Norwegian parents avoid placing infants in prone sleeping positions but frequently share beds in hazardous ways
Funding information
This study did not receive any specific funding.
Abstract
Aim
Campaigns to prevent prone sleeping and other modifiable risk factors have greatly reduced the incidence of sudden infant death syndrome in Norway. Sleep-related infant deaths still occur sporadically and may be preventable. We studied infants’ sleeping environments and whether parents followed safe sleep recommendations.
Methods
Parents with infants up to 12 months of age were invited to complete an online questionnaire from May to December 2018. It was publicised by health centres and on websites and social media.
Results
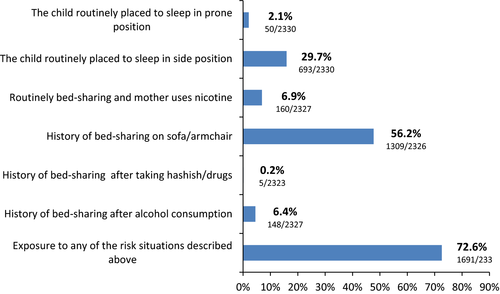
We received 4886 responses and 4150 met the age criteria and were included. Just under two-thirds (62.7%) reported routine bed-sharing, and this practice was associated with increased nocturnal breastfeeding, single parents and having more than one child. A small number of infants under six months were occasionally placed prone when they were laid down to sleep (2.1%) and 29.7% were placed on their side. Nearly three-quarters (72.6%) of the 2330 parents with infants under six months of age reported previous high-risk behaviour, such as sleeping together on a sofa or bed-sharing after smoking or drinking.
Conclusion
Norwegian parents rarely used prone sleeping positions for infants. However, bed-sharing was common, including high-risk scenarios such as smoking, alcohol use and sofas.
Abbreviations
-
- SIDS
-
- sudden infant death syndrome
Key notes
- Safe sleep recommendations have lowered sudden infant death rates in Norway, but data on adherence is lacking.
- An online survey in 2018 examined whether 4150 parents followed safe sleep recommendations and studied infants’ sleeping environments.
- A key finding was that 72.6% of the 2330 parents with infants under six months of age reported a history of high-risk behaviour, such as sleeping together on a sofa or bed-sharing after smoking or drinking.
1 INTRODUCTION
The dramatic decline in the incidence of sudden infant death syndrome (SIDS) in the early 1990 s has primarily been attributed to back-to-sleep campaigns, which advised parents to avoid placing infants in the prone position.1, 2 In Norway, 142 infants died of SIDS in 1989, compared to an average of 7 deaths per year in the 10-year period between 2010 and 2020.3 These numbers correspond to a drop in incidence from approximately 2.6 to 0.12 per 1000 live births. In addition to the prone position, a number of other factors in the child's sleeping environment have been shown to increase the risk of sudden death in infancy. Overly-soft mattresses, bumper pads and excessive bedding or clothing may lead to overheating. It may also lead to hypoxia, because the baby is rebreathing expired air, or entrapment, which mechanically restricts its airway passage.4 Putting the baby to sleep in a defective or broken bed may cause wedging or other mechanisms of accidental suffocation. Avoiding such risk factors is strongly recommended in safe sleep guidelines worldwide.4 The risk of bed-sharing, when an adult and infant share a bed and both fall asleep, has been a matter of debate for more than three decades. Several epidemiological studies have documented a clear association between bed-sharing and sudden death in infants younger than four months and infants with low birth weights.5, 6 But, the risk seems to have been mainly related to the parents’ use of tobacco smoking, alcohol and, or, drugs or if the co-sleeping occurred on an unsuitable surface, such as a sofa or armchair.7-9
Recommendations and campaigns for safe sleeping practices need to be based on scientific evidence, but they also need to be adapted to local cultures and target population. The Norwegian guidelines are formed on behalf of the Norwegian authorities by the advisory board of the Norwegian SIDS and stillbirth association. These guidelines emphasise that infants should always be put to sleep in a supine position. They also state that the safest place for an infant to sleep is in a separate bed, specially designed for infants, close to their parents’ bed.10 The guidelines recognise that mothers frequently fall asleep while breastfeeding and, as such, they do not completely discourage all forms of bed-sharing. However, they do offer advice on how this can be done in the safest possible way.
