SNIPER(TACC3) induces cytoplasmic vacuolization and sensitizes cancer cells to Bortezomib
Funding Information
Japan Society for the Promotion of Science (KAKENHI Grants 26860049 to N.O.; 16H05090 and 16K15121 to M.N.), Japan Agency for Medical Research and Development (AMED) (15ak0101029 h1402 and 16ak0101029j1403 to M.N.; 16cm0106124j0001 to N.O.), Ministry of Health and Labour Welfare (to M.N) and Takeda Science Foundation (to N.O.).
Abstract
We previously developed a hybrid small molecule SNIPER (Specific and Nongenetic IAP-dependent Protein ERaser) against transforming acidic coiled-coil-3 (TACC3), SNIPER(TACC3), that induces proteasomal degradation of TACC3 protein. In this study, we found that SNIPER(TACC3) induces cytoplasmic vacuolization derived from endoplasmic reticulum (ER) and paraptosis-like cell death selectively in cancer cells. Mechanistic analysis suggests that accumulation of ubiquitylated protein aggregates that requires X-linked inhibitor of apoptosis protein (XIAP) induces ER stress, which results in ER-stress responses involving X-box binding protein-1 (XBP-1) and ER-derived vacuolization in cancer cells. Importantly, inhibition of proteasome enhanced the SNIPER(TACC3)-induced vacuolization, and the combination treatment of SNIPER(TACC3) and bortezomib exhibited a synergistic anticancer activity in several cancer cell lines. The induction of paraptosis-like cell death in cancer cells by SNIPER(TACC3) could be applied to treat cancer cells resistant to undergo apoptosis by overexpression of XIAP.
Protein knockdown is a recently developed technology to degrade target proteins by a class of chemical compounds such as SNIPERs (Specific and Nongenetic IAP-dependent Protein Erasers) and PROTACs (Proteolysis Targeting Chimeras).1 These compounds are chimeric molecules containing a ligand for a target protein of interest connected by a linker to another ligand for a ubiquitin ligase, which are designed to crosslink these proteins to induce polyubiquitylation and proteasomal degradation of the target proteins. With methyl-bestatin (MeBS) as a ligand for cellular inhibitor of apoptosis protein 1 (cIAP1) ubiquitin ligase, we have developed several SNIPER compounds targeting cellular retinoic acid-binding protein 2 (CRABP2),2, 3 estrogen receptor α (ERα),4-6 and spindle regulatory protein transforming acidic coiled-coil-3 (TACC3).7 The SNIPERs against CRABP2 and ERα induce cIAP1-mediated ubiquitylation and proteasomal degradation of the target proteins as intended.3, 6 However, SNIPER(TACC3) requires anaphase-promoting complex/cyclosome with CDH1 (APC/CCDH1) ubiquitin ligase instead of cIAP1 to induce ubiquitylation and degradation of TACC3 protein.7
A spindle-regulatory protein TACC3 is one of the attractive targets for cancer therapy because TACC3 is aberrantly expressed in various human cancers and its depletion leads to mitotic or postmitotic cell cycle arrest and occasionally induce apoptosis of cancer cells.8-13 We have previously shown that SNIPER(TACC3) induces apoptosis selectively in cancer cells expressing a large amount of TACC3 protein as compared with normal cells.7 However, caspase activation was not extensively observed in the SNIPER(TACC3)-treated cancer cells, suggesting the involvement of different cell death mechanisms.
Cell death is classified into several types, such as apoptosis, necrosis (necroptosis), autophagy-associated death, mitotic catastrophe, paraptosis and oncosis.14 Paraptosis has been characterized by cytoplasmic vacuolization that associates with extensive swelling of endoplasmic reticulum (ER), and mitochondria in some cases, in the absence of typical apoptotic features such as formation of apoptotic bodies and nuclear fragmentation.15 Several reports have shown that paraptosis or paraptosis-like cell death (PLCD) is induced by overexpression of oncogenic genes,16, 17 mutation or deletion of genes related to ER function,18-20 and exposure to natural or synthetic compounds.21-26 Notably, paraptosis or PLCD have been frequently observed in a variety of cancer cells but not in normal cells, therefore induction of paraptosis could be an alternative approach to kill cancer cells that are resistant to undergo apoptosis.21, 22, 24, 26 In this study, we demonstrate that SNIPER(TACC3) induces cytoplasmic vacuolization and PLCD in cancer cells. We also showed that the SNIPER(TACC3) sensitizes cancer cells to bortezomib.
