Accelerometer-based sedentary time, light physical activity, and moderate-to-vigorous physical activity from childhood with arterial stiffness and carotid IMT progression: A 13-year longitudinal study of 1339 children
Abstract
Aims
We examined the longitudinal associations of sedentary time (ST), light physical activity (LPA), and moderate-to-vigorous PA (MVPA) from childhood with carotid-femoral pulse wave velocity (cfPWV), a measure of arterial stiffness and carotid intima-media thickness (cIMT).
Methods
We studied 1339 children, aged 11 years from Avon Longitudinal Study of Parents and Children, UK, followed up for 13 years. Accelerometer-based ST, LPA, and MVPA were assessed at ages 11, 15, and 24 years clinic visits. cfPWV and cIMT were measured with Vicorder and ultrasound, respectively, at ages 17 and 24 years.
Results
Among 1339 [56.4% female] participants, mean ST increased from ages 11 through 24 years, while mean LPA and MVPA decreased. Persistently high ST tertile from childhood was associated with increased cfPWV progression, effect estimate 0.047 m/s; [(95% CI 0.005 to 0.090); p = 0.030], but not cIMT progression. Persistently high LPA tertile category was associated with decreased cfPWV progression in males −0.022 m/s; [(−0.028 to −0.017); p < 0.001] and females −0.027 m/s; [(−0.044 to −0.010); p < 0.001]. Cumulative LPA exposure decreased the odds of progressively worsening cfPWV [Odds ratio 0.994 (0.994–0.995); p < 0.0001] and cIMT. Persistent exposure to ≥60 min/day of MVPA was paradoxically associated with increased cfPWV progression in males 0.053 m/s; [(0.030 to 0.077); p < 0.001] and females 0.012 m/s; [(0.002 to 0.022); p = 0.016]. Persistent exposure to ≥60 min/day of MVPA was inversely associated with cIMT progression in females −0.017 mm; [(−0.026 to −0.009); p < 0.001].
Conclusion
LPA >3 h/day from childhood may attenuate progressively worsening vascular damage associated with increased ST in youth.
1 INTRODUCTION
Arterial stiffness and carotid intima-media thickness (cIMT) have been associated with cardiometabolic morbidity and mortality.1-9 However, whether longitudinal exposure to physical activity (PA) and sedentary (ST) confers long-term vascular health benefits during growth from childhood until early adulthood is unclear.10-12 Due to the paucity of longitudinal accelerometer movement behavior measures in the pediatric population, findings of simulated replacements of ST with time spent in PA in relation to metabolic health have been employed in formulating PA guidelines.10, 11, 13 The sex-specific longitudinal effect of increased PA and increased ST on subclinical arteriosclerosis and atherosclerosis in the young population remains unclear and there is contrasting evidence regarding the benefits of movement or harm of exercise-mediated cardiovascular remodeling.10-12, 14, 15
The mechanism underlying the relationship between ST, light PA (LPA), and moderate-to-vigorous PA (MVPA) and arterial structure and function is not fully elucidated.11, 16-19 Increased ST from childhood through young adulthood has been strongly associated with increased inflammation, fat mass, and dyslipidemia and it was recently reported that higher inflammation in adolescence temporally preceded higher arterial stiffness and cIMT.20-22 It is, however, unclear whether increased ST from childhood independently associates with increased arterial stiffness and cIMT via an increased inflammatory and altered metabolic pathway. Therefore, we examined (1). the sex-based longitudinal associations of objectively measured ST, light PA (LPA), and moderate-to-vigorous PA (MVPA), from ages 11–24 years with changes in arterial stiffness and cIMT between ages 17–24 years, and (2). the mediating roles of glucose, insulin, high-sensitivity C-reactive protein, lipids, systolic blood pressure, and body composition in these relationships using data from the Avon Longitudinal Study of Parents and Children (ALSPAC) birth cohort, England, UK.
2 METHODS
2.1 Study cohort
Data were from the ALSPAC birth cohort, which investigates factors that influence childhood development and growth. Altogether, pregnant women resident in Avon, UK with expected dates of delivery from 1st April 1991 to 31st December 1992 were invited to take part in the study. The initial number of pregnancies enrolled is 14 541, of which there was a total of 14 676 fetuses. When the oldest children were approximately 7 years of age, an attempt was made to bolster the initial sample size with eligible cases who had failed to join the study originally resulting in 14 901 children alive at 1 year of age. Regular clinic visits of the children commenced at 7 years of age and are still ongoing into adulthood. Study data at 24 years of age were collected and managed using REDCap electronic data capture tools.23
In this study, of the 3862 participants with complete arterial measures at the age 17 years clinic visit, only 1339 participants had at least two timepoints valid ST, LPA, and MVPA measurements at either age 11, 15, or 24 years clinic visit and were eligible for analyses (Figure S1). The excluded participants who had one or no timepoint measure of ST and PA during the 13-year-long follow-up study had similar baseline characteristics with those included in the study (Table S1). Furthermore, 3233 participants with complete arterial measures at 17 years had at least one timepoint measure of valid ST, LPA, and MVPA accelerometer data, and analyses involving these participants are presented in the supplementary appendix.
Ethical approval for the study was obtained from the ALSPAC Ethics and Law Committee and the Local Research Ethics Committees. Informed consent for the use of data collected via questionnaires and clinics was obtained from participants following the recommendations of the ALSPAC Ethics and Law Committee at the time.24-26 Consent for biological samples has been collected in accordance with the Human Tissue Act (2004). Please note that the study website contains details of all the data that is available through a fully searchable data dictionary and variable search tool (http://www.bristol.ac.uk/alspac/researchers/our-data/).
