Prognostic significance of the Medical Research Council cytogenetic classification compared with the European LeukaemiaNet risk classification system in acute myeloid leukaemia
We compared the outcomes of patients with newly diagnosed, non-M3 acute myeloid leukaemia (AML) treated between 1993 and 2012 with available cytogenetic data based on the European LeukaemiaNet (ELN-C) and UK Medical Research Council classification (MRC-C) systems (Dohner et al, 2010; Grimwade et al, 2010). Patients <60 years were treated with idarubicin-based protocols (typically 12 mg/m2/d ×3) combined with high-dose cytarabine (1000–2000 mg/m2/d for 3–5 d); patients >60 years with non-favourable (FAV) cytogenetics were treated with lower-intensity programmes utilizing azacitidine, decitabine and novel agents. All protocols were approved by the Institutional Review Board and patients signed informed consents in accordance with the Declaration of Helsinki.
Patients with available cytogenetic data were classified according to the MRC-C (Grimwade et al, 2010). Patients with cytogenetic data and mutational status for the FLT3 and NPM1 genes were also grouped according to a modified ELN-C (Dohner et al, 2010). Biallelic CEBPA mutational analysis was not available for the majority of patients, and was not included in the current analysis. Although an important limitation, given the low incidence of biallelic CEBPA mutations (8–14%) in prior studies, the current analysis remains informative.
We examined the categorization and outcomes of patients according to the MRC-C and the ELN-C and compared the incidence of cytogenetic subgroups by age using the Wilcoxon–Mann–Whitney test and survival using the Kaplan–Meier method. Log-rank test was used to compare overall survival (OS) among subgroups of patients categorized by MRC-C or ELN-C. The C-index was computed to assess the discriminative ability of MRC-C and ELN-C for OS within age groups.
A total of 2070 patients, with a median age of 60 years (range, 12–89) were included (Table SI). The median follow-up was 37 months (0·6–135) and 1196 (55%) were male. Among all patients, 766 (37%) had a normal karyotype (Cytogenetically normal, CN), including 330 (34%) patients <60 years. Of the remainder, 27%, 10%, 5%, 3% and 17% of patients had 1, 2, 3, 4 or 5+ cytogenetic abnormalities, respectively. Patients (N = 1920, non-acute promyelocytic leukaemia) were first classified according to the MRC-C. As the MRC-C only included patients <60 years, those aged <60 years (N = 857) and ≥60 years (N = 1063) were analysed separately. The incidence of cytogenetic abnormalities overall and in those <60 years, along with the incidence reported by the MRC (Grimwade et al, 2010) are summarized in Table SII. In comparison to the MRC data, our cohort of patients (<60 years) had a significantly lower incidence of CN-AML (34% vs. 41%, P < 0·001) and a significantly higher incidence of del(5q), del(7q), t(9;11) and monosomies 5, 7, 12 and 17 (all P < 0·001).
Next, a subset of patients with available molecular data (N = 1026, 50%) were further analysed. These patients had a median follow-up of 25 months and a median age of 62 years (17–88), with 539 patients (53%) ≥60 years old. Of these, 199 (19%) were FLT3-ITD (+) and 114 (11%) were NPM1mut (+). Significantly more patients <60 years were classified as FAV and significantly more patients ≥60 years were classified as adverse (ADV, P < 0·001) (Fig 1A–D).
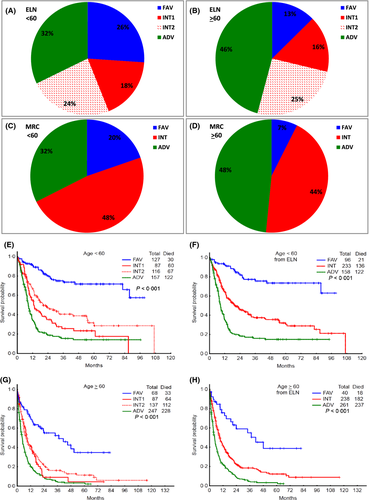
The outcomes of patients <60 and ≥60 years grouped by the ELN-C and MRC-C are shown in Fig 1E–H. The median OS, 5-year OS, and complete response rates are summarized in Tables SIII and SIV.
