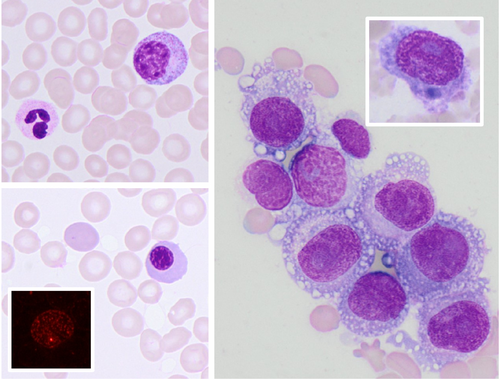
Metastatic melanoma presenting with leucoerythroblastic blood film
A 58-year-old male patient presented with abdominal pain, fever and cutaneous bleeding. Routine laboratory tests showed anaemia (haemoglobin concentration: 91.8 g/L), thrombocytopenia (platelet count: 24 × 109/L), haemolysis (haptoglobin: <10 g/L, lactate dehydrogenase: 7380 U/L), evidence of fibrinolysis (D-dimer: 4.1 mg/L, fibrinogen: 0.9 g/L) and acute kidney injury (glomerular filtration rate: 29 mL/min). A suspicion of thrombotic microangiopathy (PLASMIC score 5, intermediate risk) was promptly raised, and a peripheral blood film was performed to search for schistocytes. The blood film showed no evidence of schistocytes, but revealed a leucoerythroblastic reaction with reticulocytes, polychromatic erythroblasts (May–Grünwald–Giemsa staining, 60× objective; bottom left main panel) and coexistence of mature and immature granulocytes (top left). Reticulocytes were also readily detectable by immunofluorescence microscopy with immunostaining of the cytoskeletal protein non-muscular myosin IIa showing typical aggregates (bottom left, inset). A review of patient's medical history revealed a previous diagnosis of malignant melanoma treated with surgery 2 years earlier, with subsequent development of axillary lymph node and lung metastases during treatment with checkpoint inhibitor therapy. At presentation, the patient was receiving a combination chemotherapy with dabrafenib and trametinib targeting the BRAF and MEK genes. Bone marrow metastasis from melanoma was suspected, and a bone marrow aspiration and biopsy were performed. The aspiration revealed a diffuse infiltration of the bone marrow with large, vacuolated cells with large, open-chromatin nuclei and prominent nucleoli (May–Grünwald–Giemsa staining, 60× objective; right main panel). A small proportion of these cells displayed melanin pigment (upper right, inset). The cells were CD45-negative by flow cytometry, confirming their non-haematopoietic origin. A computed tomography scan revealed multiple hepatic metastases. The patient was treated palliative and died few days later.
The reported case reaffirms the importance of peripheral blood morphology, which can uniquely guide the diagnostic workup even in the era of precision medicine.
ACKNOWLEDGEMENT
Open Access funding enabled and organized by Projekt DEAL.