2.2 Physical activity and sedentary time assessment
ST, LPA, and MVPA were assessed with ActiGraphTM (LLC, Fort Walton Beach, FL, USA) accelerometer worn on the hip for 7 consecutive days at 11- and 15-year clinic visits whereas at 24 years movement behavior was assessed using ActiGraph GT3X+ accelerometer device worn on the hip for four consecutive days.15, 21, 27 There is a strong absolute agreement between the Actigraph™ models intraclass correlation coefficient 0.99 (95% CI = 0.98–0.99) thus making it acceptable to use different models within a study.28 A valid day was defined as providing data for at least 10 h per day (excluding sequences of 10 or more minutes with consecutive zero counts) and children were only included in the analyses if they provided at least 3 valid days of recording. The devices capture movement in terms of acceleration as a combined function of frequency and intensity. Data are recorded as counts that result from summing postfiltered accelerometer values (raw data at 30 Hz) into 60-s epoch units. Data were processed using Kinesoft software, version 3.3.75 (Kinesoft), according to established protocol. Activity counts per minute threshold validated in young people was used to calculate the amount of time spent; MVPA, >2296 counts per minute (cpm); for LPA, 100–2296 cpm; and for ST, 0 – <100 cpm at ages 11 and 15 years, but 2020 cpm for the 24-year MVPA assessment.6, 29, 30 The Evenson cutpoint used in stratifying activity threshold has shown the best overall performance across all intensity levels and was suggested as the most appropriate cut point for youth.31, 32 Pearson bi-variate correlations (r) between cumulative ST and LPA are (−0.70), ST and MVPA (−0.33), LPA and MVPA (0.19), p-value <0.001 for all. These correlation matrices are similar to the report of meta-analysis of cross-sectional accelerometer studies.13 ST and LPA were grouped in tertiles as low-, middle-, and high-tertile categories. MVPA was classified according to PA guideline recommendations of <40 min/day as low (reference), 40 – <60 min/day as moderate, and ≥60 min/day as high.10 The 40 – <60 min/day of MVPA was based on the lowest tertile cutpoint (39.95 min) for MVPA in the total population. The cut point between the middle and highest MVPA tertile was 59.8 min/day in line with the current PA guideline.27
2.3 Anthropometry and body composition
Anthropometry (height and weight) of participants at ages 17 and 24 years was assessed in line with standard protocols and body mass index (BMI) was computed as weight in kilograms per height in meters squared.1, 29 Body composition (total fat mass, and lean mass) was assessed using a dual-energy X-ray absorptiometry scanner at 17 and 24 years as previously described.1, 2, 29 All participants had attained puberty at the baseline of the outcome measure at the 17-year clinic visit using a time (years) to age at peak height velocity objective assessment derived from Superimposition by Translation And Rotation mixed-effects growth curve analysis.29, 33 The participant's mother's socioeconomic status was grouped according to the 1991 British Office of Population and Census Statistics classification.34
2.4 Vascular phenotype
At ages 17 and 24 years, carotid-femoral pulse wave velocity, cfPWV, was computed from pressure waveforms obtained using the Vicorder device (Skidmore Medical, Bristol, UK) observing standard protocols as detailed earlier.1, 2, 29 All measurements were taken independently by one of two trained vascular technicians (interobserver mean difference 0.2 m/s, SD 0.1).2, 29 cIMT from the right and left common carotid arteries at 17 years was assessed by ultrasound using a linear 12-MHz transducer (Vivid7, GE Medical, Chicago, Illinois), and cIMT from the right and left common carotid arteries at 24 years was measured using an ultrasound machine (CardioHealth Panasonic and a 13.5 MHz linear array broadband transducer (probe; center frequency 9.0 MHz)).1, 29 All vascular measures at 17 and 24 years were extensive and rigorous as earlier described, interobserver variability for cIMT was assessed in a separate sample of 25 young adults (coefficient of variation: 4.4 ± 2.2%).1, 2, 6, 29 For our analysis, we computed the mean of the measurement of the right and left common carotid arteries as cIMT. We categorized participants according to the 90th percentile cutpoint of cfPWV and cIMT at baseline and follow-up to identify those at risk of target vascular organ damage.8 At age 17 years, the 90th percentile cutpoint for cfPWV and cIMT in males was 6.89 m/s and 0.54 mm, respectively, while among females it was 6.30 m/s and 0.53 mm, respectively. At age 24 years, the 90th percentile cutpoint for cfPWV and cIMT in males was 8.08 m/s and 0.65 mm, respectively, while among females it was 7.27 m/s and 0.64 mm, respectively.
2.5 Cardiometabolic and lifestyle factors
Heart rate and systolic and diastolic blood pressure were measured with Omron monitor at ages 17 and 24 years as previously detailed.1, 29 Using standard protocols, fasting blood samples at ages 17 and 24 years were collected, spun, and frozen at −80°C, and a detailed assessment of fasting glucose, insulin, high-sensitivity C-reactive protein, low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, and triglycerides has been reported (coefficient of variation was <5%).1, 2, 29, 35 Questionnaires to assess smoking behavior were administered at the 17 and 24-year clinic visits. A specific question regarding whether participants smoked in the last 30 days was used as an indicator of current smoking status. At the 17-year clinic visit, participants were briefly asked about their personal and family (mother, father, and siblings) medical history such as a history of hypertension, diabetes, high cholesterol, and vascular disease.
2.6 Statistical analysis
Cohort descriptive characteristics were summarized as means and standard deviation, medians and interquartile ranges, or frequencies and percentages. We explored sex differences using independent t-tests, Mann–Whitney U-tests, or Chi-square tests for normally distributed, skewed or dichotomous variables, respectively. Multicategory variables were analyzed using a one-way analysis of variance. Normality was assessed by histogram curve, quantile-quantile plot, and Kolmogorov–Smirnov tests. We conducted a logarithmic transformation of skewed variables and confirmed normality prior to further analysis. For all continuous variables “cumulative” refers to the average values over the repeated measures across follow-up visits.
We examined the separate associations of the 13-year ST, LPA, and MVPA progression (11 through 24 years) in categories with each of cfPWV and cIMT progression measured from ages 17 through 24 years using generalized mixed-effect model with identity link for repeated measures. The generalized linear mixed-effect model is robust for handling highly correlated variables such as ST and LPA. We selected a random effect variance component type and determined the effect of the predictor trajectory on the progression in repeated outcome measures and a random intercept modeled on the subject level. While the mixed-effect model assumes that the data are missing at random and is robust for accounting for missing data at follow-up, we elected to additionally conduct 20 cycles of multiple imputations to account for missing data, especially in the outcome follow-up measures. In this population, 20 cycles of multiple imputations have been shown to have a relative efficiency of over 98% in simulating real data.1, 2, 6, 36 The analysis strategy accounted for baseline ST, LPA, MVPA predictors, vascular outcomes, and covariates and their repeated measures. Model 1 was adjusted for time-varying covariates measured at both baseline and follow-up such as age, low-density lipoprotein cholesterol, insulin, triglyceride, high-sensitivity C-reactive protein, high-density lipoprotein cholesterol, heart rate, systolic blood pressure, glucose, fat mass, lean mass, smoking status, family history of hypertension/diabetes/high cholesterol/vascular disease, and socioeconomic status. Model 2 was an additional adjustment for ST, LPA, or MVPA depending on the predictor. Unadjusted regression variable plots between movement behaviors and vascular outcomes continuous variables were presented for males, and females, separately. The generalized mixed-effect model with logit link was used to examine the longitudinal associations between ST, LPA, and MVPA and the risk of progressive target vascular organ damage (90th percentile cutpoint of cfPWV and cIMT) from ages 17 through 24 years.
Mediating path analyses using structural equation models separately examined the mediating role of each of cumulative fasting glucose, insulin, low-density lipoprotein cholesterol, triglyceride, high-density lipoprotein cholesterol, high-sensitivity C-reactive protein, systolic blood pressure, total body fat mass, and lean mass on the longitudinal associations of each of cumulative ST, LPA, and MVPA with each of the progression in cfPWV and cIMT. The mediation analysis was conducted in line with the Guideline for Reporting Mediation Analyses of Randomized Trials and Observational Studies (AGReMA).37 The examined mediation mechanism between movement behavior and arterial indices is partly based on previous studies in which poor movement behavior has been associated with worse cardiometabolic indices and the latter associated with worse arterial function and structure.6, 10, 17, 20, 21, 27, 38, 39 Analyses were adjusted for sex, family history of hypertension/diabetes/high cholesterol/vascular disease, socioeconomic status, and time-varying covariates measured at both baseline and follow-up such as age, heart rate, smoking status, sedentary time, light physical activity, moderate-to-vigorous physical activity, fat mass, lean mass, insulin, glucose, high-sensitivity C-reactive protein, high density lipoprotein cholesterol, low density lipoprotein cholesterol, and triglyceride depending on the predictor or mediator.