To assess the discriminative ability of each classification system for OS, we computed the C-index for the younger and older patients within each system. For patients ≥60 years, the C-index was 0·610 and 0·613 for the MRC-C and ELN-C, respectively. In contrast, for patients <60 years, the C-index was 0·659 and 0·674, for the MRC-C and ELN-C, respectively. This suggests that the two systems were similar in their discriminative ability for patients ≥60 years, but the ELN-C was more discriminative in patients <60 years.
We analysed how many patients changed prognostic categories upon reclassification by the ELN-C. Of the 419 patients classified as ADV by the MRC-C, 35 (8%) were reclassified as intermediate (INT)-2 by ELN-C. Of the 471 patients classified as INT by the MRC-C, 20 (4%) were reclassified as ADV, 59 (13%) reclassified as FAV, and the rest, as INT-1 (36%) and INT-2 (46%) (Table 1). All patients in the MRC-C FAV category remained FAV in the ELN-C (Table 1). Although we examined the outcomes, by age, of those that were reclassified to a new ELN group, the subgroups were too small to make meaningful conclusions. The median OS of these patients was either similar to the original MRC estimation, or intermediate between the two. However, in the larger group of patients (in both age groups) reclassified from MRC-INT to ELN-FAV, the median OS was significantly higher than their original classification and more in line with the expected outcome for ELN-FAV.
| Prognostic category | ELN-C | |||||
|---|---|---|---|---|---|---|
| Adverse | Intermediate-1 | Intermediate-2 | Favourable | Total | ||
| MRC-C | Adverse | 384 | 0 | 35 | 0 | 419 |
| Intermediate | 20 | 174 | 218 | 59 | 471 | |
| Favourable | 0 | 0 | 0 | 136 | 136 | |
| Total | 404 | 174 | 253 | 195 | 1026 | |
| Age ≥ 60 years | Adverse | Intermediate-1 | Intermediate-2 | Favourable | Total | |
|---|---|---|---|---|---|---|
| MRC-C | Adverse | 239 | 0 | 22 | 0 | 261 |
| Intermediate | 8 | 87 | 115 | 28 | 238 | |
| Favourable | 0 | 0 | 0 | 40 | 40 | |
| Total | 247 | 87 | 137 | 68 | 539 |
| Age < 60 years | Adverse | Intermediate-1 | Intermediate-2 | Favourable | Total | |
|---|---|---|---|---|---|---|
| MRC-C | Adverse | 145 | 0 | 13 | 0 | 158 |
| Intermediate | 12 | 87 | 103 | 31 | 233 | |
| Favourable | 0 | 0 | 0 | 96 | 96 | |
| Total | 157 | 87 | 116 | 127 | 487 |
- Bold, underlined figures indicate the number of patients that were re-classified.
To our knowledge, this is the first study that applied both the MRC-C and ELN-C to the same large cohort of AML patients and analysed their outcomes by each. We found that the ELN-C provided similar discriminatory ability as the MRC-C in patients ≥60 years, but was better able to discriminate prognostic subgroups in patients <60 years. However, in the subgroup of patients who were reclassified from MRC-INT to ELN-FAV (in both age groups), the availability of the FLT3 and NPM1 mutation data was able to identify a cohort (NPM1mut+/FLT3wt) with a FAV prognosis, with implications for treatment strategy (Schlenk et al, 2008).
The outcomes of our patients in each subgroup classified by the ELN-C are comparable to published reports of large validation studies (Rollig et al, 2011; Mrozek et al, 2012). Although the correlation was stronger for patients <60 years, this was also the case in patients ≥60 years, despite the heterogeneity of therapy in our cohort. The relative consistency of the ELN-C across three different cohorts of patients treated by three separate groups further validates its utility as an important prognostic tool.
Further determination of the prognostic significance of newly discovered genetic abnormalities in AML (Ley et al, 2013) will allow further refinement of classification systems for better risk-adapted treatment approaches and individualized therapy.
Acknowledgements
This research is supported in part by the National Institutes of Health through MD Anderson's Cancer Center Support Grant CA016672.
Author contribution
TMK, HK and FR designed the study and performed the research. TMK, FR, XW, MB and SP collected, analysed and interpreted the data. TMK, HK, GGM, GB, EJ, ND, NP, JC and FR contributed patients for the study. KP helped with haemato-pathologic and molecular analysis. TMK and FR wrote the manuscript with input from HK, JC, GGM, GB, KP, EJ, ND and NP. All authors approved the final manuscript.
Conflict of interest
The authors have no relevant conflicts of interest to disclose.