The aim of this cross-sectional survey was to determine infants’ sleeping practices in Norway, and to what extent they were exposed to potentially hazardous sleeping arrangements.
2 METHODS
An online survey was prepared by the authors, with input from the Norwegian National Advisory Unit on Breastfeeding. The survey was revised following a small pilot study and advice from 10 community nurses from Oslo and the surrounding area. The survey was marketed to the parents of infants via public health centres, websites and social media affiliated with the Norwegian SIDS and Stillbirth Society, the Interest Group of Public Health Nurses in the Norwegian Nurses Organization and the National Advisory Unit on Breastfeeding. We also use Norwegian online channels for the parents of infants, such as Babybloggerne, Mammabanden, Altformamma, Kjennliv, Lillemini and others. The survey was conducted from May to December 2018 and was answered anonymously on the SurveyMonkey website. This took an average of five min and 38 s. The completion rate was 91%. The website generated an electronic dataset that included an Internet protocol address for the computer, mobile phone or tablet used to fill out the survey form. This was just used to remove duplicates and was then deleted to ensure anonymity before the raw data were stored and processed.
The survey consisted of 36 questions, including demographics about the child and the parents and the parents’ country of origin and marital status (Supplementary file). The sleep environment was evaluated using questions concerning where and how the child was put to sleep, the contents of any crib that was used, what clothing the child slept in and different questions regarding bed-sharing. The child's nutrition was explored as well as the parents’ use of nicotine products, alcohol and narcotics. We recorded the answer as routine bed-sharing if the respondent said that they put the child to sleep in the parents’ bed between the mother and father or partner or next to the mother or father. The same method was used when recording answers concerning where the child slept the previous night.
Several of the questions did not have mutually exclusive answers. In these cases, the answers were merged and overlapping responses were removed. Inconsistent answers were compared with other similar questions for confirmation.
First, we performed descriptive analyses and then logistical regression analysis with routine bed-sharing as the outcome variable. We then used multivariate logistical regression analysis. The seven independent variables that were found to be significant in the univariate analysis and were then included in the model. We also included the child's gender and the ages of the mother and the father. Non-significant variables were removed in a stepwise manner, and only significant variables were included in the final analysis.
The conventional significance level of 5% was used. The analyses were conducted using SPSS, version 26 (IBM Corp, New York, USA).
3 RESULTS
The survey generated 4886 responses, and 4150 were included in the study. We removed 727 responses because the children were over 12 months of age and nine that had failed to report the child's age. The median age of the infants was five months. The infants were divided into groups according to their age in months and each group contained a minimum of 236 responses. Just over half of the responses related to boys (51%). The majority (99%) were filled in by the child's mother, 0.7% by the child's father, 0.3% by other family members who cared for the child such as a step-parent or grandmother. The age and marital status of the parents, their country of birth and the number of children in the household are shown in Table 1.