The path models had three equations per regression analysis (Figure S2): the longitudinal associations of cumulative ST, LPA, or MVPA with cumulative glucose, insulin, lipids, high-sensitivity C-reactive protein, systolic blood pressure, or body composition (Equation 1); the longitudinal associations of cumulative glucose, insulin, lipids, high-sensitivity C-reactive protein, systolic blood pressure, or body composition with cumulative cfPWV and cIMT (Equation 2); and the longitudinal associations of cumulative ST, LPA or MVPA with cumulative cfPWV and cIMT (Equation 3, total effect), and Equation 3′(direct effect) accounted for the mediating role of cumulative glucose, insulin, lipids, high-sensitivity C-reactive protein, systolic blood pressure, and body composition on the longitudinal associations of cumulative ST, LPA or MVPA with cumulative cfPWV and cIMT. Each mediator was included in a separate model for each vascular outcome, resulting in 9 models for either cfPWV or cIMT. The proportion of mediating or suppressing roles was estimated as the ratio of the difference between Equation 3 and Equation 3′ or the multiplication of Equations 1 and 2 divided by Equation 3 and expressed in percentage. A mediating or indirect role is confirmed when there are statistically significant associations between (a) the predictor and mediator, (b) the predictor and outcome, (c) the mediator and outcome, and (d) the longitudinal association between the predictor and outcome variable was attenuated upon inclusion of the mediator.40
However, when the magnitude of the longitudinal association between the predictor and outcome is increased upon inclusion of a third variable, a suppression is confirmed.40 This means that suppression occurs when the mediational path has an opposite effect, that is, instead of a decrease in the point estimate of the direct effect between an exposure and an outcome in relation to the total effect, there is rather an increase in the direct effect above the total effect's point estimate.40 We considered a statistically significant mediation or suppression of <1% as minimal, and ≥1% as partial. Path analyses were conducted with 1000 bootstrapped samples.41, 42 Collinearity diagnoses were performed and accepted results with a variance inflation factor <5, considered differences and associations with a 2-sided p-value <0.05 as statistically significant, and made conclusions based on effect estimates and their confidence intervals (CI). We applied Sidak correction for multiple testing. Analyses involving 10% of a sample of 10 000 ALSPAC children at 0.8 statistical power, 0.05 alpha, and 2-sided p-value would show a minimum detectable effect size of 0.084 standard deviations if they had relevant exposure for a normally distributed quantitative variable or identify statistically significant a true relative risk of 1.29 to an exposure of 10% prevalence.43 All statistical analyses were performed using SPSS statistics software, Version 27.0 (IBM Corp, Armonk, NY, USA).
3 RESULTS
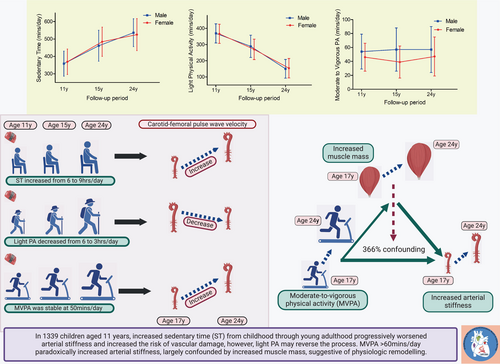
The cardiometabolic profiles of participants are described in Table 1, with males having higher muscle mass, height, and systolic blood pressure than females. However, females had higher ST from childhood through young adulthood, whereas males accumulated more MVPA minutes (Table 2 and Figure 1). Among 1339 [56.4% female] participants, mean ST increased from ages 11 through 24 years, while mean LPA and MVPA decreased. There was a significant decrease in accruing at least 60 min/day of MVPA from ages 11 years to 15 years in both male and female participants. Among males, 54%, 41%, and 41% accumulated ≥60 min/day of MVPA at ages 11, 15, and 24 years, respectively. Among females, 19%, 15%, and 28% accumulated ≥60 min/day of MVPA at ages 11, 15, and 24 years, respectively (Table 2). Other characteristics are described in Tables 1 and 2.
| Variables | 17 years | 24 years | ||||
|---|---|---|---|---|---|---|
| Male (n = 584) | Female (n = 755) | p-value | Male (n = 370) | Female (n = 599) | p-value | |
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |||
| Anthropometry | ||||||
| Age at clinic visit (years) | 17.70 (0.28) | 17.70 (0.30) | 0.875 | 24.61 (0.72) | 24.52 (0.74) | 0.045 |
| Height (m) | 1.79 (0.07) | 1.66 (0.06) | <0.0001 | 1.80 (0.07) | 1.66 (0.06) | <0.0001 |
| *Weight (kg) | 68.90 (14.20) | 60.30 (13.20) | <0.0001 | 77.70 (17.60) | 64.50 (18.33) | <0.0001 |
| Ethnicity-White (n, %) | 525 (95.8) | 675 (97.1) | 0.215 | NA | — | — |
| Body composition | ||||||
| *Total fat mass (kg) | 10.22 (10.46) | 19.15 (10.27) | <0.0001 | 18.05 (10.89) | 22.36 (13.18) | <0.0001 |
| Lean mass (kg) | 54.74 (6.05) | 37.90 (4.06) | <0.0001 | 56.69 (7.22) | 41.34 (5.21) | <0.0001 |
| *Body mass index (kg/m2) | 21.36 (3.89) | 21.91 (4.24) | 0.027 | 24.07 (4.90) | 23.45 (6.08) | 0.339 |
| Fasting plasma metabolic indices | ||||||
| High-density lipoprotein (mmol/L) | 1.20 (0.26) | 1.35 (0.31) | <0.0001 | 1.41 (0.38) | 1.66 (0.42) | <0.0001 |
| Low-density lipoprotein (mmol/L) | 2.00 (0.81) | 2.21 (0.66) | <0.0001 | 2.48 (0.81) | 2.42 (0.77) | 0.228 |
| *Triglyceride (mmol/L) | 0.74 (0.33) | 0.74 (0.35) | 0.749 | 0.86 (0.56) | 0.81 (0.48) | 0.001 |
| Glucose (mmol/L) | 5.16 (0.57) | 4.90 (0.35) | <0.0001 | 5.45 (0.44) | 5.24 (0.53) | <0.0001 |
| *Insulin (mU/L) | 5.87 (3.80) | 7.44 (4.01) | <0.0001 | 7.15 (5.50) | 8.00 (5.72) | 0.039 |
| *High-sensitivity C-reactive protein (mg/L) | 0.44 (0.58) | 0.64 (1.16) | <0.0001 | 0.63 (1.15) | 1.01 (2.26) | <0.0001 |
| Vascular measures | ||||||
| Heart rate (beat/mins) | 63 (10) | 67 (10) | <0.0001 | 64 (10) | 68 (10) | <0.0001 |
| Systolic blood pressure (mm Hg) | 120 (9) | 110 (8) | <0.0001 | 122 (10) | 112 (9) | <0.0001 |
| Diastolic blood pressure (mm Hg) | 63 (7) | 65 (6) | <0.0001 | 67 (8) | 66 (8) | 0.273 |
| Arterial measures | ||||||
| *Carotid-femoral pulse wave velocity (m/s) | 5.97 (0.85) | 5.47 (0.77) | <0.0001 | 6.42 (1.28) | 5.93 (1.10) | <0.0001 |
| *Carotid intima-media thickness (mm) | 0.48 (0.06) | 0.47 (0.05) | <0.0001 | 0.52 (0.10) | 0.52 (0.10) | 0.429 |
| Lifestyle factors | ||||||
| Smoked cigarette in the last 30 days (n, %) | 109 (20.8) | 160 (24.0) | 0.209 | 82 (22.5) | 140 (23.5) | 0.753 |
| Family history of H-D-C-V (n, %) | 167 (28.6) | 226 (29.9) | 0.628 | NA | — | — |
| Maternal social economic status (n, %) | — | — | 0.846 | NA | — | — |
| Professional | 21 (7.3) | 21 (6.3) | — | — | — | — |
| Managerial and technical | 115 (40.1) | 133 (39.8) | — | — | — | — |
| Skilled non-manual | 98 (34.1) | 116 (34.7) | — | — | — | — |
| Skilled manual | <5 (0.7) | 7 (2.1) | — | — | — | — |
| Partly skilled | 43 (15) | 49 (14.7) | — | — | — | — |
| Unskilled | 8 (2.8) | 8 (2.4) | — | — | — | — |
- Note: The values are means (standard deviations) and *median (interquartile range) except for lifestyle factors categories in percentage. Differences between sexes were tested using Student's t-test for normally distributed continuous variables, Mann–Whitney U-test for skewed continuous variables, Chi-square test for dichotomous variable, and analysis of covariance for multicategory variable. A 2-sided p-value <0.05 is considered statistically significant. H-D-C-V, hypertension, diabetes, high cholesterol, and vascular disease; NA, not available/applicable; p-value for sex differences.
