Impact of cleanroom status on the reasons for discarding organ-cultured corneal transplants in a modern eye bank – More donor corneas thanks to astronaut suit?
Abstract
Purpose
This study investigated the influence of cleanroom conditions on the discard rates of donor corneas in a German university eye bank.
Methods
Discard rates were analysed from 2017 to 2020 at the LIONS Cornea Bank at Saarland University Medical Center. 1941 corneas from 971 donors were included. 1262 corneas (65.1%) were stored in a class D cleanroom from 2017 to 2019 and processed in a cleanroom class A sterile bank (group 1). 679 corneas (34.9%) were continuously stored in a class B cleanroom and processed in a class A cleanroom safety cabinet in the same room from 2019 to 2020 (group 2). The target parameter of this work was the number of contamination-related discards. Although they cannot be influenced by the spatial conditions, the discards due to insufficient endothelial quality, serology, contraindications, scars and technical causes were also recorded. Statistical analysis was performed using SPSS and various testing procedures.
Results
In group 1, significantly more corneas were discarded due to positive serology (6.9%|3.8%, p = 0.020). There was no significant change between both groups for either contamination or the other reasons for discard.
Conclusion
Optimization of hygiene standards from cleanroom class D to B did not reduce contamination. Serology, endothelial quality, medical contraindications and the presence of scars cannot be influenced by cleanroom conditions.
1 INTRODUCTION
Since Eduard Zirm performed the first successful keratoplasty in 1905, the procedure has become the most common tissue transplantation in the world (Maghsoudlou et al., 2022; Zirm, 1906). In Germany, there are currently 26 cornea banks – 7 of which are supported by the LIONS – in which 11 788 corneas were cultured and 8438 were released for transplantation in 2021 (Reinshagen et al., 2023).
Despite this amount of corneal transplants performed annually, the German Society for Tissue Transplantation (DGFG) estimates that 12.0% of patients on a waiting list for keratoplasty cannot be supplied due to lack of donor tissue (German Society for Tissue Transplantation, 2020). Flockerzi et al. reported an average waiting time of 9 weeks for a PKP in Germany in 2021 according to the recent German Keratoplasty Registry Report of the cornea section of the German Ophthalmological Society (DOG) (Flockerzi et al., 2023). This is due on the one hand to the overall low willingness to donate and on the other hand to the increasing demand also in view of the increasing age of the overall population (Seitz et al., 2004). The shortage is exacerbated by the fact that not every cornea harvested meets the requirements for donor tissue. In 2021, the discard rate of all corneas harvested in Germany was 32.0%, which was almost unchanged compared to 2014 (30.0%) (Reinshagen et al., 2016, 2023). Therefore, in addition to increasing the willingness to donate, measures to reduce the discard rate are also important influencing factors. Since bacterial contamination of the culture system is one of the quantitatively relevant reasons for discard, it can be assumed that the proportion of suitable corneal transplants can be increased with an optimization of the hygienic standards in the premises of an eye bank.
The guideline for the collection of donor corneas and for the management of a cornea bank contains specifications for facilities and premises and is fixed by the German Medical Association in the framework conditions for cornea donation in Germany. In addition to the strict separation of cornea bank and daily clinical practice “guaranteed,” the quality of cleanrooms is also stipulated. The classifications of cleanrooms according to the European Union Good Manufacturing Practices (EU GMP) guidelines are based on microbiological parameters, defined air exchange rates and the number of particles in the air. The corresponding specifications are listed in Tables 1 and 2.
| Cleanroom class | Air sample CFU/m3 | Sedimentation plates (Ø 90 mm) CFU/4 h | Contact plates (Ø 55 mm) CFU/plate | Glove print 5 fingers CFU/glove | Minimum air exchange rate (1/h) |
|---|---|---|---|---|---|
| D | 200 | 100 | 50 | - | 15 |
| C | 100 | 50 | 25 | - | 30 |
| B | 10 | 5 | 5 | 5 | 60 |
| A | <1 | <1 | <1 | <1 | 80 |
- Abbreviations: CFU, colony-forming unit.
| Cleanroom class | Idle status | Operating status | ||
|---|---|---|---|---|
| 0.5 μm | 0.5 μm | 0.5 μm | 0.5 μm | |
| D | 3.520.000 | 29.000 | Not specified | Not specified |
| C | 352.000 | 2.900 | 3.520.000 | 29.000 |
| B | 3.520 | 29 | 3.520 | 20 |
| A | 3.520 | 20 | 3.520 | 20 |
The specifications of the German Medical Association say “For all processing steps… in which the donor cornea is exposed to the environment, … a Class A air cleanliness level of the definition of the EU GMP Guide, with a … suitable background environment that … corresponds at least to Class D, is required.” By this regulation, only a suitable safety cabinet is obligatory as a Class A cleanroom, and the suitability of the same must be guaranteed by regular qualification (German Medical Association, 2018).
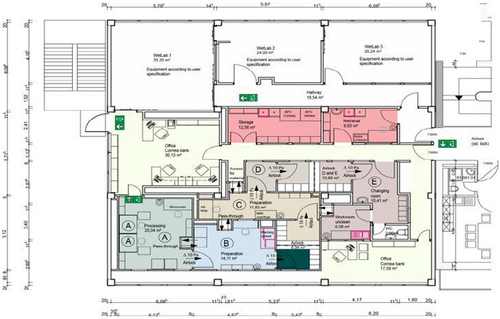
The rooms of the original cornea bank in Homburg/Saar, which was inaugurated in 2000, met these requirements. On a total of about 25 square meters, there was a room for administrative tasks and a class D cleanroom of about 12 square meters in which the corneal grafts were stored and processed in the HeraSafe HS 12 safety cabinet (Heraeus GmbH, Hanau, Germany) (Figure 1). This corresponded to cleanroom class A. In comparison, the rooms of the recently established Klaus Faber Center for Corneal Diseases, incl. LIONS Cornea Bank Saar-Lor-Lux, Trier/Westpfalz, which opened in February 2019, far exceed the minimum legal requirements. On approximately 200 square meters, a pure facility plant was developed after a concept of the company ap-Systems (Reutlingen, Germany) with areas of the classes E without fixed minimum requirements (therefore not listed in tables 1 and 2) to B, which are arranged – as a component of the contamination control – in a shell concept. This means that clean areas are surrounded by areas of the next lower cleanliness class. The layout of the plan is shown in Figure 2. A WetLab for learning technically demanding procedures is also located in the eye bank rooms (Seitz et al., 2018).
With regard to the technical specifications, the technical conditions of cleanroom class A are met in the production room (Figure 3). For example, the ventilation system with 170 air exchanges per hour permanently guarantees cleanroom class A conditions. In addition to the shell concept and to ensure air quality, a clothing concept contributes to contamination control. After removing street clothing and shoes and using several airlocks, this involves donning cleanroom undergarments, hairnets, cleanroom shoes, cleanroom overalls, sterile gloves and a sterile face mask. This also complies with the requirements of cleanroom class A according to EU GMP guidelines. However, in view of very high operating costs – including for cleaning and electrical supply – the manufacturing room was not operated permanently as a Class A cleanroom, which is why it is classified here as a Class B cleanroom.


The aim of this work was to evaluate the impact of cleanroom status on the corneal graft discard rate in the cornea bank of a German university eye department.
2 MATERIALS AND METHODS
A total of 1941 corneas collected (971 donors) between 01/01/2017 and 03/02/2020 were divided into two groups according to the cleanroom conditions of culture and processing. A group of 1262 corneas (65.1%) from 631 donors was cultured and processed between 01/01/2017 and 02/03/2019 under the original cornea bank premises (opened 07/14/2000) in a laminar flow cabinet (Grade A) in class D background (group 1). This group is opposed to a group of 679 corneas (34.9%) from 340 donors that were cultured and processed in a laminar flow cabinet (Grade A) in a class B background between 04/02/2019 and 03/02/2020 under the new premises of the Klaus Faber Center for Corneal Diseases, incl. LIONS Cornea Bank Saar-Lor-Lux, Trier/Westpfalz. In all cases, corneal preparation was performed in a cleanroom class A safety cabinet. There were no differences between the two corneal banks regarding the collection method, the endothelial assessment methodology and the composition of the culture medium. The corneas were procured by in situ excision of corneoscleral discs. The sampling location was not standardized. The corneal collection took place in the clinical department where the donor passed away. Blood collection for serological testing took place at the time of corneal procurement. The serological examination was performed by PCR. Cooling of the donors did not take place on a regular basis, as corneal sampling was usually performed promptly while the donors were still at the place of death.
The primary outcome measure was the number of discards due to infection, detected by positive conjunctival swabs or contamination of the culture medium. Although not influenced by spatial conditions, discards due to inadequate endothelial quality, contraindications, serology, technical causes, and scars were also recorded.
A relevant detection of germs in the conjunctival swab was also considered a reason for discard as well as contamination of the culture medium until the amendment of the guideline for the operation of a cornea bank in spring 2018. However, in the LIONS Eye Bank Saar-Lor-Lux, Trier/Westpfalz, standard conjunctival swabs were performed until January 13, 2020 as an additional safety measure beyond the legal requirements. Accordingly, only in a few cases of the second group (n = 48) no additional conjunctival swab was performed. Endothelial cell density of 2000 cells/mm2 for penetrating keratoplasty (PKP) and 2200 cells/mm2 for Descemet Membrane Endothelial Keratoplasty (DMEK) was defined as the cut-off value for endothelial quality. Corneas with an endothelial cell density < 2000 cells/mm2 were not released for primary PKP. However, grafts with an endothelial cell density between 1700 and 2000 cells/mm2 were released for emergency PKP, corneas with <1700 cells/mm2 for Deep Anterior Lamellar Keratoplasty (DALK). Those with endothelial cell loss of more than 25.0% during cultivation or extensive necrotic areas exceeding 10% of the endothelium or more were also excluded for elective keratoplasty. The criteria were not changed during the observation period; however, a new microscope was implemented in the new rooms of the Klaus Faber Center (Old: Leica DM IL, Leica Camera AG, Wetzlar, Germany. New: Primovert, Carl Zeiss AG, Oberkochen, Germany).
A positive result on serologic workup for human immunodeficiency virus (HIV), hepatitis B or C, or evidence of Treponema pallidum infection would result in graft discard. Technical causes for discard are impossible blood collection from the donor or rupture of the graft during preparation for DMEK. In addition, according to the Transplantation Act, diseases of the central nervous system such as Alzheimer's disease, amyotrophic lateral sclerosis or multiple sclerosis, a risk of prion diseases transmission or active systemic infections were considered medical contraindications, which also excluded the use in the context of an emergency transplantation. Scars conspicuous during slit-lamp examination also led to exclusion if DMEK was not possible due to the endothelial condition. The collected data on corneal donors and corneas were taken from internal hospital documents such as death certificates, collection protocols, microbiological findings, or examination protocols and stored in a Microsoft Access 2019 database. To perform the statistical analysis the IBM (IBM, Armonk, NY, USA) SPSS Version 29 was used. T-test, Mann–Whitney U test, chi-squared test, Pearson's correlation as well as multiple logistic regression were used where appropriate. A p-value <0.05 was considered to show a statistically significant result.
3 RESULTS
3.1 Demographic characteristics of corneal donors
The mean age of all corneal donors recorded was 73 ± 14 years with a range of 4 to 103 years and a median of 76 years. In group 1 (cleanroom class D), the age ranged from 4 to 103 years with a mean of 72 ± 15 and a median of 75 years, and in group 2 (cleanroom class B), the age range was from 17 to 98 years with a mean of 74 ± 14 and a median of 76 years (p = 0.098). With regard to the donor age, there was a minimum age of 4 years, without an upper limit. Overall, 59.1% (n = 1150) of all donors were male. In the original cornea bank (cleanroom class D), 786 corneas of male donors (62.0%), and in the Klaus Faber Center for Corneal Diseases, incl. LIONS Cornea Bank Saar-Lor-Lux, Trier/Westpfalz (cleanroom class B), 364 corneas of male donors (53.6%) were recorded.
3.2 Discard rate
During the observed period, the overall discard rate was 45.8% (n = 890). After a discard rate of 627 (49.7%) corneas in group 1 (cleanroom class D), the rate decreased to 287 (42.3%) in group 2 (cleanroom class B). This 7.4% reduction in the discard rate showed statistical significance (p = 0.0018).
3.3 Reasons for donor discard
Table 3 summarizes the frequency of discard reasons.
| Reason for discard | Group 1 (D) | Group 2 (B) | Total | p-value |
|---|---|---|---|---|
| Serology | n = 87 (6.9%) | n = 26 (3.8%) | 113 (5.8%) | p = 0.020 |
| Endothelial quality | n = 332 (26.3%) | n = 144 (21.2%) | 476 (24.5%) | p = 0.430 |
| Technical causes | n = 20 (1.6%) | n = 21 (3.1%) | 41 (2.1%) | p = 0.064 |
| Conjunctival swab | n = 106 (8.4%) | n = 51 (7.5%) | 157 (8.1%) | p = 0.489 |
| Contamination | n = 51 (4%) | n = 27 (4%) | 78 (4%) | p = 0.651 |
| Contraindications | n = 23 (1.8%) | n = 15 (2.2%) | 38 (2%) | p = 0.180 |
| Scars | n = 33 (2.6%) | n = 11 (1.6%) | 44 (2.3%) | p = 0.124 |
| ECD >2.000 cells/mm2 | n = 910 (72.1%) | n = 540 (79.5%) | 1450 (74.7%) |
- Note: The difference between the number of discards (n = 890) mentioned throughout the manuscript and the sum of discard reasons (n = 910) results from the fact that some corneas were discarded because of more than one discard reason.
With 476 (24.5%) corneas discarded, insufficient endothelial quality was the most common reason for discarding corneal donor buttons for primary keratoplasty. From 332 (26.3%) discarded corneas in group 1 (cleanroom class D), the endothelium-related discard rate decreased to 133 (19.6%) in group 2 (cleanroom class B) (p = 0.011). Of the total 476 corneas, which were not released for primary PKP due to endothelial quality, 194 could be used for emergency indications.
The second most frequent reason for discard was a germ detection in the conjunctival swab of the respective corneal donor. This affected a total of 157 corneas (8.1%). Distribution of 106 discards (8.4%, group 1) and 51 discards (7.5%, group 2) does not represent a significant reduction (p = 0.489). Candida albicans was detected most frequently (90.4%). Another indicator of infection was contamination of the culture medium. This led to discard in a total of 4% of cases (n = 78). There was no statistical significance with regard to the reduction for a proportion of 4% (n = 51, group 1) versus 4% (n = 27, group 2, p = 0.651).
The third most frequent reason for discard was positive serology, which was present in a total of 113 donors (5.8%). Before change of premises, this affected 87 donors (6.9%), afterwards 26 donors (3.8%, p = 0.020).
Less common reasons for discard were stromal scars, medical contraindications or technical reasons. Because of present scars, a total of 2.3% (n = 44) had to be discarded, including 2.6% (n = 33) in group 1 and 11 (1.6%, p = 0.201) in group 2. A medical contraindication required discard in 2% (n = 38) of all cases (1.8%, (n = 23, group 1) and 2.2%, (n = 15, group 2, p = 0.180). Technical causes of discard included, for example, impossible blood collection from the donor – making serologic testing impossible – or rupture during preparation of the Descemet membrane endothelial lamella for DMEK. These were present in 2.1% (n = 41) of all cases 1.6%, (n = 20, group 1) and 3.1% (n = 21, group 2, p = 0.064).
4 DISCUSSION
According to a survey by Flockerzi et al. (2018), the number of corneal transplants performed in Germany increased 1.5-fold from 2001 (n = 4730) to 2016 (n = 7325) (Flockerzi et al., 2018). Despite similar figures from a 2020 publication of the German Keratoplasty Registry in Germany (2011: 4533 procedures, 2020: 8912 procedures), 4615 patients were still waiting for corneal transplantation in Germany on December 31, 2020 (Seitz, 2021). The average waiting time for PKP is about 8–12 weeks (Flockerzi et al., 2018). In view of the increasing life expectancy, the demand for corneal transplantation is expected to increase further. Therefore, different approaches are used to increase the number of donors and to reduce the discard rate of donor corneas. The subject of the present study was the approach to reduce the number of contamination-related discards by optimizing the hygienic conditions in a high-class cleanroom cornea bank.
According to the German Ophthalmological Society's 2021 performance report, the discard rate this year was 32%. 14% of the discards were due to contamination. With 48%, insufficient endothelial quality was the main reason for discard. Of 1460 endothelially compromised donor corneas, 519 could be transplanted for emergency indications. The discard rate remained almost constant compared with 2014 (Reinshagen et al., 2016). Endothelial quality was also the most common reason for discard in our study. Of 476 corneas not released for PKP, 194 could be used for emergency indications.
In our study, a total of 12.1% of corneas were discarded because of microbiological contamination (8.1% conjunctival swab, 4% contamination of culture medium), which is close to the 14% in the German average (Reinshagen et al., 2023). International studies show inhomogeneous results regarding contamination rates. The New Zealand Eye Bank Study reported 1% microbiological contamination between 2000 and 2009 (Cunningham et al., 2012). Data from a French eye bank between 2005 and 2018 reported an average annual contamination rate of 6.8% (Fabre et al., 2021). In a study by the Eye Bank of Rome, contamination was detected in 67% of donated corneas (Vignola et al., 2018). It is indispensable to utilize transplants with limited suitability for emergency indications. Despite an increasing number of some emergency indications such as acanthamoebic keratitis or fungal keratitis, the number of emergency transplants has remained constant during the observation period of our work (Daas et al., 2015; Nielsen, 2020; Roth et al., 2019). Looking at the annual rate of emergency transplants, there was no significant change in 2017, 2018, and 2019 (2017 10%, 2018 9.8%, 2019 9.8%, p = 0.722).
Internationally, 124 843 donor corneas were processed by American cornea banks with intent to surgical use in 2019. The discard rate of 32.4% corresponds approximately to the German average of 32.0%. Main reasons for discard were insufficient tissue suitability, positive serology as well as medical contraindications (according to American guidelines), which in contrast to our study included all septic processes as causes of death (Eye Bank Association of America, 2020). Given the low number of serologically induced discards in our study, there is no clinical relevance despite statistical significance. Since donor serology cannot be influenced by the spatial conditions, this result cannot be explained by the cleanroom conditions. A possible cause could be the reporting of donors from different hospitals with different treatment priorities. However, such a cause could not be identified in the present study.
Arya et al. published a study from an Indian cornea bank in April 2021. Here, a total of 1646 corneas were recorded between November 1999 and October 2015. The overall discard rate was reported to be 43.3%, although in contrast to our study, donor corneas were discarded only at an endothelial cell density < 1500 cells/mm2. Medical contraindications and inadequate graft quality were reported as the main causes of discard. Furthermore, the percentage of usability of corneas decreased with increasing donor age (Arya et al., 2021).
With the onset of the worldwide COVID-19 pandemic, corneal banks experienced difficulties in finding suitable donors. However, the absence of active viral structural proteins in Severe Acute Respiratory Syndrome COVID-19-positive donor corneas (Casagrande et al., 2021) and the negligible risk of transmission after proper donor selection promptly allowed a return to normal donations (Hamon et al., 2021).
Kramp et al. (2020) could prove by an analysis of data of the LIONS Cornea Bank Saar-Lor-Lux, Trier/Westpfalz from 2006 to 2016 that a donor age > 80 years as well as a previous cataract surgery significantly increase the risk of donor discard. Similarly, sepsis and multiple organ failure significantly increase the risk of contamination of the culture medium (Kramp et al., 2020). Similar results were reported by Yu et al. (2014) from the eye bank of the Ludwig-Maximilians-University Munich. Here, 377 patients were followed up after PKP during the period 2001–2011. Significant factors associated with graft failure included high donor age and low donor endothelial cell density (Yu et al., 2014).
The present work is one of the first to address the effects of the cleanroom infrastructure on the discard rate. Since working in a cleanroom significantly improves the hygienic conditions, the focus of attention was primarily on the infection-related discards that can be detected by conjunctival swabbing or contamination of the culture medium. With regard to this, the evaluation of the collected data did not show a significant reduction of the discard rates. Therefore, it must be assumed that the cleanroom conditions around the safety cabinet during the cultivation and processing of the corneas do not have a relevant impact on the discard rate. Since the Klaus Faber Center for Corneal Diseases, incl. LIONS Cornea Bank Saar-Lor-Lux, Trier/Westpfalz was designed very early future-oriented at the current point in time (05/2022) – with requirements that exceed the legal requirements by far – no comparable data are currently available in the literature.
The data presented suggest that infection of the donor cornea is acquired only to a small extent during collection and processing, but is already determined at the time of procurement. To support this assumption, a risk assessment was performed using the Microbiological Risk of Contamination Assessment (MiRCA) tool of the European Directory for the quality of medicines & HealthCare (EDQM). Considering the existing conditions during collection, transport and processing, the probability of acquired infection was considered “unlikely” with a score of 63.9 from 695.
5 CONCLUSIONS
Optimization of hygienic conditions by establishing a cleanroom cornea bank has no significant impact on the contamination-related corneal donor tissue discard. Serology, medical contraindications and the presence of scars cannot be influenced by cleanroom conditions.
Acknowledgements
Open Access funding enabled and organized by Projekt DEAL.