| Percentage | n | |
|---|---|---|
| Mother's age. n = 4147 | ||
| Under 20 | 0.4% | 17 |
| 20–25 | 15.8% | 656 |
| 26–30 | 41.1% | 1704 |
| 31–35 | 31.7% | 1314 |
| 36–40 | 9.6% | 398 |
| Above 40 | 1.4% | 58 |
| Father's age. n = 4145 | ||
| Under 20 | 0.1% | 5 |
| 20–25 | 7.3% | 304 |
| 26–30 | 31.8% | 1320 |
| 31–35 | 36.1% | 1499 |
| 36–39 | 14.4% | 597 |
| 40–45 | 8.1% | 336 |
| Above 45 | 2.0% | 84 |
| Mother's birthplace. n = 4146 | ||
| Norway | 94.7% | 3930 |
| Western Europe | 2.7% | 110 |
| Eastern Europe | 1.0% | 43 |
| Africa | 0.0% | 2 |
| Asia | 0.9% | 38 |
| North America | 0.2% | 9 |
| South America | 0.3% | 13 |
| Australia | 0.0% | 1 |
| Father's birthplace. n = 4145 | ||
| Norway | 89.9% | 3730 |
| Western Europe | 4.9% | 202 |
| Eastern Europe | 1.2% | 50 |
| Africa | 0.7% | 27 |
| Asia | 1.6% | 68 |
| North America | 0.5% | 20 |
| South America | 0.7% | 30 |
| Australia | 0.1% | 6 |
| Unknown | 0.3% | 12 |
| Marital status. n = 4150 | ||
| Single parent | 2.7% | 110 |
| Married | 35.3% | 1464 |
| Cohabitant/partnership | 62.0% | 2575 |
| Number of children in the family. n = 4146 | ||
| 1 | 51.8% | 2151 |
| 2 | 32.4% | 1345 |
| 3 | 11.0% | 457 |
| 4 or more | 4.7% | 193 |
Table 2 details how the respondents usually placed their children to sleep. This shows that 2.6% routinely placed their child to sleep in a prone position and 33.2% routinely used a side position. Several added notes to say that the prone and, or, side position were used when breastfeeding, and the child sometimes fell asleep on the mother's chest. However, they were then placed in the supine position. Of the 2330 patients with children under six months of age, 50 (2.1%) reported placing their children to sleep in the prone position and 693 (29.7%) on their side.
| Percentage | n | |
|---|---|---|
| Routinely bed-share with parentsa | 62.7% | 2604 |
| Next to mother | 55.0% | 1433 |
| Between mother and father | 21.3% | 555 |
| Both next to mother and between parents | 23.3% | 608 |
| Next to father | 0.3% | 8 |
| Routinely use of separate bed (incl. bedside crib)a | 74.2% | 3078 |
| In the parents’ bedroom | 80.2% | 2468 |
| In separate bedroom | 19.8% | 610 |
| Routinely position laid to sleep | 100% | 4150 |
| Supine | 65.6% | 2721 |
| Prone | 0.8% | 34 |
| Side | 9.1% | 379 |
| Supine/side | 22.7% | 944 |
| Supine/prone | 1.1% | 45 |
| Prone/side | 0.7% | 27 |
| Routinely use of baby nest | 50.4% | 2091 |
| In the cot | 54.1% | 1132 |
| In the parent's bed | 32.2% | 673 |
| Other (day bed, playpen, crib, etc.) | 13.7% | 286 |
| Routinely use of plastic mattress protectors | 24.1% | 1001 |
| Routinely use of breathing monitor | 1.3% | 56 |
| Routinely use of pillow | 5.1% | 213 |
| Routinely use of woollen blankets/sheepskin over the mattress | 11.7% | 460 |
| Routinely use of baby hat | 0% | 0 |
- a Multiple answers possible.
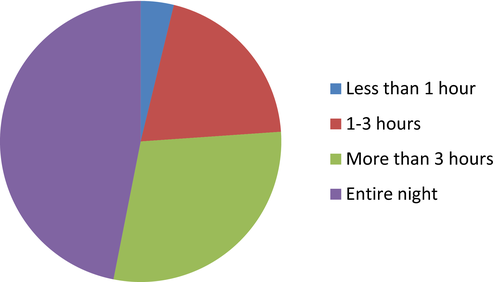
Routinely infant bed-sharing with one or both parents was reported by 2604/4150 (62.7%) (Table 2). There were 2651/4150 (63.9%) who reported having bed-shared with their infant the night before filling in the questionnaire, but 290 (10.9%) of these said that they did not do this on a routine basis. Routine night and previous night bed-sharing rates were both consistent across the age groups. The duration of bed-sharing the previous night is shown in Figure 1.
Of those who reported bed-sharing, 2514/2601 (96.7%) said the parental bed was a king size, which was at least 140 cm wide, with a mattress top covering the entire bed. Others reported that the bed-sharing took place in a smaller 120 cm double bed (2.3%), single bed (0.5%) or other types of beds or mattresses. However, when they were asked if they had ever fallen asleep with the child on a sofa or armchair, 2270/4143 (54.8%) replied yes. This proportion did not differ between those who reported routine bed-sharing (54.7%) and those who did not (55.0%).