| Age at follow-up | 11 years | 15 years | 24 years | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Male (n = 572) | Female (n = 733) | p-value | Male (n = 510) | Female (n = 603) | p-value | Male (n = 86) | Female (n = 174) | p-value | |
| Sedentary Time (mins/day; mean, SD) | 358 (72) | 369 (73) | 0.011 | 461 (89) | 484 (84) | <0.0001 | 536 (80) | 525 (92) | 0.348 |
| Light PA (mins/day; mean, SD) | 369 (59) | 366 (59) | 0.364 | 289 (69) | 270 (63) | <0.0001 | 150 (58) | 154 (60) | 0.593 |
| MVPA (mins/day; mean, SD) | 54 (25) | 46 (20) | <0.001 | 57 (31) | 39 (23) | <0.0001 | 57 (33) | 47 (28) | 0.010 |
| Cutpoints of tertile categories of ST | |||||||||
| Lowest to middle tertile (mins/day) | 326 | 340 | — | 425 | 452 | — | 505 | 483 | — |
| Middle to high tertile (mins/day) | 390 | 400 | — | 501 | 521 | — | 564 | 560 | |
| Cutpoints of tertile categories of LPA | |||||||||
| Lowest to middle tertile (mins/day) | 346 | 340 | — | 255 | 239 | — | 120 | 120 | — |
| Middle to high tertile (mins/day) | 393 | 391 | — | 316 | 290 | — | 169 | 166 | — |
| Categories of MVPA | <0.0001 | <0.0001 | 0.063 | ||||||
| MVPA <40 min /day (n, %) | 105 (18.4) | 304 (41.5) | — | 161 (31.6) | 342 (56.7) | — | 33 (38.4) | 82 (47.1) | — |
| MVPA 40 – <60 min/day (n, %) | 159 (27.8) | 287 (39.2) | — | 141 (27.6) | 168 (27.9) | — | 18 (20.9) | 43 (24.7) | — |
| MVPA ≥60 mins/day (n, %) | 308 (53.8) | 142 (19.4) | — | 208 (40.8) | 93 (15.4) | — | 35 (40.7) | 49 (28.2) | — |
- Note: The values are means (standard deviations) and MVPA categories in percentage. Differences between sexes were tested using Student's t-test for normally distributed continuous variables and analysis of covariance for multicategory variables. A 2-sided p-value <0.05 is considered statistically significant. p-value for sex differences. Statistically significant values are bolded.
- Abbreviations: LPA, light physical activity; MVPA, moderate-to-vigorous physical activity, ST, sedentary time.
3.1 Cumulative sedentary time with cfPWV and cIMT progression
Among females, persistent exposure to high and moderate tertile levels of ST from childhood was directly associated with increased cfPWV progression after full adjustment for cardiometabolic and lifestyle factors (Table 3). There were no statistically significant associations between cumulative tertiles categories of ST and cfPWV progression in males, and cIMT progression in the total cohort, males, or females (Table 3). Each minute increase in ST from ages 11–24 years was independently associated with an increased risk of progressively elevated cfPWV and cIMT in the total cohort (Table 3 and Figure 1). The unadjusted regression plot showed that an increasing ST from ages 11–24 years was associated with increased cfPWV and cIMT progression from ages 17–24 years in males, and females (Figures S3 and S4). Among 3233 participants with at least one accelerometer valid measure from ages 11–24 years, cumulative ST was associated with cfPWV but not cIMT progression after full adjustments (Table S2).
| Carotid-femoral pulse wave velocity (m/s) | Carotid intima-media thickness (mm) | |||
|---|---|---|---|---|
| β (95% CI) | p-value | β (95% CI) | p-value | |
| Males (n = 584) | ||||
| Sedentary time (lowest tertile) | ||||
| Reference | Reference | Reference | ||
| Sedentary time (middle tertile) | ||||
| Model 1 | 0.019 (−0.009 to 0.049) | 0.181 | 0.010 (−0.033 to 0.054) | 0.649 |
| Model 2 | 0.020 (−0.011 to 0.051) | 0.200 | 0.010 (−0.032 to 0.052) | 0.646 |
| Sedentary time (highest tertile) | ||||
| Model 1 | 0.015 (−0.014 to 0.044) | 0.310 | 0.021 (−0.006 to 0.048) | 0.129 |
| Model 2 | 0.016 (−0.014 to 0.046) | 0.296 | 0.022 (−0.006 to 0.050) | 0.131 |
| Females (n = 755) | ||||
| Sedentary time (lowest tertile) | ||||
| Reference | Reference | Reference | ||
| Sedentary time (middle tertile) | ||||
| Model 1 | 0.025 (−0.001 to 0.050) | 0.057 | 0.014 (−0.005 to 0.033) | 0.139 |
| Model 2 | 0.029 (0.001 to 0.057) | 0.041 | 0.016 (−0.001 to 0.033) | 0.062 |
| Sedentary time (highest tertile) | ||||
| Model 1 | 0.039 (−0.001 to 0.077) | 0.045 | 0.009 (−0.015 to 0.034) | 0.455 |
| Model 2 | 0.047 (0.005 to 0.090) | 0.030 | 0.013 (−0.008 to 0.034) | 0.225 |
| All participants (N = 1339) | ||||
| Elevated cfPWV (≥90th Percentile) | Elevated carotid IMT (≥90th Percentile) | |||
| (Mins/day) | Odds ratio (95% CI) | p-value | Odds ratio (95% CI) | p-value |
| Sedentary time | 1.001 (1.000 to 1.002) | 0.005 | 1.002 (1.001 to 1.002) | <0.001 |
- Note: Model 1 was adjusted for time-varying covariates measured at both baseline and follow-up such as age, low-density lipoprotein cholesterol, insulin, triglyceride, high-sensitivity C-reactive protein, high-density lipoprotein cholesterol, heart rate, systolic blood pressure, glucose, fat mass, lean mass, smoking status, family history of hypertension/diabetes/high cholesterol/vascular disease, and socioeconomic status. Model 2 was an additional adjustment for light physical activity and moderate-to-vigorous physical activity. Skewed covariates were logarithmically transformed. Regression coefficients effect estimates (β) were computed from the generalized mixed-effect model with identity link for repeated measures while the odds ratio was computed from generalized mixed-effect model with logit link for repeated measures. All participants' analyses were adjusted for sex and above above-listed covariates. CI, confidence interval. A 2-sided p-value <0.05 is considered statistically significant and are bolded. Multiple testing was corrected with Sidak correction. Multiple imputations were used to account for missing variables.