Materials and Methods
Chemical compounds
SNIPER(TACC3)-1 and -2 were synthesized as described previously.7 The chemical synthesis and physicochemical data on the other compounds are provided in the Doc. S1, Schemes S1 and S2.
Cell culture
Human osteosarcoma U2OS, human fibrosarcoma HT1080, and human fetal lung fibroblast TIG1, TIG3, MRC5, MRC9 were maintained in Dulbecco's modified Eagle's medium containing 10% fetal bovine serum (FBS) and 100 μg/mL of kanamycin (Sigma, St. Louis, MO, USA). Human breast carcinoma MCF-7, human myeloid leukemia K562 and human Burkitt's lymphoma Raji cells were maintained in RPMI 1640 medium containing 10% FBS and 100 μg/mL of kanamycin. Human multiple myeloma RPMI-8226 and KMS-11 cells were obtained from Japanese Collection of Research Bioresources (JCRB, Osaka, Japan) Cell Bank (JCRB0034 and JCRB1179), and these cells were maintained in RPMI 1640 medium containing 10% FBS and 100 μg/mL of kanamycin.
siRNA Transfection
- UBE1 (5′-GCGCCAAAUGAAUCCACAU-3′);
- XBP1-1 (5′-GGAAGAACCUGUAGAAGAU-3′);
- XBP1-2 (5′-CCUCUCUGCUUGGUGUAAA-3′);
- ATF4-1 (5′-GCCUAGGUCUCUUAGAUGA-3′);
- ATF4-2 (5′-CCACGUUGGAUGACACUUG-3′);
- CHOP (5′-GCAGCGCAUGAAGGAGAAA-3′);
- cIAP1-1 (5′-UCUAGAGCAGUUGAAGACAUCUCUU-3′);
- cIAP1-2 (5′-GCUGUAGCUUUAUUCAGAAUCUGGU-3′);
- XIAP-1 (5′-ACACUGGCACGAGCAGGGUUUCUUU-3′);
- XIAP-2 (5′-GAAGGAGAUACCGUGCGGUGCUUUA-3′).
Western blotting
Cells were lysed with SDS lysis buffer (0.1 M Tris–HCl at pH 8.0, 10% glycerol, 1% SDS) and immediately boiled for 10 min to obtain clear lysates. The protein concentration was measured by BCA method (Pierce, Rockford, IL, USA) and the lysates containing an equal amount of proteins were separated by SDS-PAGE, transferred to PVDF membranes (Millipore, Darmstadt, Germany) for western blot analysis using the appropriate antibodies. The immunoreactive proteins were visualized using the Immobilon Western chemiluminescent HRP substrate (Millipore) or Clarity Western ECL substrate (Bio-Rad, Hercules, CA, USA), and light emission was quantified with a LAS-3000 lumino-image analyzer (Fuji, Tokyo, Japan). The antibodies used in this study were: ATF4 (Cell Signaling Technology, 11815, Danvers, MA, USA), CHOP (Santa Cruz, Dallas, TX, USA; sc-793), cIAP1 (R&D Systems, Minneapolis, MN, USA; AF8181), β-actin (Sigma A5316), XIAP (Cell Signaling Technology, 2042), LC3 (Sigma; L7543, MBL, Nagoya, Japan; M115-3), XBP-1 (Santa Cruz, sc-7160; Cell signaling Technology, 12782), UBE1 (Cell Signaling Technology, 4890), Hsp90 (BD Biosciences, 610419, San Jose, CA, USA).