Maternal use of nicotine products and drugs is shown in Table 3. Smoking was more prevalent among single parents (12/110, 10.9%) than among married or cohabiting parents (134/4033, 3.3%, p < 0.001). The same was true for the use of snus moist tobacco (23/109, 21.1%) compared to 9.9%, 401/4035, p < 0.001). Routine night and previous night bed-sharing were reported by 51.4% and 54.8% of mothers who smoked. The prevalence of bed-sharing among mothers who smoked, used moist tobacco or e-cigarettes was consistent throughout the first year of life. Of the fathers, 317/4150 (7.6%) smoked and 1310/4142 (31.6%) used moist tobacco. Routine infant bed-sharing with both parents was reported in 81/317 (25.5%) cases when the father smoked. Only 51/2324 (2.2%) of the mothers with children under six months of age reported drinking alcohol >1 time per week, but 148/2327 (6.4%) of these reported a history of bed-sharing after alcohol consumption (Figure 2).
| Percentage | n | |
|---|---|---|
| Mother smokes | ||
| Yes | 3.5% | 146 |
| Occasionally | 1.6% | 65 |
| <5 cigarettes/day | 0.4% | 17 |
| 5–10 cigarettes/day | 1.1% | 44 |
| >10 cigarettes/day | 0.4% | 20 |
| Mother uses moist tobacco placed in the mouth | ||
| Yes | 10.2% | 424 |
| Occasionally | 4.6% | 191 |
| < 5 doses/day | 0.7% | 29 |
| 5–10 doses/day | 2.5% | 103 |
| >10 doses/day | 2.4% | 101 |
| Mother uses e-cigarettes | ||
| Yes | 1.3% | 52 |
| Mother smokes, uses moist tobacco placed in the mouth and, or e-cigarettes (multiple answers possible) | 14.1% | 585 |
| Mother uses alcohol | ||
| Yes | 42.4% | 1755 |
| <1 time per month | 27.5% | 1142 |
| <1 time per week | 12.0% | 499 |
| >1 time per week | 2.7% | 114 |
| Mother uses hashish | ||
| Yes | 0.4% | 10 |
When they were asked when the child slept in the parental bed, 77.2% answered that bed-sharing was linked to breastfeeding, 63.8% said it was when the infant needed help to calm down and 36.5% said when it was convenient. Multivariate regression analysis found that several factors were associated with significantly increased odds ratios for bed-sharing. These were single parents, infant being older than six months and nocturnal breastfeeding (Table 4). The increased frequency of nocturnal breastfeeding was associated with a higher rate of bed-sharing. The odds for bed-sharing when breastfeeding three or more times per night were 11.9, with a 95% confidence interval of 9.7–14.7, compared with those who did not breastfeed at all.