3.2 Cumulative light physical activity with cfPWV and cIMT progression
In males and females, persistent exposure to high-tertile levels of LPA from childhood was associated with decreased cfPWV progression after full adjustment for cardiometabolic and lifestyle factors (Table 4 and Figure 1). There were no statistically significant associations between the cumulative high-tertile category of LPA and cIMT progression in males, and females (Table 4). Each minute increase in LPA from ages 11–24 years was independently associated with a lower risk of progressively elevated cfPWV and cIMT in the total cohort (Table 4 and Figure 1). The unadjusted regression plot showed that cumulative LPA from ages 11–24 years was inversely associated with increased cfPWV and cIMT progression from ages 17–24 years in males, and females (Figures S3 and S4). Among 3233 participants with at least one accelerometer valid measure from ages 11–24 years, cumulative LPA was inversely associated with cfPWV and cIMT progression after full adjustments (Table S2).
| Carotid-femoral pulse wave velocity (m/s) | Carotid intima-media thickness (mm) | |||
|---|---|---|---|---|
| β (95% CI) | p-value | β (95% CI) | p-value | |
| Males (n = 584) | ||||
| Light PA (lowest tertile) | ||||
| Reference | Reference | Reference | ||
| Light PA (middle tertile) | ||||
| Model 1 | 0.030 (−0.010 to 0.070) | 0.146 | −0.006 (−0.013 to 0.001) | 0.117 |
| Model 2 | 0.030 (−0.013 to 0.074) | 0.172 | −0.003 (−0.008 to 0.001) | 0.122 |
| Light PA (highest tertile) | ||||
| Model 1 | −0.022 (−0.033 to −0.012) | <0.001 | −0.002 (−0.024 to 0.020) | 0.876 |
| Model 2 | −0.022 (−0.028 to −0.017) | <0.001 | 0.000 (−0.021 to 0.021) | 0.981 |
| Females (n = 755) | ||||
| Light PA (lowest tertile) | ||||
| Reference | Reference | Reference | ||
| Light PA (middle tertile) | ||||
| Model 1 | −0.009 (−0.032 to 0.014) | 0.422 | 0.003 (−0.013 to 0.019) | 0.687 |
| Model 2 | −0.007 (−0.030 to 0.015) | 0.526 | 0.001 (−0.014 to 0.016) | 0.892 |
| Light PA (highest tertile) | ||||
| Model 1 | −0.030 (−0.047 to −0.014) | <0.001 | 0.006 (−0.011 to 0.023) | 0.493 |
| Model 2 | −0.027 (−0.044 to −0.010) | 0.002 | 0.003 (−0.012 to 0.017) | 0.705 |
| All participants (N = 1339) | ||||
| Elevated cfPWV (≥90th percentile) | Elevated carotid IMT (≥90th percentile) | |||
| (Mins/day) | Odds ratio (95% CI) | p-value | Odds ratio (95% CI) | p-value |
| Light PA | 0.994 (0.994 to 0.995) | <0.0001 | 0.993 (0.993 to 0.994) | <0.0001 |
- Note: Model 1 was adjusted for time-varying covariates measured at both baseline and follow-up such as age, low-density lipoprotein cholesterol, insulin, triglyceride, high-sensitivity C-reactive protein, high-density lipoprotein cholesterol, heart rate, systolic blood pressure, glucose, fat mass, lean mass, smoking status, family history of hypertension/diabetes/high cholesterol/vascular disease, and socioeconomic status. Model 2 was an additional adjustment for sedentary time and moderate-to-vigorous physical activity. Skewed covariates were logarithmically transformed. Regression coefficients effect estimates (β) were computed from generalized mixed-effect model with identity link for repeated measures while the odds ratio was computed from generalized mixed-effect model with logit link for repeated measures. All participants' analyses were adjusted for sex and the above-listed covariates. CI, confidence interval; PA, physical activity. A 2-sided p-value <0.05 is considered statistically significant and are bolded. Multiple testing was corrected with Sidak correction. Multiple imputations were used to account for missing variables.
3.3 Cumulative moderate-to-vigorous physical activity with cfPWV and cIMT progression
Among males and females, persistent exposure to ≥60 min/day of MVPA from childhood through young adulthood was directly associated with increased cfPWV progression after full adjustment for cardiometabolic and lifestyle factors (Table 5 and Figure 1). Cumulative exposure to ≥60 min/day of MVPA from childhood was inversely associated with increased cIMT progression only in females (Table 5). Each minute increase in MVPA from ages 11–24 years was independently associated with a lower risk of progressively elevated cfPWV and cIMT in the total cohort (Table 5). The unadjusted regression plot showed that cumulative MVPA from ages 11–24 years was inversely associated with increased cfPWV and cIMT progression from ages 17–24 years in females but not among males (Figures S3 and S4). Among 3233 participants with at least one accelerometer valid measure from ages 11–24 years, cumulative MVPA was inversely associated with cIMT but not cfPWV progression after full adjustments (Table S2).
| Carotid-femoral pulse wave velocity (m/s) | Carotid intima-media thickness (mm) | |||
|---|---|---|---|---|
| β (95% CI) | p-value | β (95% CI) | p-value | |
| Males (n = 584) | ||||
| MVPA <40 min/day | ||||
| Reference | Reference | Reference | ||
| MVPA 40 – <60 min/day | ||||
| Model 1 | 0.041 (0.010–0.073) | 0.011 | −0.006 (0.044–0.032) | 0.754 |
| Model 2 | 0.041 (0.009–0.073) | 0.011 | −0.006 (−0.045–0.033) | 0.757 |
| MVPA ≥60 min/day | ||||
| Model 1 | 0.054 (0.031–0.076) | <0.001 | 0.007 (−0.009–0.023) | 0.371 |
| Model 2 | 0.053 (0.030–0.077) | <0.001 | 0.008 (−0.005–0.022) | 0.238 |
| Females (n = 755) | ||||
| MVPA <40 min/day | ||||
| Reference | Reference | Reference | ||
| MVPA 40 – <60 min/day | ||||
| Model 1 | −0.004 (−0.020–0.012) | 0.623 | −0.003 (−0.032–0.026) | 0.847 |
| Model 2 | −0.002 (−0.019–0.014) | 0.778 | −0.003 (−0.032–0.027) | 0.862 |
| MVPA ≥60 min/day | ||||
| Model 1 | 0.008 (−0.002–0.019) | 0.130 | −0.017 (−0.027 – −0.007) | 0.001 |
| Model 2 | 0.012 (0.002–0.022) | 0.016 | −0.017 (−0.026 – −0.009) | <0.001 |
| All participants (N = 1339) | ||||
| Elevated cfPWV (≥90th percentile) | Elevated carotid IMT (≥90th percentile) | |||
| (Mins/day) | Odds ratio (95% CI) | p-value | Odds ratio (95% CI) | p-value |
| MVPA | 1.002 (1.000–1.004) | 0.025 | 1.003 (1.001–1.005) | <0.001 |
- Note: Model 1 was adjusted for time-varying covariates measured at both baseline and follow-up such as age, low-density lipoprotein cholesterol, insulin, triglyceride, high-sensitivity C-reactive protein, high-density lipoprotein cholesterol, heart rate, systolic blood pressure, glucose, fat mass, lean mass, smoking status, family history of hypertension/diabetes/high cholesterol/vascular disease, and socioeconomic status. Model 2 was an additional adjustment for sedentary time and light physical activity. Skewed covariates were logarithmically transformed. Regression coefficients effect estimates (β) were computed from the generalized mixed-effect model with identity link for repeated measures while the odds ratio was computed from generalized mixed-effect model with logit link for repeated measures. All participants' analyses were adjusted for sex and the above-listed covariates. CI, confidence interval; MVPA, moderate-to-vigorous physical activity. A 2-sided p-value <0.05 is considered statistically significant and are bolded. Multiple testing was corrected with Sidak correction. Multiple imputations were used to account for missing variables.
3.4 Mediation effect of glucose, insulin, lipids, inflammation, blood pressure, and body composition on the associations of lipids with cfPWV and cIMT
Cumulative triglyceride partly mediated the associations of the cumulative increase in ST with increased cfPWV (3.4% mediation effect), but increased fat mass and lean mass suppressed the association by 3.6 and 9.6%, respectively (Table S3). Cumulative triglyceride, high-density lipoprotein cholesterol, and fat mass partly mediated the associations of the cumulative increase in ST with increased cIMT (1.3–1.7% mediation effect), but increased low-density lipoprotein cholesterol and lean mass partly suppressed the association by 2.6 and 2.1%, respectively (Table S3). All other mediators had no statistically significant mediating effect.
Cumulative fat mass partly mediated the associations of the cumulative LPA with increased cfPWV (1.2% mediation effect; Table S4). Cumulative low-density lipoprotein cholesterol and fat mass partly mediated the associations of the cumulative LPA with increased cIMT (1.2% mediation effect), but increased high-density lipoprotein cholesterol and fat mass partly suppressed the association by 1.3 and 1.2%, respectively (Table S4). All other mediators had no statistically significant mediating effect.
Cumulative low-density lipoprotein cholesterol and triglyceride partly suppressed the associations of the cumulative MVPA with increased cfPWV (3.4–4.5% mediation effect), but increased lean mass fully attenuated the associations of cumulative MVPA with increased cfPWV to statistical non-significance with a potential suppression effect of 366% (Table 6 and Figure 1). Cumulative low-density lipoprotein cholesterol and triglyceride partly mediated the associations of the cumulative MVPA with increased cIMT (7.5–9.6% mediation effect), but increased high-density lipoprotein cholesterol, high-sensitivity C-reactive protein, and lean mass partly suppressed the association by 16.3, 5.7 and 13.3%, respectively (Table 6). All other mediators had no statistically significant mediating effect.
| N = 1339 | Carotid-femoral pulse wave velocity progression from ages 17–24 years | ||||||
|---|---|---|---|---|---|---|---|
| Moderate-to-vigorous physical activity | Total effect | Direct effect | Indirect effect | Mediation or suppression (%) | |||
| Mediators | β (95% CI) | p-value | β (95% CI) | p-value | β (95% CI) | p-value | |
| Glucose | 0.077 (0.041–0.113) | 0.003 | 0.076 (0.042–0.113) | 0.002 | 0.001 (−0.006–0.010) | 0.827 | 1.3 |
| Insulin | 0.090 (0.052–0.126) | 0.003 | 0.089 (0.052–0.125) | 0.002 | 0.001 (0.000–0.004) | 0.142 | 1.1 |
| LDL-cholesterol | 0.089 (0.054–0.125) | 0.003 | 0.093 (0.057–0.129) | 0.003 | −0.004 (−0.008 – −0.001) | 0.004 | 4.5 suppression |
| Triglyceride | 0.089 (0.052–0.124) | 0.003 | 0.092 (0.056–0.127) | 0.003 | −0.003 (−0.007–0.000) | 0.035 | 3.4 suppression |
| HDL-cholesterol | 0.083 (0.046–0.119) | 0.002 | 0.083 (0.046–0.119) | 0.003 | 0.000 (−0.002–0.003) | 0.887 | 0 |
| High-sensitivity CRP | 0.087 (0.048–0.122) | 0.003 | 0.085 (0.047–0.120) | 0.003 | 0.001 (−0.001–0.005) | 0.158 | 11.5 |
| Systolic blood pressure | 0.041 (0.006–0.075) | 0.013 | 0.046 (0.010–0.081) | 0.010 | −0.006 (−0.015–0.003) | 0.226 | 14.6 |
| Fat mass | 0.084 (0.047–0.122) | 0.003 | 0.085 (0.047–0.123) | 0.003 | 0.000 (−0.005–0.002) | 0.641 | 0 |
| Lean mass | 0.006 (−0.029–0.043) | 0.775 | −0.016 (−0.050–0.019) | 0.347 | 0.022 (0.015–0.030) | 0.002 | 366.6 |
| Carotid intima-media thickness progression from ages 17–24 years | |||||||
| Glucose | −0.067 (−0.104 – −0.027) | 0.002 | −0.068 (−0.105 – −0.023) | 0.003 | 0.001 (−0.006–0.011) | 0.807 | 1.5 |
| Insulin | −0.047 (−0.085 – −0.007) | 0.021 | −0.050 (−0.089 – −0.008) | 0.015 | 0.002 (−0.001–0.007) | 0.217 | 4.3 |
| LDL-cholesterol | −0.053 (−0.091 – −0.011) | 0.010 | −0.048 (−0.087 – −0.004) | 0.028 | −0.005 (−0.010 – −0.002) | 0.001 | 9.4 mediation |
| Triglyceride | −0.053 (−0.091 – −0.012) | 0.010 | −0.049 (−0.087 – −0.008) | 0.014 | −0.004 (−0.008–0.000) | 0.035 | 7.6 mediation |
| HDL-cholesterol | −0.043 (−0.080 – −0.003) | 0.035 | −0.050 (−0.086 – −0.009) | 0.015 | 0.007 (0.003–0.011) | 0.001 | 16.3 suppression |
| High-sensitivity CRP | −0.053 (−0.093 – −0.012) | 0.009 | −0.057 (−0.095 – −0.014) | 0.006 | 0.003 (0.001–0.008) | 0.015 | 5.7 suppression |
| Systolic blood pressure | −0.081 (−0.119 – −0.039) | 0.002 | −0.079 (−0.115 – −0.038) | 0.002 | −0.003 (−0.008–0.001) | 0.211 | 3.7 |
| Fat mass | −0.039 (−0.077–0.004) | 0.079 | −0.032 (−0.071–0.008) | 0.096 | −0.007 (−0.013–0.000) | 0.029 | 17.9 |
| Lean mass | −0.113 (−0.151 – −0.069) | 0.002 | −0.127 (−0.165 – −0.080) | 0.003 | 0.015 (0.010–0.021) | 0.002 | 13.3 suppression |
- Note: Mediation structural equation model was adjusted for sex, family history of hypertension/diabetes/high cholesterol/vascular disease, socioeconomic status, and time-varying covariates measured at both baseline and follow-up such as age, heart rate, smoking status, sedentary time, light physical activity, fat mass, lean mass, insulin, glucose, high-sensitivity C-reactive protein, high-density lipoprotein cholesterol, and triglyceride depending on the predictor or mediator. β is standardized regression coefficient. p-value <0.05 was considered statistically significant and are bolded. When the magnitude of the longitudinal association between the predictor and outcome is increased upon inclusion of a third variable, a suppression is confirmed, However, when decreased it is mediation.
4 DISCUSSION
This is the largest prospective single birth cohort study that examined the role of objectively measured movement behavior from childhood through young adulthood on repeated measures of arterial stiffness, assessed using cfPWV, and cIMT progression from adolescence until young adulthood. We observed that persistent highest ST tertile over a 13-year period was directly associated with increased cfPWV progression over a 7-year period, but not cIMT progression. Moreover, persistent exposure to the highest LPA tertile was inversely associated with increased cfPWV progression but not cIMT progression. Paradoxically, cumulative exposure to MVPA was associated with increased cfPWV progression. Our results buttress existing evidence on the importance of movement behavior and provide novel information regarding the potential for attenuating subclinical arteriosclerosis and atherosclerosis before mid-life. Thus, significantly lowering mid-and high-tertile ST levels and increasing the high-tertile LPA category from childhood could mitigate the burden of cardiovascular morbidities and mortality in adulthood.
4.1 Cumulative sedentary time with cfPWV and cIMT progression
Longitudinal evidence on the role of accelerometer-measured ST on altered arterial function and structure is grossly lacking in the pediatric population.12 Majority of studies in this population have focused on the detrimental effects of ST on metabolic, adiposity, and blood pressure risks.10, 11, 13 However, arterial stiffness and cIMT progression have been associated with cardiovascular morbidity and mortality in adulthood, necessitating studies on the role of movement behavior on arterial health.3-5, 44 Arterial stiffness is a strong risk factor for elevated blood pressure and hypertension, insulin resistance, adiposity, metabolic syndrome, premature cardiac damage in adolescents and young adults.1, 2, 7, 9, 44 The present finding establishes that persistent exposure to high ST tertiles strongly predicts increased arterial stiffness progression, independent of cardiometabolic and lifestyle risk factors, especially in females. A cross-sectional study conducted among 1259 Brazilian young adults with a mean age of 30 years reported that only the highest quartile of ST (>12 h/day) was associated with higher cfPWV.45 Another cross-sectional study conducted among 658 Swedish young adults with a mean age of 22 years, reported no association between 8 and 10 h/day of ST and cfPWV.46 A recent cross-sectional study conducted among 1574 British adolescents age 15–17 years reported no association between 8 h/day of ST and cfPWV.47 However, in the present prospective study, both the middle and highest ST tertile were longitudinally associated with increased arterial stiffness progression. The cutpoint for the lowest ST tertile category was circa 6 h/day at age 11 years, 7 h/day at age 15 years, and 8 h/day at age 24 years. Among adults, a higher risk of death has been reported for ST ≥9.5 h/day.48
Males had ca. 10–20 min less ST compared to females at ages 11- and 15 years assessments, which could explain why cumulative ST was not associated with increased arterial stiffness progression in males, after accounting for cardiometabolic covariates, and additionally for time spent in LPA and MVPA. Therefore, as strongly recommended in the latest World Health Organization guidelines based mainly on cross-sectional evidence, children and adolescents should limit the amount of time spent being sedentary,10 and according to our findings, possibly below 6 h/day. The recommendation10 that undertaking more MVPA could reduce the detrimental effects of high levels of ST may not be effective in attenuating arterial stiffness progression, based on our observation since accounting for cumulative LPA and MVPA had minimal effect on the relationship. On the contrary, the positive associations between cumulative ST and subclinical atherosclerosis were significantly attenuated after controlling for cardiometabolic and lifestyle risk factors. It is known that dyslipidemia from childhood is strongly associated with increased subclinical atherosclerosis,6 premature cardiac damage,49 and cardiovascular mortality.50 This suggests that the detrimental effects of ST on subclinical atherosclerosis may be exerted via a cardiometabolic pathway.6, 10, 13 However, we observed a <4% partial mediating effect of individual cardiometabolic factors on the association of ST with cIMT warranting further experimental studies.
4.2 Cumulative light physical activity with cfPWV and cIMT progression
The 2020 World Health Organization guidelines did not specifically mention LPA for children and adolescents due to a lack of evidence.12 LPA is important from a public health perspective since it is more likely to be engaged in LPA for longer periods and easier to accumulate for those unaccustomed to being active or with low fitness in contrast to MVPA.10, 12, 48, 51 Increasing knowledge about the health benefits of LPA in the young population may potentially promote understanding of the extent to which substituting ST with LPA impacts health.12, 21, 22, 27, 51 Previous isotemporal substitution analyses conducted in a mostly cross-sectional design favored MVPA over LPA as the movement behavior to reverse ST's detrimental effect on cardiometabolic health.13 However, our longitudinal study revealed that the cumulative high-tertile category of LPA from childhood was inversely associated with increased arterial stiffness progression, thereby partly filling this knowledge gap. At age 11 years, participants spent 6-fold more time in LPA than MVPA, which reduced to 5-fold and 3-fold by 15 and 24 years, respectively. This large amount of time spent in LPA may explain its independent effect on attenuating arterial stiffness progression even after adjusting for cardiometabolic and lifestyle factors. The high inverse correlation between ST and LPA may suggest that time in LPA may be useful in reversing the detrimental effect of ST on health. Our findings in the young population extend the evidence already confirmed among adults that LPA is inversely associated with arterial stiffness.52 While the unadjusted regression plots showed inverse associations between cumulative LPA and cIMT progression, the fully adjusted model had no significant association in the whole cohort, among males and females participants who had at least 2 timepoint valid accelerometer measurements. The significant decline in LPA during the 13-year follow-up period may partly explain this finding. Nonetheless, subclinical atherosclerosis progression may not be attenuated by recommending increased LPA alone, the reduction in adverse cardiometabolic and lifestyle risk factors may have important roles.6, 53, 54
4.3 Cumulative moderate-to-vigorous physical activity with cfPWV and cIMT progression
There is conflicting evidence on the role of exercise and vascular remodeling in humans and the balance of benefit and harm remains disputed.14 A prospective study conducted among 254 children aged 8–10 years and followed up for 6 years, concluded that Actigraph-based MVPA was not associated with arterial stiffness and cIMT.55 Recently, a randomized control trial conducted among 203 hypertensive young adults aged 27 years concluded that moderate-to-high-intensity aerobic exercise did not improve arterial stiffness, at 16 and 52 weeks after the intervention.56 The present prospective study with a larger and longer follow-up with repeated arterial stiffness and cIMT measures showed that accruing ≥60 min/day of MVPA was associated with increased arterial stiffness progression in males and females but inversely associated with subclinical atherosclerosis progression in females. The mediation analyses revealed that increased lean mass may fully explain the paradoxical relationship between MVPA and increased cfPWV. Increased lean mass from childhood is a driver of physiologic arterial remodeling and exercise has been associated with increased muscle mass.29 These paradoxical findings between higher MVPA and higher arterial stiffness have been reported in strength-trained young male athletes and long-distance marathon runners.14, 16, 57-59
An increase in plasma norepinephrine concentrations may result in a chronic increase in sympathetic adrenergic vasoconstrictor tone within the arterial vessel.14, 16, 58, 60 Moreover, chronic vascular remodeling from repetitive wall strain and stress could occur due to protracted elevations in heart rate, cardiac output, and blood pressure from sustained high-intensity exercise.14, 16, 58-61 Intense exercise results in the mass production of free radicals that overwhelm the body's buffering capacity thus occasioning susceptibility to oxidative stress, atherogenesis, and endothelial dysfunction.59-62 Regional increases in blood flow during exercise, in synchrony with the metabolic demand of skeletal muscle, have been associated with training-induced arterial remodeling.63 The present study provides additional evidence on the relative impact of different exercise modality on vascular structure and function remodeling14 but confirmation of these findings are warranted in other pediatric cohorts. In a recent meta-analysis conducted among adults, it was reported that MVPA >24 min/day may be the threshold value for maximal risk reduction of all-cause mortality.48 In a recent cross-sectional study, accelerometer-measured MVPA was associated with higher left ventricular mass in 540 adolescents.15
It is not completely understood when MVPA-induced physiologic vascular remodeling, transit to pathological changes in the young population. Exercise-induced vascular remodeling involves angiogenesis, that is, formation of new capillaries from existing capillaries, and arteriogenesis.14, 19 Arteriogenesis refers to arterialization of capillaries (i.e., envelopment with smooth muscle and fibroblasts) leading to arterioles formation that enlarges further to become functioning conduit vessels.19 In the present study cumulative MVPA was associated with the odds of progressively elevated cfPWV and cIMT, derived from ≥90th percentile cutpoints. The 90th percentile has previously been employed as a cut point for possible target vascular organ damage.8 Moreover, studies in adults have shown that MVPA over a certain threshold may increase the risk of adverse cardiovascular events.48 This could be attributed to age-related divergent angiogenic behavior in body composition and growth and endocrine factors. Nonetheless, further experimental studies are needed to understand the lifelong impact of MVPA on vascular function and structure. Of note, accruing ≥60 min/day of MVPA was inversely associated with subclinical atherosclerotic progression in females but not in males. This is rather surprising since females spent a significantly lower amount of time in MVPA compared to males. Nonetheless, in the expanded cohort involving 3233 participants with at least one timepoint valid accelerometer measurement, cumulative MVPA was inversely associated with increased cIMT progression.
It was recently shown that increased lipid indices such as elevated cholesterol and triglyceride levels contribute to cIMT progression and premature cardiac damage in youth.6, 49 Another study reported engaging in both LPA and MVPA reduced lipid levels.22 Thus, in consonance with the mediation analysis where triglyceride (7.6%) and LDL-c (9.4%) independently mediated the inverse association between MVPA and cIMT, a potential explanatory mechanism is that MVPA may lower cIMT by decreasing lipid levels.22
4.4 Strength and limitation
The ALSPAC birth cohort provides an extensive array of gold-standard and repeated measures of variables from childhood through young adulthood which allowed us to fill knowledge gaps recently recommended as movement behavior research priority.10-13 Tertile categorization of predictors enable in between individual analyses, while continuous variable analyses present within-individual analyses and using both continuous and categorical variable in this study either in the mediation analyses or generalized linear mixed-effect model analyses comprehensively addressed alteration in both individual's group-based behavior change. We cannot exclude unmeasured or residual confounders, for instance, different equipment used during the 13-year follow-up period, such as uniaxial activity measures at ages 11 and 15 years and more sensitive triaxial activity measures at 24 years. A 60-s epoch may underestimate MVPA and reclassify as more LPA since children typically perform activity in shorter bouts, nonetheless, the highest averaged MVPA mins/day was accrued at age 11 years. The significant decrease in participants available at age 24 years clinic visit especially in males was due to less than one-third of the ALSPAC cohort being invited to participate in a subset study. This could potentially create a female-driven result in the total cohort, hence, the findings should be interpreted cautiously. Our study participants were mostly Caucasian with minimal geographic variations; thus, the findings may not be generalizable to other ethnicities. Lastly, the observational nature of our study may not establish causality but provide stronger evidence for future health guidelines in the pediatric population.
5 CONCLUSION
Persistently high ST tertiles from childhood through young adulthood was associated with worsening arterial stiffness progression whereas persistently high LPA tertile was associated with arterial stiffness regression. Cumulative LPA decreased the odds of premature vascular functional and structural damage. There were no associations of high ST and LPA with cIMT progression. Persistent engagement in MVPA of ≥60 min/day from childhood through young adulthood was associated with increased arterial stiffness progression, an “MVPA Paradox” possibly related to a concurrent increase in lean mass. Decreasing ST to <6 h/day while increasing LPA to >3 h/day in early life could independently attenuate worsening arterial stiffness progression; however, accruing ≥60 min/day of MVPA may attenuate subclinical atherosclerosis via the reduction in lipid indices.
AUTHOR CONTRIBUTIONS
Andrew O. Agbaje: Conceptualization; investigation; funding acquisition; writing – original draft; methodology; validation; visualization; writing – review and editing; software; formal analysis; project administration; data curation; supervision; resources. Alan R. Barker: Writing – review and editing; visualization. Adam J. Lewandowski: Visualization; writing – review and editing. Paul Leeson: Visualization; writing – review and editing. Tomi-Pekka Tuomainen: Writing – review and editing; visualization.
ACKNOWLEDGMENTS
We are extremely grateful to all the families who took part in this study, the midwives for their help in recruiting them, and the whole ALSPAC team, which includes interviewers, computer and laboratory technicians, clerical workers, research scientists, volunteers, managers, receptionists and nurses.
FUNDING INFORMATION
The UK Medical Research Council and Wellcome (Grant ref: 217065/Z/19/Z) and the University of Bristol provide core support for ALSPAC. The British Heart Foundation grant (CS/15/6/31468) funded blood pressure, carotid-femoral pulse wave velocity, and Actigraph activity monitoring device measurement at 24 years. The Medical Research Council grant (MR/M006727/1) supported smoking data collection. A comprehensive list of grant funding is available on the ALSPAC website (http://www.bristol.ac.uk/alspac/external/documents/grant-acknowledgements.pdf); Dr Agbaje's research group (UndeRstanding FITness and Cardiometabolic Health In Little Darlings: urFIT-child) was funded by the Jenny and Antti Wihuri Foundation (Grant no: 00180006), the North Savo regional and central Finnish Cultural Foundation (Grants no: 65191835, 00200150 and 00230190), Orion Research Foundation sr, Aarne Koskelo Foundation, Antti and Tyyne Soininen Foundation, Paulo Foundation, Paavo Nurmi Foundation, Yrjö Jahnsson Foundation (Grant no: 20217390), Ida Montin Foundation (Grant no: 20230289), Eino Räsänen Fund, Matti and Vappu Maukonen Fund, Kuopio University Foundation, Finnish Foundation for Cardiovascular Research (Grant no: 220021 and 230012) and the Alfred Kordelin Foundation (230082). The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
CONFLICT OF INTEREST STATEMENT
None.
CONSENT FOR PUBLICATION
Informed consent for the use of data collected via questionnaires and clinics was obtained from participants.
Open Research
DATA AVAILABILITY STATEMENT
The informed consent obtained from ALSPAC participants does not allow the data to be made freely available through any third-party maintained public repository. However, data used for this submission can be made available on request to the ALSPAC Executive. The ALSPAC data management plan describes in detail the policy regarding data sharing, which is through a system of managed open access. Full instructions for applying for data access can be found here: http://www.bristol.ac.uk/alspac/researchers/access/. The ALSPAC study website contains details of all the data that are available (http://www.bristol.ac.uk/alspac/researchers/our-data/).