Immunostaining
Cells were fixed in 100% methanol on ice for 10 min, washed four times with PBS, and blocked in PBS containing 3% BSA, 0.1% Triton X-100 (PBS-TB) for 1 h at room temperature. Cells were incubated for 2 h with the indicated antibodies as the first antibodies, and for 1 h with Alexa Fluor 488-conjugated anti-rabbit or mouse IgG or Alexa Fluor 568-conjugated anti-rabbit or mouse IgG (Life Technologies) as the second antibodies with Hoechst 33342 (Life Technologies). Fluorescent images were obtained using a BZ-9000 (Keyence, Osaka, Japan). The antibodies used were: multi-ubiquitin (MBL, D058-3), ubiquitin, Lys48-Specific (Millipore; 05-1307), TACC3 (Cell Signaling, 8069), LAMP2 (BD Biosciences, 555803), PMP70 (Abcam, Cambridge, UK; ab85550), GM130 (Abcam, ab52649), COX IV (Cell Signaling, 4850).
Cell viability assay
Cell viability was determined using water-soluble tetrazolium WST-8 (4-[3-(2-methoxy-4-nitrophenyl)-2-(4-nitrophenyl)-2H-5-tetrazolio]-1,3-benzene disulfonate) for the spectrophotometric assay according to the manufacturer's instructions (Dojindo, Tokyo, Japan). Cells treated with compounds were incubated with WST-8 reagent for 0.5 h at 37°C in a humidified atmosphere of 5% CO2. The absorbance at 450 nm of the medium was measured using an EnVision Multilabel Plate Reader (PerkinElmer, Waltham, MA, USA).
Statistical analysis
A student's t-test was used to determine the significance of differences among the experimental groups. Values of P < 0.05 were considered significant.
Results
SNIPER(TACC3) induces cytoplasmic vacuolization in cancer cells
When human osteosarcoma U2OS cells were treated with SNIPER(TACC3)-1 and -2, the cells formed remarkable cytoplasmic vacuolization (Fig. 1a, b). SNIPER(TACC3)s contain two different ligands, MeBS for cIAP1 and KHS108 for TACC3, which are connected by linkers. Combination treatment with MeBS and KHS108 did not induce cytoplasmic vacuolization, indicating that linking the two ligands is critically needed for the induction of cytoplasmic vacuolization. To investigate which chemical structure of SNIPER(TACC3) is required for the vacuolization, we replaced the KHS108 moiety of SNIPER(TACC3) with benzoyl-amide or biotin, and the resulting compounds did not induce vacuole formation (Fig. 1b; compound 10 and 13). In addition, other SNIPERs targeting CRABP23 and ERα did not induce cytoplasmic vacuolization6 (Fig. S1). We further derivatized the SNIPER(TACC3) by replacing bestatin moiety to MV1, another IAP ligand, and this compound induced vacuolization as well as SNIPER(TACC3)-1 and -2 (Fig. 1b; compound 19). However, substitution of bestatin with fluorescein isothiocyanate (FITC) lost the ability to induce vacuolization (Fig. 1b; compound 17). Notably, the compounds with the activity to induce vacuolization caused cell death (Fig 1c). These results suggest that conjugating KHS108 to IAP ligands is required for the induction of vacuolization and cell death. Hereafter, we mainly used SNIPER(TACC3)-2 in the following experiments.
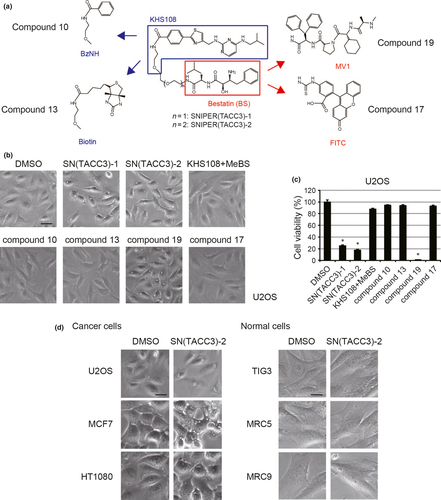
SNIPER(TACC3)-2 also induced cytoplasmic vacuolization in human breast carcinoma MCF7 and human fibrosarcoma HT1080 cells, but not in normal human fibroblast TIG3, MRC5 and MRC9 cells (Fig 1d), suggesting that SNIPER(TACC3) induces cytoplasmic vacuolization selectively in cancer cells.