| Variable | Percentage | Number | OR | p-value | Adjusted OR | p-value |
|---|---|---|---|---|---|---|
| Marital status | ||||||
| Marrieda | 62.6% | 916/1464 | ||||
| Partner | 62.4% | 1606/2575 | 0.99 (0.87–1.13) | 0.90 | 1.14 (0.99–1.33) | 0.08 N. S. |
| Single parent | 74.5% | 82/110 | 1.75 (1.13–2.73) | 0.01 | 2.68 (1.65–4.38) | <0.001 |
| The age of the child | ||||||
| 0–5 monthsa | 64.1% | 1495/2330 | ||||
| 6–11 months | 61.0% | 1110/1820 | 0.88 (0.77–0.99) | 0.04 | 1.33 (1.14–1.54) | <0.001 |
| Siblings/other children in the household | ||||||
| Noa | 58.6% | 1261/2151 | ||||
| Yes. 1 or more | 67.1% | 1339/1995 | 1.44(1.27–1.64) | <0.001 | 1.42 (1.23–1.64) | <0.001 |
| Nocturnal breastfeeding | ||||||
| Noa | 27.6% | 207/749 | ||||
| Yes. 1 time | 48.5% | 284/586 | 2.46 (1.96–3.09) | <0.001 | 2.64 (2.09–3.34) | <0.001 |
| Yes. 2 times | 63.1% | 577/914 | 4.48) (3.63–5.53) | <0.001 | 5.04 (4.04–6.28) | <0.001 |
| Yes. 3 or more times | 80.8% | 1533/1897 | 11.03 (9.06–13.43) | <0.001 | 11.90 (9.67–14.65) | <0.001 |
| Mother smokes | ||||||
| Noa | 63.2% | 2527/3998 | ||||
| Yes | 51.4% | 75/146 | 0.62 (0.44–0.86) | 0.004 | —b | |
| Mother uses moist tobacco placed in the mouth | ||||||
| Noa | 63.6% | 2368/3721 | ||||
| Yes | 55.0% | 233/424 | 0.70 (0.57–0.85) | <0.001 | —b | |
| Mother's alcohol use after birth | ||||||
| Nevera | 68.2% | 1629/2388 | ||||
| <1 time per month | 57.2% | 653/1142 | 0.62 (0.54–0.72) | <0.001 | 0.87 (0.73–1.02) | 0.09 N. S. |
| <1 time per week | 52.7% | 263/499 | 0.52 (0.43–0.63) | <0.001 | 0.59 (0.47–0.73) | <0.001 |
| >1 time per week | 49.1% | 56/114 | 0.45 (0.31–0.66) | <0.001 | 0.69 (0.45–1.04) | 0.08 N. S. |
- a reference variable.
- b Not significant and therefore not included in the final multivariate analysis.
A total of 1691/2330 (72.6%) respondents with children under six months of age indicated that the infant had been exposed to one or more risk situations for sudden infant death or suffocation (Figure 2).
4 DISCUSSION
This study indicates that in 2018, a very high proportion of parents in Norway practised bed-sharing in their child's first year of life. The occurrence of bed-sharing has increased steadily in Norway, from 4% in the mid-1980 s to around 30% in 2003–04. It is possible that it is now more than 60%.11-14 The prevalence indicated in this study is far higher than in other industrialised countries.9, 15 In spite of this, the incidence of sudden infant deaths has continued to decline. An in-depth study from Norway showed that there were approximately nine sleep-related infant deaths each year between 2010 and 2016, which was an annual incidence of 0.16 per 1000 live births.16 That incidence was approximately one-sixth of what has been reported from the United States.4 Such sleep-related deaths include SIDS, undetermined cases where accidental suffocation cannot be ruled out and rare cases of evident asphyxia due to entrapment or wedging. Although the incidence is low, all cases of accidental suffocation are preventable. It is very likely that some of the recent SIDS cases could also have been prevented by eliminating known risk factors. The Norwegian in-depth study reported that 46% of those who died from SIDS were found in a prone position and 46% of the parents reported smoking.16 Furthermore, eight infants who were less than 18 weeks of age were found dead when bed-sharing with a parent who smoked.16
Extensive international research has documented the increased risk of sudden infant death when bed-sharing is practised by parents who smoke, are under the influence of alcohol or drugs. Sleeping in a sofa or armchair is another factor.7, 8, 17-20 Whether bed-sharing in itself increases the risk of sudden infant death, without other contributory risk factors, is the subject of international debate.9, 21 Carpenter et al combined five databases that provided information on 1472 SIDS cases and 4679 controls from 19 countries in the UK, Europe and Australasia. They found that when non-smokers shared their bed with an infant who was two weeks of age the infant had an 8.3 times higher risk of sudden infant death than an infant who did not bed-share.7 This risk decreased to 3.6 at 10 weeks of age and 1.2 at 20 weeks. However, detailed data on the actual sleeping situations were lacking in this study. Parental use of alcohol or drugs, bed-sharing on sofas or in other hazardous sleeping environments may explain the observed increased risk, as indicated by other studies.9
