneous MSCs population used in experiments carried out by Rosland et al.43 and Rubio et al.44 that was originally contaminated by cells that initially grew slowly and then transformed into cancer cells.45, 46 Moreover, current immune-deficient animal models may not be suitable for predicting tumor initiation or progression. It was highlighted that the immunological status of experimental animals should be considered in studies designed for evaluation of tumorigenicity of MSCs. When MSCs were allogeneically transplanted into immunocompetent mice, immune rejection of allogeneic cells may prevent development of tumor in vivo. To date, no cancer has been diagnosed or has recurred in clinical trials that would originate from experimentally given MSCs. However, potential tumorigenicity of MSCs should be further explored and monitored in order to elucidate the risk of potential tumorigenicity related to MSCs-based therapies.
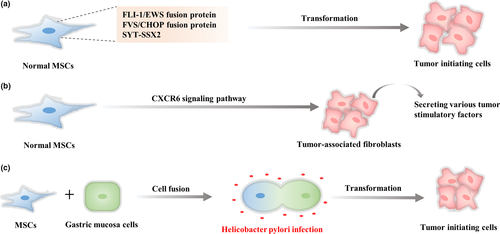
MSCs as a Direct Cellular Origin of Cancer
The origin of cancer cells is an area of ongoing research. Recently, MSCs have been indicated as the cellular origin of certain chromosomal translocation-associated solid tumors.47 Indeed, a number of studies have suggested that the introduction of the FLI-1/EWS fusion protein into MSCs may cause transformation of these cells into malignant sarcoma cells.48 Consistent with these studies, ectopic expression of other oncogenic proteins, such as the FUS/CHOP fusion protein or synovial sarcoma translocated protein (SYT-SSX1), in human MSCs can cause transformation of MSCs into myxoid liposarcomas49 or sarcoma cells,50 respectively. Taken together, these studies support the hypothesis that MSCs may represent target cells for oncogenic development of sarcoma. In addition, the CXCR6 signaling pathway stimulates transformation of MSCs into cancer-associated fibroblasts which secrete various tumor stimulating factors.51 Interestingly, Houghton et al.42 found that MSCs may initiate gastric cancer development by fusing with gastric mucosal cells under Helicobacter pylori infection. However, it is yet to be determined whether or not MSCs also give rise to other cancer types. Transformations of MSCs into malignant cells are summarized in Figure 1, highlighting the role of the signaling proteins in stimulating tumorigenesis.
MSCs Migrate Preferentially Towards Tumor Sites
Rapidly growing cancers have been shown to induce a persistent inflammatory microenvironment which may be similar to that evoked by the wound-healing response.52 Interestingly, accumulating evidence indicates that MSCs are able to preferentially migrate into tumor sites in a similar way to how they are recruited into sites of injury.53 Indeed, systemically injected MSCs accumulated at tumor sites in tumor-bearing mice with limited homing capacity to other organs.54, 55 Factors responsible for MSCs recruitment to tumors have emerged as a new exciting research field. Recent advances have shown that the factors responsible for the recruitment of hematopoietic stem cells (HSC), such as basic fibroblast growth factor (bFGF),56 hepatoma-derived growth factor (HDGF),57 interleukin-6 (IL-6),58 monocyte chemotactic protein-1 (MCP-1),59 stromal-cell derived factor (SDF-1),60 urokinase plasminogen activator (uPA),61 and vascular endothelial growth factor (VEGF),56 have also been involved in the migration capacity of MSCs toward tumor xenografts (Fig. 2). Although various factors are responsible for MSCs tropism, inflammatory-related responses appear to be important regulators of MSCs recruitment to tumor sites. However, it is important to note that the inhibition of a single factor alone appears to be effective, but not sufficient to completely disrupt MSCs homing and migration into tumor sites.62 These results suggest that the sophisticated interplay of multiple components appears to be involved in their tropism to tumors. MSCs recruitment to developing tumors with great affinity may initiate a vicious cycle in tumor progression, causing further recruitment of MSCs to tumor sites, thereby exacerbating various steps of tumor development such as proliferation/apoptosis, invasion, metastasis, and angiogenesis.19, 63

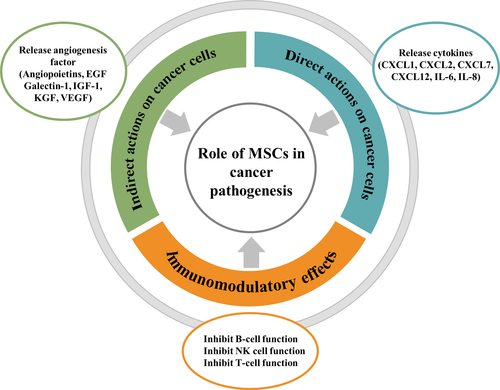
Role of MSCs in Cancer Pathogenesis
Tumor initiation and progression is not only affected by genetic alterations in the tumor cell itself but potentially also by non-tumor cells present in the microenvironment. In addition to neoplastic cells, the tumor microenvironment is composed of multiple non-tumor cell types, including blood vessel cells, various immune cells, fibroblasts, and MSCs. In particular, MSCs have been shown to communicate with cancer cells directly through gap junctions as well as indirectly through soluble factors such as cytokines, chemokines, complement factors, growth factors, metabolites, and proteolytic enzymes. Contribution of MSCs to tumor pathogenesis has been the subject of intense scientific research in recent years. As their potential roles in cancer pathogenesis are still being elucidated in detail, several possible mechanisms through which MSCs promote cancer progression and metastasis are summarized in Table 1.
| Action mechanism | Target | Cell type | References |
|---|---|---|---|
| Direct actions on cancer cells | Release cytokines (CXCL1, CXCL2, and CXCL12) | Breast cancer | 64, 65 |
| Release inflammatory factors (IL-6 and IL-8) |
Colon cancer Breast cancer |
66, 67 | |
| Indirect actions on cancer cells | Release angiogenesis factor (angiopoietins, EGF, galectin-1, IGF-1, KGF, and VEGF) |
Colon cancer Skin cancer |
47, 69 |
| Immunomodulatory effects | Inhibit B-cell function | B-cell | 76 |
| Inhibit natural killer cell function | Natural killer cell | 77 | |
| Inhibit T-cell function | T-cell | 78, 79 |
- CXCL, chemokine (C-X-C motif) ligand; EGF, epidermal growth factor; IGF, insulin-like growth factor; IL, interleukin; KGF, keratinocyte growth factor; MSCs, mesenchymal stem cells; VEGF, vascular endothelial growth factor.
Direct actions on cancer cells
Recent observations suggest that MSCs produce and secrete a number of paracrine factors, such as chemokines, cytokines and growth factors, thereby regulating tumor progression and metastasis in many tumors. Indeed, MSCs-derived inflammatory modulators, such as CXCL1, CXCL2 or CXCL12, have been shown to accelerate tumorigenesis in a wide range of tumor models through their respective receptors CXCR2 and CXCR4 on the cells.64, 65 Similarly, MSCs-derived inflammatory chemokines, including IL-6 and IL-8, have been shown to promote malignant potential in multiple cancer models, such as colon66 and breast.67 Consistently, recent studies have revealed that fluorescence dye-labeled MSCs migrated into rapidly growing breast cancer xenografts and increased CSC subpopulations through a paracrine mechanism involving IL-6 and CXCL7.67
Indirect actions on cancer cells
Recent studies have demonstrated the MSCs typically facilitate angiogenesis through paracrine secretion of angiogenic growth factors.68 Indeed, MSCs may stimulate tumor neo-angiogenesis within the primary tumor through the production and secretion of tumor angiogenesis factor, such as angiopoietins, EGF, galectin-1, IGF-1, KGF, and VEGF47, 69 and are intimately involved in the recruitment of endothelial cells, thereby promoting the formation of new blood vessels in and around a tumor.70, 71 Furthermore, recent studies have demonstrated that MSCs can differentiate into endothelial cells, resulting in significant increased tumor vascularity.72, 73 These observations highlight the distinct aspect of their tumor-supporting potential and suggest that targeting MSCs appears to be one of the most promising treatment strategies for highly vascularized tumors.
Immunomodulatory characteristics of MSCs
Recent investigations have demonstrated that MSCs may also act as an immune regulator to suppress both innate and adaptive immunity.74, 75 MSCs may modulate immune responses through regulation of the proliferative capacities of various immune cells which are important in maintaining self-tolerance and immune homeostasis. Indeed, MSCs have been shown to significantly inhibit B-cell proliferation and maturation76 as well as NK cells,77 resulting in less secretion of soluble immune mediators and NK-mediated cytotoxicity, respectively. Consistent with these results, MSCs have recently been shown to inhibit the proliferation of CD4+/CD8+-activated T cells by cell–cell contact.78 MSCs may even suppress T-cell proliferation indirectly by regulating the proliferation and maturation of immune-regulatory DC, which trigger generation of regulatory T cells.79
Taken together, the immunomodulatory properties of MSCs may be mediated, at least in part, by direct cell–cell contact and/or specific immune-modulatory factors secreted by MSCs, thereby promoting tumor growth and progression. A schematic diagram summarizes the potential roles of MSCs in tumor development (Fig. 3).
Inhibitory Effects of MSCs on Cancer Cell Growth
In contrast to the tumor-stimulatory effect of MSCs, various studies have shown that MSCs inhibit tumor progression and metastasis by suppressing immune responses, inhibiting angiogenesis, suppressing Akt and Wnt signaling, and inducing apoptosis or cell cycle arrest in the G0-G1 phase.80 Indeed, co-administration of glioma cells and MSCs resulted in significantly decreased tumor growth and angiogenesis by suppressing Akt signaling in a murine experimental model.81 Subsequently, several studies have also demonstrated tumor suppressive effects of MSCs in multiple types of cancer. Ohlsson et al.82 showed that MSCs effectively inhibited the growth of colon carcinoma by infiltrating immune cells in vivo. MSCs also exhibited potent antitumor activity of both hematopoietic and non-hematopoietic origin by inducing G1 phase cell cycle arrest.83 In addition, Clarke et al.5 showed that MSCs reduce migration and invasion of human breast cancer cells through regulating the secretion of TIMP-1 and -2. Similarly, MSCs can significantly decrease the proliferation of chronic myelogenous leukemia in a cell-to-cell contact-independent way and these suppressive effects were achieved through DKK-1 (dickkopf-1) secretion.84 Khakoo et al. also reported that tumor-suppressive effects of MSCs can be correlated with their ability to inhibit target cell Akt signaling activity in a contact-dependent way.85 A potential mechanism of MSCs-mediated tumor cell suppression could also be related to its immunosuppressive effects. As modulators of immune responses, MSCs produce multiple immunomodulators that suppress the growth of various immune cells by arresting the early stages of the cell cycle.86, 87 These MSCs-mediated inhibitory effects on multiple types of immune cells can also be produced on other “non-immune” cells. In this context, Ramasamy et al.83 demonstrated that MSCs inhibit cell proliferation of multiple malignant cell types of both immune and non-immune origin. Importantly, these conflicting results regarding the influence of MSCs on tumor development may be caused by various experimental conditions such as differences in time points after treatment, different cell source (adipose tissue, bone marrow, and peripheral blood), and route of cell administration (intramuscular, intravenous, and subcutaneous injection).19 Therefore, the role of MSCs in cancer progression and metastasis is under debate and its molecular mechanism is not yet fully established.
Communication Between MSCs and Cancer Through EV
Extracellular vesicles are 40–1000-nm membrane-enclosed vesicles that are produced and released by the pinching off of the outer membrane.88 EV are released from various cell types, including MSCs, constitutively or under stimulation, and exert different effects depending on the target cell.89 MSCs-EV express some characteristic markers of their origin, such as CD29, CD44, CD73, and CD105.90 MSCs-EV also contain a variety of molecules associated with MSCs self-renewal and multi-lineage differentiation potential (TGF-β, MAPK, PPAR etc.),91 lipids, and genetic materials (mRNA and miRNAs)92 involved in multiple biological functions.
Tumor-supportive effects of MSCs-EV
Vallabhaneni et al.93 demonstrated that bone marrow-derived MSCs-EV contain a large amount of tumor-supportive small RNA (miRNA-21 and 34a), and approximately 150 different factors, most of which are known tumor-supportive proteins such as PDGFR-β, TIMP-1, and TIMP-2. Indeed, they also demonstrated the tumor supportive function of these EV in a breast cancer xenograft model.93 Zhu et al.94 also revealed that MSCs-EV promote tumor growth in vivo by enhancing VEGF expression and ERK1/2 signaling activity in gastric and colon cancer xenograft models. Umbilical cord-derived MSCs-EV can protect against cisplatin-induced renal oxidative stress and apoptosis in vivo and in vitro.95 Subsequently, Yang et al.96 demonstrated that MSCs-EV were associated with the acquisition of protumorigenic properties by enhancing the expression of MMP-2 and MSCs-specific markers (CD73 and CD90) in breast and ovarian cancer cells. In addition, Salomon et al.97 have revealed that placental MSCs-EV promote the migration and angiogenic tube formation of microvascular endothelial cells under hypoxic conditions. Lin et al.98 noted that MSCs-EV stimulate the migration and growth of breast cancer cells by enhancing Wnt/β-catenin signaling. Taken together, these findings suggest that MSCs-EV can mediate intercellular communication to improve tumor growth and metastasis.
Antitumor effects of MSCs-EV
In contrast to the tumor-stimulatory effect of MSCs-EV, various studies have shown that bone marrow-derived MSCs-EV induced cell-cycle arrest in the G0/G1 phase and apoptosis of multiple types of cancer cells such as hepatoma, Kaposi's sarcoma, and ovarian cancer cells, in vitro and in vivo.99 Lee et al.100 observed that MSCs-EV suppressed angiogenesis by down-regulating VEGF expression in tumor cells, which lead to angiogenesis inhibition in vitro and in vivo. Moreover, liver stem cell-derived EV inhibited the growth of multiple types of cancer cells such as glioblastoma, hepatoma, and lymphoblastoma cells, both in vitro and in vivo.101 Another study has also presented the same result; MSCs-EV exhibited a potent anti-angiogenic activity by releasing multiple miRNAs that target VEGF in human nasopharyngeal carcinoma cells.102 These findings suggest that EV transfer from the various MSCs may suppress tumor growth and angiogenesis. However, the role of MSCs-EV in tumor development is still controversial and their molecular mechanisms are not yet fully established.
Conclusion
Growing evidence shows that besides the traditional mesoderm/mesenchymal differentiation potential, MSCs can differentiate into extra-mesenchymal lineages, such as ectodermal and endodermal cells. Therefore, MSCs are one of the most interesting areas of stem cell research demanding further investigation for their clinical use. However, it is also clear that tumor-derived cytokines have a remarkable capacity to attract MSCs to the tumor microenvironment. The remarkable tropism of MSCs for primary and metastatic tumor sites has been observed with almost all cancer types. It is generally thought that MSCs may be involved in multiple stages of cancer development as a source of soluble regulatory factors to regulate immune surveillance, tumor growth, and tumor angiogenesis and, when in direct contact with cancer cells, MSCs affect tumor growth, apoptosis, and chemodrug resistance. Although increased attention is now focused on the effects of MSCs on tumor progression, current knowledge about the involvement of MSCs in tumor progression and metastasis and their underlying mechanisms are still at an early stage. Therefore, more detailed information about the mutual interactions between MSCs and cancer cells will undoubtedly lead to more effective clinical therapy in the future.
Disclosure Statement
Authors declare no conflicts of interest for this article.
Abbreviations
-
- BM
-
- bone marrow
-
- CSC
-
- cancer stem cell
-
- CXCL
-
- chemokine (C-X-C motif) ligand
-
- DC
-
- dendritic cell
-
- EGF
-
- epidermal growth factor
-
- EV
-
- extracellular vesicle
-
- IGF
-
- insulin-like growth factor
-
- IL
-
- interleukin
-
- KGF
-
- keratinocyte growth factor
-
- miRNA
-
- microRNA
-
- MSCs
-
- mesenchymal stem cells
-
- NK
-
- natural killer
-
- PDGFR
-
- platelet-derived growth factor receptor
-
- PPAR
-
- peroxisome proliferator-activated receptor
-
- SYT-SSX1
-
- synovial sarcoma translocated protein
-
- TGF-β
-
- transforming growth factor beta
-
- UCB
-
- umbilical cord blood
-
- VEGF
-
- vascular endothelial growth factor