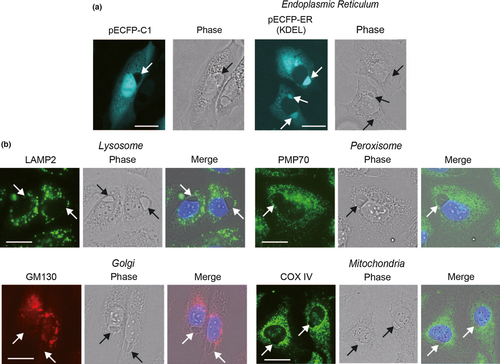
To investigate the origin of the vacuoles, we stained cells with a variety of organelle markers. The vacuole was not stained with LAMP2, PMP70, GM130 and COX IV, markers of lysosome, peroxisome, golgi apparatus and mitochondria, respectively, but clearly stained with ECFP-ER that has an ER localization signal (KDEL motif) (Fig. 2). These results strongly suggest that the vacuole is derived from ER.
SNIPER(TACC3) activates the X-linked inhibitor of apoptosis protein (XIAP)-mediated ubiquitylation and ER stress response selectively in cancer cells
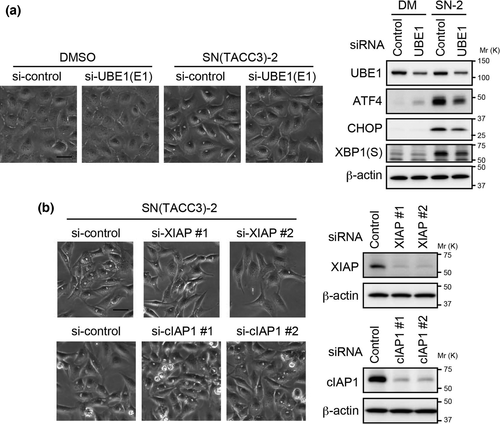
To investigate the mechanism by which SNIPER(TACC3) induces cytoplasmic vacuolization, the effect of siRNA-mediated gene silencing was examined. The SNIPER(TACC3)-2-induced cytoplasmic vacuolization was prevented by silencing of ubiquitin-activating enzyme 1 (UBE1) (Fig. 3a), indicating that the ubiquitylation system is required for the vacuolization. To clarify the requirement of an IAP ubiquitin ligase for the vacuolization, we also silenced IAPs. IAP antagonists, such as MV1, are known to bind to cIAP1, cIAP2 and XIAP.27-29 Since cIAP2 is not expressed in U2OS cells, we focused on cIAP1 and XIAP. The silencing of XIAP, but not cIAP1, suppressed cytoplasmic vacuolization by SNIPER(TACC3)-2 (Figs 3b and S2). These results suggest that the XIAP-mediated ubiquitylation is required for the SNIPER(TACC3)-induced vacuole formation.
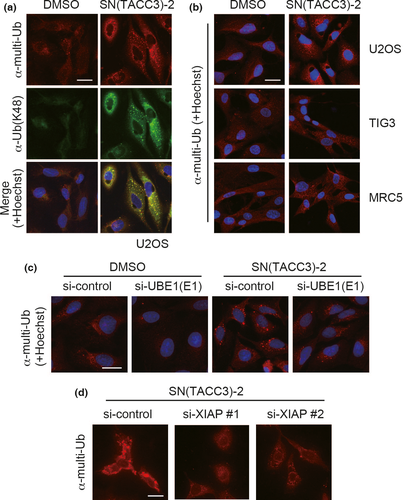
To examine if the ubiquitylation actually occurs in the SNIPER(TACC3)-treated cells, we immunostained the cells with antibodies against ubiquitin. Immunostaining with antibodies specific to multi-ubiquitin and K48-linked ubiquitin showed a punctate signal in the SNIPER(TACC3)-treated U2OS cells, suggesting that SNIPER(TACC3)-2 induces ubiquitylated protein aggregates in cytoplasm of U2OS cells (Fig. 4a). The ubiquitylated protein aggregates were not observed in normal fibroblasts TIG3 and MRC5 (Fig. 4b), indicating the selectivity to cancer cells. We then investigated the role of E1 and XIAP in the SNIPER(TACC3)-induced ubiquitylated protein aggregate formation. The silencing of UBE1 prevented the SNIPER(TACC3)-induced accumulation of ubiquitylated protein aggregates (Fig. 4c), which is consistent with the suppression of cytoplasmic vacuolization induced by SNIPER(TACC3) (Fig. 3a). In addition, XIAP silencing reduced the SNIPER(TACC3)-induced accumulation of ubiquitylated proteins (Fig. 4d), indicating that XIAP-mediated ubiquitylation takes place in the SNIPER(TACC3)-treated cells.
Since accumulation of ubiquitylated protein aggregates often causes ER stress in a variety of cell system,30, 31 we next examined ER stress responses in the SNIPER(TACC3)-treated cells. Consistent with the accumulation of ubiquitylated protein aggregates, SNIPER(TACC3)-2 induced the expression of activating transcription factor 4 (ATF4), C/EBP homologous protein (CHOP), and the spliced form of X-box binding protein-1 (XBP-1), mediators of ER-stress response, in U2OS cells, which were suppressed by E1 silencing (Fig. 3a). However, the ER stress responses were not observed in normal fibroblasts, TIG3 and MRC5 (Fig. 5a). To examine which ER-stress response pathway mediates the SNIPER(TACC3)-induced cytoplasmic vacuolization, we silenced ATF4, CHOP and XBP-1 in the cells. The silencing of XBP-1 repressed the SNIPER(TACC3)-2-induced vacuolization, while ATF4 and CHOP silencing did not (Fig. 5b), suggesting that XBP-1 plays an important role in mediating vacuole formation induced by SNIPER(TACC3)-2.
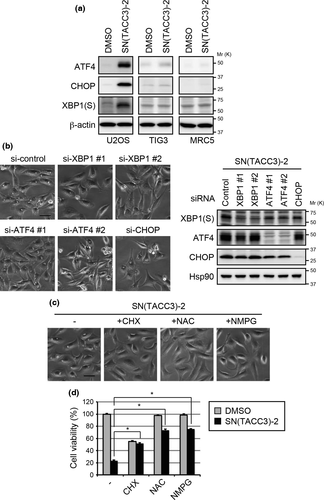
Cell death characterized by ER vacuolization accompanied by ER stress response and accumulation of ubiquitylated protein aggregates is known as paraptosis or PLCD,15, 16 and this type of cell death is often suppressed by a protein synthesis inhibitor and thiol antioxidants.16, 21-26 Consistent with these reports, the SNIPER(TACC3)-2-induced cytoplasmic vacuolization and cell death were also inhibited by co-treatment with cycloheximide (CHX) and thiol antioxidants, N-acetylcysteine (NAC) and N-(2-mercaptopropionyl)glycine (NMPG) (Fig. 5c,d). Necrosis (necroptosis) and oncosis also represent cell death with ER vacuolization, however, these types of cell death are not inhibited by CHX treatment.15, 16, 32, 33 Collectively, these results strongly suggest that SNIPER(TACC3) induces the accumulation of ubiquitylated protein aggregates mediated by XIAP, which causes ER stress and vacuole formation culminating in PLCD of cancer cells.
Combination of SNIPER(TACC3) and bortezomib
Bortezomib and MG132 induce ER stress by inhibiting proteasome, therefore, we next examined the combination of these drugs with SNIPER(TACC3) on the vacuole formation. As shown in Figure 6a, MG132 and bortezomib at 1 μM did not induce the vacuolization. However, they enlarged the size of vacuoles induced by 30 μM of SNIPER(TACC3)-2. They also induced vacuole formation when combined with 5, 10 and 20 μM of SNIPER(TACC3)-2 that scarcely induced vacuole formation by single treatments (Fig. 6a). These results suggest that proteasome inhibition enhances the SNIPER(TACC3)-induced vacuolization.
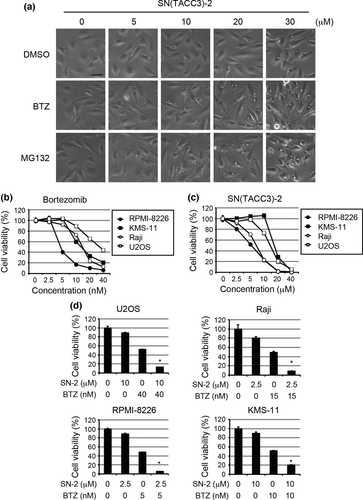
Since bortezomib is clinically used to treat multiple myelomas,34 we then evaluated the anticancer effects of SNIPER(TACC3)-2 in cancer cells including human multiple myeloma RPMI-8226 and KMS-11 cells, human Burkitt's lymphoma Raji cells and U2OS cells. The viability of these cancer cells were reduced by individual treatment of bortezomib and SNIPER(TACC3) in a dose-dependent manner (Fig. 6b,c). When these cancer cells were co-treated with suboptimal doses of bortezomib and SNIPER(TACC3), the viability was synergistically reduced (Fig. 6d). Thus, SNIPER(TACC3) sensitizes cancer cells to bortezomib.
Discussion
In our previous study, we developed SNIPER(TACC3)s that induces degradation of TACC3 protein via the ubiquitin-proteasome pathway.7 The SNIPER(TACC3) caused significant apoptosis in cancer cells expressing larger amount of TACC3 protein, however, caspase activation was not extensively observed.7 To understand how SNIPER(TACC3) induces cell death in cancer cells in more detail, we analyzed the SNIPER(TACC3)-treated cancer cells, and found that SNIPER(TACC3) also induces cytoplasmic vacuolization and PLCD selectively in cancer cells (Fig. 7). The SNIPER(TACC3)-induced degradation of TACC3 is important for induction of apoptosis in cancer cells.7 However, the downregulation of TACC3 is not likely to be involved in the induction of PLCD because the vacuolization was not blocked by siRNA-mediated knockdown of APC/CCDH1-components that plays an important role in the TACC3 degradation by SNIPER(TACC3) (Fig. S3) and siRNA-mediated knockdown of TACC3 did not induce cytoplasmic vacuolization (Fig. S4).
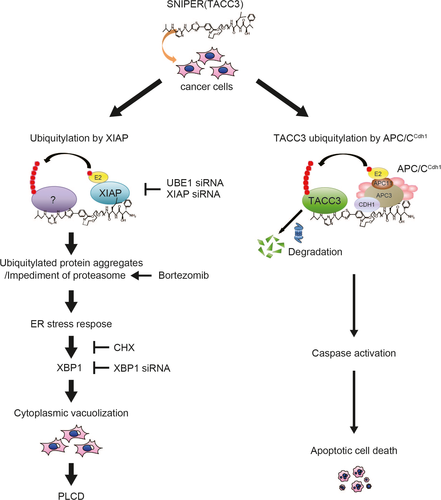
The vacuolization and PLCD were induced by both bestatin-based and MV-1-based SNIPER(TACC3)s, but substitution of the IAP-ligands to FITC abolished the activity, suggesting that IAPs play a role in the SNIPER(TACC3)-induced vacuolization. In line with this, silencing of XIAP suppressed the SNIPER(TACC3)-induced accumulation of the ubiquitylated protein aggregates and cytoplasmic vacuolization, indicating an indispensable role of XIAP in this process. Thus, SNIPER(TACC3) induces XIAP-mediated ubiquitylation, which results in the accumulation of ubiquitylated protein aggregates. Since the ubiquitylated protein aggregates often cause cytoplasmic vacuolization,21, 22, 35-37 the SNIPER(TACC3)-induced accumulation of ubiquitylated aggregates would results in the vacuolization as well. At present, the ubiquitylated proteins included in the aggregates were not clear. TACC3 was not found in the aggregates (data not shown) probably because most of the TACC3 protein is degraded in the cells.
Although the ubiquitylated proteins are not identified, the protein aggregates accumulated in the SNIPER(TACC3)-treated cells would cause ER-stress. Substantial and prolonged accumulation of misfolded proteins in the ER would bring about extensive ER swelling. XBP-1 was reported to induce ER expansion and ER biogenesis.38, 39 Consistent with these reports, the vacuoles induced by SNIPER(TACC3) are derived from ER, and the vacuolization requires expression of XBP-1. This evidence suggests that the suppression of SNIPER(TACC3)-induced vacuolization by CHX (Fig. 5c) could be attributed to the inhibition of XBP-1 expression (Fig. S5).
The SNIPER(TACC3)-induced cytoplasmic vacuolization and PLCD were observed in cancer cells but not in normal fibroblasts. Since cancer cells accumulate mutations in their genome, they produce more amounts of abnormal mutant proteins than normal cells, and therefore, cancer cells are constantly under an ER-stressed condition.40 In addition, new protein synthesis and thiol homeostasis are more essential for rapidly growing cancer cells than quiescent normal cells.21, 22, 41 This evidence could explain, at least in part, why SNIPER(TACC3) showed selectivity to cancer cells. In addition, the expression level of XIAP might be involved in the selectivity to cancer cells, because XIAP is overexpressed in a variety of cancer cells.42, 43
Bortezomib enhanced the SNIPER(TACC3)-induced vacuolization, and the combination treatment of bortezomib and SNIPER(TACC3) exhibited a synergistic anticancer activity against several cancer cell lines. Since SNIPER(TACC3) impedes ER-associated protein degradation (ERAD) system, a target of proteasome inhibitors, and induces ER stress responses, the susceptibility of cancer cells to bortezomib could be enhanced by SNIPER(TACC3). Combination of these would be effective to treat a variety of cancers represented by multiple myelomas, in which the ER is expanded to accommodate the synthesis of secretory immunoglobulin.44 Meanwhile, the SNIPER(TACC3)-induced PLCD was mediated by XIAP as described above, which is involved in the resistance to cancer therapy by inhibiting apoptosis.42, 43 Therefore, the induction of PLCD by SNIPER(TACC3) might be applied to treat cancers resistant to apoptosis by overexpression of XIAP.
Acknowledgments
The authors appreciate Dr. K. Okuhira for helpful discussions. We thank Dr. M. Tada for kindly providing CFP-ER plasmid. This work was supported in part by grants from Japan Society for the Promotion of Science (KAKENHI Grants 26860049 to N.O.; 16H05090 and 16K15121 to M.N.), Japan Agency for Medical Research and Development (AMED) (15ak0101029 h1402 and 16ak0101029j1403 to M.N.; 16cm0106124j0001 to N.O.), Ministry of Health and Labour Welfare (to M.N) and Takeda Science Foundation (to N.O.).
Disclosure Statement
K. Nagai, H. Nara and N. Cho are employees of Takeda Pharmaceutical Co., Ltd. M. Naito received a research fund from Takeda Pharmaceutical Company (Osaka, Japan). The other authors declare no conflict of interest.
Abbreviations
-
- APC/CCDH1
-
- anaphase-promoting complex/cyclosome with CDH1
-
- ATF4
-
- activating transcription factor 4
-
- CHOP
-
- C/EBP homologous protein
-
- CHX
-
- cycloheximide
-
- cIAP1
-
- cellular inhibitor of apoptosis protein 1
-
- CRABP2
-
- cellular retinoic acid-binding protein 2
-
- ERAD
-
- ER-associated protein degradation
-
- ER
-
- endoplasmic reticulum
-
- ERα
-
- estrogen receptor α
-
- FITC
-
- fluorescein isothiocyanate
-
- MeBS
-
- methyl-bestatin
-
- NAC
-
- N-acetylcysteine
-
- NMPG
-
- N-(2-mercaptopropionyl)glycine
-
- PLCD
-
- paraptosis-like cell death
-
- PROTAC
-
- Proteolysis Targeting Chimera
-
- SNIPER
-
- Specific and Nongenetic IAP-dependent Protein ERaser
-
- TACC3
-
- transforming acidic coiled-coil-3
-
- XBP-1
-
- X-box binding protein-1
-
- XIAP
-
- X-linked inhibitor of apoptosis protein