Our study provides evidence that a high proportion of children in their first year of life is placed in what could be described as high-risk sleeping situations. Mothers who smoked, used moist tobacco or e-cigarettes, reported bed-sharing to a larger extent than those who did not, regardless of the potential risk for the infant. The fact that as many as 56.2% reported falling asleep with their child on a sofa or in an armchair and 6.4% reported sleeping with their child after consuming alcohol is worrying (Figure 2). It is encouraging that very few (2.1%) reported routinely placing infants below six months of age in a prone position when they put them down to sleep at night. A similar low rate of prone sleeping was reported by Wennergren et al in a Swedish survey published in 2020.22 Interestingly that survey also observed a high prevalence of side sleeping, like our study. The side position is unstable and has been associated with an increased risk for SIDS, although to a lesser extent than the prone position.23, 24
Research has showed that parental risk-related behaviour can effectively be altered with campaigns.25 The main goal of the guidelines formed by the Norwegian authorities for safe infant sleeping is to discourage prone sleeping. In 2007, the guidelines were changed from a categorical warning against any form for bed-sharing to specifically discouraging parents who smoke and avoid bed-sharing in hazardous settings, such as after consuming alcohol. The more subtle guidelines were because mothers increasingly reported that bed-sharing was related to breastfeeding, despite the warnings.11 Reaching common grounds with breastfeeding advocates, it was anticipated that the revised guidelines could improve understanding of the need to reach the population at risk. The present study raises the question of whether more targeted education of high-risk populations might be a better approach in the future.
Knowledge about trends in infant sleeping environments is essential so that we can distinguish between factors that pose risks and those that may contribute to prevention. Such knowledge is also important for the law enforcement officers who investigate these deaths. A major purpose of such investigations is to consider whether a death was the result of a criminal offence. Pressing charges for child endangerment when parents have been bed-sharing in a hazardous environment is an issue that is discussed from time to time. One important issue is whether parents are aware of the dangers. Updated knowledge can contribute to increased legal protection for both the children and the parents in the event of child deaths.
Our study also describes other trends in infant bedding. A high portion of the caregivers reported using a baby nest mattress (50.4%). Whether these products, which come in various forms, increase the safety of the child when bed-sharing, remain unknown. A variant of such a device, the Wahakura, has effectively been introduced to promote safe sleeping in a high-risk population in New Zealand.26 Baby nest is increasingly being used in other countries,22 and we are unaware of any deaths associated with them. However, more information is needed before advising their use. More concerning is the relatively high number of parents reporting use of plastic mattress protectors (24.1%) and sheep skins (11.7%) in the baby bed. Although there is limited evidence of risk, these devices might cause suffocation and overheating. Plastic mattresses may be impossible for a child to breathe through, causing suffocation. Misuse of sheep skins and warm clothing in a warm indoor climate may pose a threat of overheating the child.
A limitation of this study was that the socioeconomic background of the respondents was not fully explored. Low socioeconomic status has been shown to increase the risk of SIDS, possibly by affecting the ability to understand health advice and put it into practice.27 The study's strength was the relatively high number of respondents, as more than 4000 parents took part. However, this was less than 7.5% of number of births in Norway in 2018.28 The questionnaire was only in Norwegian, which limited participation to parents who had mastered the native language. Both the language restriction and the recruitment process may have led to a biased sample. Nevertheless, based on comparison of data from National registers, our respondents seem quite representative of the parents of infants in Norway. A number of factors corresponded to findings in the general population. These were the age of the first-time mothers, the gender distribution of the infants, the marital status of the parents, the country of birth, reported cigarette smoking and the use of moist tobacco.28-30
5 CONCLUSION
This 2018 study showed that a large percentage of Norwegian parents did not fully follow the guidelines on how to provide a safe sleeping environment for infants. These findings are worrying and underline the need to protect infants. Our findings suggest that the current recommendations, together with parental education, need to be revised to reach the high-risk population.
ACKNOWLEDGEMENTS
We thank the community nurses in Oslo, and the surrounding areas, who encouraged parents to take part in this survey.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare.