Ectopic inner foveal layer as a factor associated with metamorphopsia after vitrectomy for epiretinal membrane
Abstract
Purpose
To analyse the relationship between the extent of metamorphopsia and optical coherence tomography (OCT) parameters including the ectopic inner foveal layer (EIFL) in patients with epiretinal membrane (ERM) who underwent pars plana vitrectomy (PPV).
Methods
This study included 63 eyes of 62 patients who underwent PPV for ERM. Metamorphopsia was assessed by measuring the metamorphopsia score for vertical lines (MV) and metamorphopsia score for horizontal lines (MH) using M-CHARTS. Central retinal thickness (CRT), EIFL thickness and disruption of outer retinal layers were measured before and after surgery, and the relationship of these parameters with metamorphopsia scores at 3 months after vitrectomy was analysed.
Results
Preoperative MV correlated with preoperative CRT and EIFL (p = 0.005 and 0.045 respectively). Postoperative MH correlated with preoperative CRT (p = 0.048), while postoperative MV correlated with preoperative CRT and EIFL (p = 0.002 and 0.0006 respectively). Postoperative MH correlated with postoperative CRT and EIFL (p = 0.001 and 0.002 respectively), and postoperative MV also correlated with postoperative CRT and EIFL (p = 0.0008 and < 0.0001 respectively). MH and MV did not correlate with outer retinal layer disruptions, both before and after vitrectomy. When multiple regression analysis was performed on preoperative and postoperative OCT parameters that correlated with postoperative metamorphopsia scores, only postoperative EIFL was identified as an independent factor associated with postoperative MV (p = 0.042).
Conclusion
When PPV was conducted for ERM, postoperative EIFL was found to be a significant factor associated with postoperative metamorphopsia score.
Introduction
Epiretinal membrane (ERM) is a membranous tissue formed on the surface of the retina in the macular area by fibrocellular proliferation and is reported to be present in approximately 7 to 11.8% of people aged 40 years and above (Klein et al. 1994; Mitchell et al. 1997). In Japan, the Funagata study has also revealed that ERM is present in 5.44% of adults aged 35 years and above and that the prevalence increases with age (Kawasaki et al. 2009). Hence, ERM can be considered to be the most common macular disease. Traction of ERM causes morphological changes of the retina, leading to various visual disturbances including central vison loss, metamorphopsia and aniseikonia. Among these disturbances, metamorphopsia has been reported to have a direct impact on vision-related quality of life (VR-QOL) (Okamoto et al. 2009).
Pars plana vitrectomy (PPV) with membrane removal is an established standard treatment for ERM. However, even after an anatomically successful surgery, impaired visual functions including metamorphopsia often remain. Therefore, many studies have attempted to elucidate the prognostic factors of postoperative visual function. In recent years, remarkable advances in diagnostic imaging devices have allowed non-invasive examination of the changes in retinal morphology and retinal vascular structure in ERM patients using optical coherence tomography (OCT) and optical coherence tomography angiography (OCTA). Various imaging markers such as the thickness of the inner nuclear layer (INL), depth of the retinal fold, area of adhesion between the ERM and internal limiting membrane (ILM), and size of the foveal avascular zone (FAZ) have been shown to be associated significantly with the extent of metamorphopsia (Watanabe et al. 2009; Ooto et al. 2011; Kinoshita et al. 2012; Okamoto et al. 2012; Bae et al. 2013; Kim et al. 2013; Okamoto et al. 2015; Takabatake et al. 2018; Bae et al. 2020; Hirano et al. 2020; Shiihara et al. 2020).
Recently, Govetto et al. (2017) reported that the OCT finding of the presence of a continuous ectopic inner foveal layer (EIFL) in eyes with ERM was associated with significant vision loss and proposed a new staging scheme of ERM using EIFL. Since their report, several studies have examined the relationship between visual acuity and EIFL before and after vitrectomy for ERM (Doguizi et al. 2018; Sato et al. 2018; Govetto et al. 2019; Baek et al. 2020; González-Saldivar et al. 2020; Coppola et al. 2021; Mavi Yildiz et al. 2021). As for the association between metamorphopsia and EIFL, only Alkabes et al. (2020) reported a significant correlation, but there is no report on the relationship between metamorphopsia and EIFL before and after vitrectomy. Therefore, we analysed the relationship between the extent of metamorphopsia and OCT findings including EIFL in patients who underwent PPV with ERM removal and ILM peeling.
Methods
Patients
We conducted a retrospective observational study on ERM patients who underwent pars plana vitrectomy (PPV) at Tokyo Medical University Hospital between July 2017 and March 2020. This research protocol was approved by the Ethics Committee of Tokyo Medical University (approval number SH3782), and the research was conducted in compliance with the tenets of the Declaration of Helsinki.
Inclusion criterion was patients with unilateral or bilateral idiopathic ERM who underwent PPV. Exclusion criteria were patients with macular pseudo-hole, lamellar macular hole, secondary ERM and other eye diseases except cataract. Patients with severe cataract that affected the quality of OCT images were also excluded.
Examinations
All patients underwent ophthalmic examination before vitrectomy and 3 months after vitrectomy. Best-corrected visual acuity (BCVA) was measured using the Landolt C acuity chart conducted in a masked fashion, and visual acuity was converted to logarithm of minimal angle of resolution (logMAR) scale.
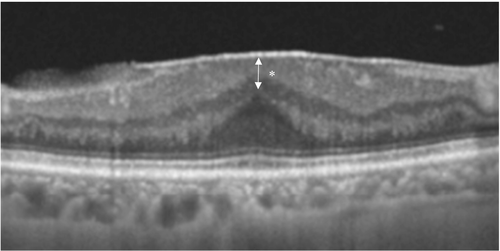
OCT imaging was conducted using spectral-domain OCT (Cirrus HD-OCT; Carl Zeiss, Dublin, CA, or RS-3000; Nidek, Aichi, Japan) and swept-source OCT (DRI OCT Triton; Topcon, Tokyo, Japan). We verified the location and position of the fovea by the fixation point, and the presence of the foveal bulge or foveal depression. When the foveal bulge or foveal depression was not depicted clearly due to strong ERM traction, we determined the foveal centre as the site where the outer nuclear layer showed the greatest inward protrusion. Both vertical and horizontal scans of 6 mm or 12 mm passing through the fovea were used. The central retinal thickness (CRT), presence or absence of disruption of external limiting membrane (ELM) and ellipsoid zone (EZ), and thickness of the EIFL were measured. CRT was measured manually using the calliper function, as the distance between the ILM and the inner limit of the retinal pigment epithelium (RPE) at the centre of the fovea. Disruption of ELM and EZ was assessed to be present when discontinuation of the bands of ELM and EZ, respectively, in the foveal region was detected. According to Govetto et al. (2017), EIFL was defined on OCT image as the presence of a continuous hypo- or hyper-reflective band extending from the INL and inner plexiform layer (IPL) across the foveal region. Similar to CRT, the calliper function was used to manually measure the distance between the inner limit of the ILM and the outer limit of the INL at the centre of the fovea (Fig. 1). All the measurements were conducted under complete masking of clinical data. To address the accuracy and reproducibility issues of manual measurements, CRT and EIFL measurements were conducted by two retina specialists (KY and YW) separately, and the averaged values were used in analyses.
Quantification of the extent of metamorphopsia is possible using M-CHARTS (Inami & Co. Ltd., Tokyo, Japan), which was developed by Matsumoto et al. (2003) and the usefulness of this tool has been reported (Matsumoto et al. 2003; Arimura et al. 2005). M-CHARTS consists of one solid straight line and 19 dotted straight lines with dot intervals ranging from 0.2° to 2.0° visual angles. When the patient is subjectively aware of metamorphopsia, the solid straight line projected onto the retina is perceived as a curved line. When the solid line is replaced by each of the dotted lines and the patient examined in the same manner, distortion of the line decreases as the distance between the dots increases, and eventually the line is perceived as a straight line. The visual angle at which the patient recognizes the dotted line as a straight line is defined as the metamorphopsia score. When the solid line is recognized as a straight line, the metamorphopsia score is 0 degree. During testing, first the metamorphopsia score for vertical lines (MV) is measured. Then, the test sheet is rotated 90 degrees and the metamorphopsia score for horizontal lines (MH) is measured. The measurements were performed by an experienced orthoptist who was completely masked to the clinical data.
Surgical technique
All patients underwent 25 G PPV conducted by three vitreoretinal surgeons using the Constellation Vision System (Alcon, Fort Worth, TX). Simultaneous phacoemulsification and aspiration together with intraocular lens implantation was performed when necessary. In all patients, triamcinolone acetonide (MaQaid, Wakamoto Pharmaceutical, Tokyo, Japan) was used to visualize the vitreous, and posterior vitreous detachment (PVD) was induced if PVD was absent. Then, the vitreous was removed. Next, the ERM was removed, and ILM was also completely removed using Brilliant Blue G. None of the patients underwent fluid-air exchange in this series.
Statistical analysis
Statistical analysis was performed using JMP® 14 (SAS Institute Inc., Cary, NC, USA). Continuous variables are expressed as mean ± standard deviation and categorical variables as number and percentage. Differences in logMAR BCVA, MH and MV scores, and all the OCT parameter before and after surgery were analysed by Wilcoxon signed rank test or Fisher's exact test. The correlation of each OCT parameter with logMAR BCVA, MH score or MV score was analysed by Spearman's rank correlation test. Multiple regression analysis was then performed using OCT parameters having significant correlation with MH and MV scores as independent variables. A p value less than 0.05 was considered statistically significant.
Results
Sixty-three eyes of 62 patients aged 68.6 ± 7.5 years (mean ± standard deviation) were studied. Table 1 shows the changes in logMAR BCVA, metamorphopsia score and OCT parameters from the first visit (baseline) to 3 months after vitrectomy. LogMAR BCVA improved significantly from 0.29 ± 016 before surgery to 0.002 ± 0.10 after surgery (p < 0.0001). Regarding the changes in metamorphopsia score, MH decreased significantly from 0.84 ± 0.57 before surgery to 0.51 ± 0.51 after surgery (p < 0.0001), and MV also decreased significantly from 0.77 ± 0.46 before surgery to 0.57 ± 0.58 after surgery (p = 0.0005). For OCT parameters, CRT (μm) decreased significantly from 452 ± 78 before surgery to 362 ± 63 after surgery (p < 0.0001), and EIFL (μm) from 117 ± 99 before surgery to 68 ± 65 after surgery (p < 0.0001). ELM disruption was observed in 20 eyes (31.7%) before surgery and in 9 eyes (14.3%) after surgery, showing a significant decrease in percentage (p = 0.023). EZ disruption was found in 7 eyes (11.1%) before surgery and in 4 eyes (6.3%) after surgery, with no significant difference.
| Baseline (n = 63) | 3 Months after surgery (n = 63) | p value | |
|---|---|---|---|
| LogMAR BCVA | 0.29 ± 0.16 | 0.002 ± 0.10 | < 0.0001* |
| MH | 0.84 ± 0.57 | 0.51 ± 0.51 | < 0.0001* |
| MV | 0.77 ± 0.46 | 0.57 ± 0.58 | 0.0005* |
| CRT, μm | 452 ± 78 | 362 ± 63 | < 0.0001* |
| EIFL, μm | 117 ± 99 | 68 ± 65 | < 0.0001* |
| ELM disruption, n (%) | 20 (31.7%) | 9 (14.3%) | 0.023† |
| EZ disruption, n (%) | 7 (11.1%) | 4 (6.3%) | 1.00† |
- BCVA = best-corrected visual acuity, CRT = central retinal thickness, EIFL = ectopic inner foveal layer, ELM = external limiting membrane, EZ = ellipsoid zone, MH = metamorphopsia score for horizontal line, MV = metamorphopsia score for vertical line.
- Values are presented as mean ± standard deviation or number (percentage).
- * p value: Wilcoxon singed-rank test.
- † p value: Fisher's exact test.
Table 2 shows the relationship between preoperative visual functions (logMAR BCVA, MH and MV) and preoperative OCT parameters. Preoperative logMAR BCVA did not correlate with any of the preoperative OCT parameters including EIFL. Regarding metamorphopsia scores, preoperative MV correlated with preoperative CRT and EIFL (p = 0.005 and 0.045 respectively), while preoperative MH did not correlate with any of the OCT parameters.
| Preoperative visual Function | Preoperative OCT parameters | |||
|---|---|---|---|---|
| CRT (μm) | EIFL (μm) | ELM disruption | EZ disruption | |
| LogMAR BCVA | ||||
| ρ | 0.136 | 0.215 | −0.044 | 0.082 |
| p value | 0.288 | 0.091 | 0.733 | 0.524 |
| MH | ||||
| ρ | 0.232 | 0.057 | −0.009 | 0.074 |
| p value | 0.067 | 0.659 | 0.942 | 0.565 |
| MV | ||||
| ρ | 0.347 | 0.254 | 0.074 | −0.033 |
| p value | 0.005 | 0.045 | 0.563 | 0.795 |
- BCVA = best-corrected visual acuity, CRT = central retinal thickness, EIFL = ectopic inner foveal layer, ELM = external limiting membrane, EZ = ellipsoid zone, MH = metamorphopsia score for horizontal line, MV = metamorphopsia score for vertical line.
- ρ: Spearman's rank correlation coefficient.
Table 3 shows the relationship between postoperative visual functions (logMAR BCVA, MH and MV) and preoperative OCT parameters. No correlation was observed between postoperative logMAR BCVA and all the preoperative OCT parameters. Regarding metamorphopsia scores, there was a significant correlation between postoperative MH and preoperative CRT (p = 0.048) and between postoperative MV and preoperative CRT and EIFL (p = 0.002 and 0.0006 respectively). In addition, both postoperative MH and postoperative MV did not correlate with preoperative outer retinal layer structure.
| Postoperative visual Function | Preoperative OCT parameters | |||
|---|---|---|---|---|
| CRT (μm) | EIFL (μm) | ELM disruption | EZ disruption | |
| LogMAR BCVA | ||||
| ρ | 0.202 | 0.043 | −0.159 | −0.153 |
| p value | 0.112 | 0.737 | 0.214 | 0.23 |
| MH | ||||
| ρ | 0.25 | 0.149 | −0.011 | 0.154 |
| p value | 0.048 | 0.243 | 0.929 | 0.23 |
| MV | ||||
| ρ | 0.38 | 0.422 | 0.068 | 0.124 |
| p value | 0.002 | 0.0006 | 0.595 | 0.334 |
- BCVA = best-corrected visual acuity, CRT = central retinal thickness, EIFL = ectopic inner foveal layer, ELM = external limiting membrane, EZ = ellipsoid zone, MH = metamorphopsia score for horizontal line, MV = metamorphopsia score for vertical line.
- ρ: Spearman's rank correlation coefficient.
Table 4 shows the relationship between postoperative visual functions (logMAR BCVA, MH and MV) and postoperative OCT parameters. Postoperative logMAR BCVA did not correlate with any of the postoperative OCT parameters. For metamorphopsia scores, postoperative MH correlated with postoperative CRT and EIFL (p = 0.001 and 0.002 respectively), and postoperative MV also correlated with postoperative CRT and EIFL (p = 0.0008 and < 0.0001 respectively). No significant correlation between postoperative metamorphopsia scores and postoperative outer retinal layer structure was observed, similar to preoperative OCT findings.
| Postoperative visual Function | Postoperative OCT parameters | |||
|---|---|---|---|---|
| CRT (μm) | EIFL (μm) | ELM disruption | EZ disruption | |
| LogMAR BCVA | ||||
| ρ | 0.19 | 0.1 | 0.004 | 0.094 |
| p value | 0.135 | 0.438 | 0.976 | 0.463 |
| MH | ||||
| ρ | 0.406 | 0.382 | −0.061 | 0.162 |
| p value | 0.001 | 0.002 | 0.637 | 0.206 |
| MV | ||||
| ρ | 0.411 | 0.581 | −0.025 | 0.19 |
| p value | 0.0008 | <0.0001 | 0.844 | 0.135 |
- ρ: Spearman's rank correlation coefficient.
- BCVA = best-corrected visual acuity, CRT = central retinal thickness, EIFL = ectopic inner foveal layer, ELM = external limiting membrane, EZ = ellipsoid zone, MH = metamorphopsia score for horizontal line, MV = metamorphopsia score for vertical line.
Multiple regression analysis was performed by the least squares method using postoperative MH or MV as dependent variable and preoperative and postoperative OCT parameters having significant correlation with postoperative metamorphopsia scores as independent variables (Table 5). This analysis identified EIFL as the only independent variable associated with postoperative MV (p = 0.042).
| Postoperative metamorphopsia score | Preoperative CRT (μm) | Postoperative CRT (μm) | Preoperative EIFL (μm) | Postoperative EIFL (μm) |
|---|---|---|---|---|
| MH | ||||
| β | 0.053 | 0.155 | * | 0.322 |
| p value | 0.717 | 0.323 | * | 0.074 |
| MV | ||||
| β | 0.007 | 0.051 | 0.051 | 0.427 |
| p value | 0.965 | 0.749 | 0.762 | 0.042 |
- BCVA = best-corrected visual acuity, CRT = central retinal thickness, EIFL = ectopic inner foveal layer, ELM = external limiting membrane, EZ = ellipsoid zone, MH = metamorphopsia score for horizontal line, MV = metamorphopsia score for vertical line.
- β: Standardized partial regression coefficient.
- * Preoperative EIFL was not included in this multiple regression analysis because this variable did not correlate with postoperative MH.
Discussion
In this study, we studied patients who underwent vitrectomy for the treatment of ERM and compared the relationship between the quantity of metamorphopsia and OCT parameters including EIFL, a new OCT marker of ERM proposed by Govetto et al. (2017), before and after PPV. We found a significant association between metamorphopsia scores and EIFL thickness both before and after surgery. Many previous reports have indicated that visual acuity and metamorphopsia of ERM patients are improved by surgery (Falkner-Radler et al. 2010; Kinoshita et al. 2012; Bae et al. 2013; Kim et al. 2013; Okamoto et al. 2015; McGowan et al. 2016; Kishi et al. 2019; Bae et al. 2020). In the present study, we also observed significant improvements in visual acuity and metamorphopsia scores both for horizontal lines and vertical lines at 3 months after surgery compared to baseline, but we found no significant correlation between EIFL and visual acuity both before and after surgery. In this study, 52 patients (82.5%) underwent simultaneous cataract surgery, which possibly had a confounding effect on the analysis of visual acuity. However, previous reports have shown no significant relationship between visual acuity and metamorphopsia scores in ERM patients (Matsumoto et al. 2003; Arimura et al. 2005; McGowan et al. 2016). Therefore, we consider that cataract surgery does not affect the analysis of the relationship between the extent of metamorphopsia and OCT findings before and after vitrectomy in this study.
Several studies have highlighted the importance of the structure of the inner retinal layers that can be observed on OCT as a prognostic factor of visual function after ERM surgery. Watanabe et al. (2009) used the Amsler chart to classify ERM patients into three groups according to the extent of metamorphopsia and reported that patients with broad metamorphopsia had a thicker INL than patients with no metamorphopsia. Using M-CHARTS to measure metamorphopsia, Okamoto et al. (2012, 2015) and Kim et al. (2013) reported a significant correlation between INL thickness and metamorphopsia score in ERM patients before and after surgery and proposed INL thickness as a predictor of the extent of metamorphopsia after surgery. However, the mechanism for the association between metamorphopsia and INL as a retina inner layer remains unclear. In the present study, a significant association was also found between metamorphopsia and EIFL observed in the inner retinal layer of patients with advanced ERM. It has been speculated that contraction of the ERM exerts traction on the retina causing distortion of the alignment of photoreceptor cells and resulting in metamorphopsia (Ooto et al. 2011; Midena & Vujosevic 2015). Other studies have shown that traction stress of the retina induces activation and proliferation of Müller cells (Lindqvist et al. 2010) and that vitreous concentrations of CD163 (a marker of M2 macrophage) and macrophage-colony stimulating factor are higher in ERM eyes with EIFL compared with those without EIFL (Baek et al. 2020). Based on these findings, it is possible that diverse factors such as physical displacement of tissue due to retinal contraction caused by ERM traction, proliferation of Müller cells and fibrosis induced by M2 macrophages are involved in the development of EIFL and that the presence of EIFL may indicate strong traction and contraction of retina caused by the ERM.
In this study, structural disruption of outer retinal layers including ELM and EZ did not correlate with visual acuity or metamorphopsia. Several previous studies have found no significant association between EZ disruption and metamorphopsia in ERM eyes (Ooto et al. 2011; Kinoshita et al. 2012; Okamoto et al. 2012, 2015), which support our present finding. On the contrary, Bae et al. (2013) reported that eyes with broadly disrupted photoreceptor inner segment and outer segment (IS/OS) junction before ERM surgery had significantly poorer postoperative metamorphopsia than eyes with intact or mildly disrupted IS/OS junction. Conversely, Takabatake et al. (2018) reported the possibility that postoperative metamorphopsia was milder when EZ disruption was present before vitrectomy for ERM. Given the paucity of reports indicating a significant association between EZ disruption and metamorphopsia in ERM, no consensus has been reached. Further research on metamorphopsia and outer retinal layer structure using OCT-related indicators is needed.
Kinoshita et al. (2012) reported that while metamorphopsia score for horizontal lines continued to improve up to 12 months after ERM surgery, metamorphopsia score for vertical lines reached a plateau at 6 months, and improvement of metamorphopsia score at 12 months after surgery was significantly less for vertical lines than for horizontal lines. Due to the course of retinal nerve fibres and the presence of the optic nerve head, the posterior pole retina is considered to have greater plasticity in the vertical direction than in the horizontal direction. In the present study, evaluation was conducted up to 3 months after surgery. Although there was no significant difference in improvement between horizontal and vertical metamorphopsia, metamorphopsia score for vertical lines correlated with EIFL thickness both before and after vitrectomy, and multiple regression analysis identified postoperative EIFL thickness as the only independent factor associated with postoperative metamorphopsia score for vertical lines. The reason why EIFL is strongly associated with metamorphopsia score for vertical lines is not clear, but vertical metamorphopsia is less likely to improve than horizontal metamorphopsia (Kinoshita et al. 2012), and the results of this study suggest that EIFL is a potential predictor of the prognosis of metamorphopsia.
This study has some limitations. The study was retrospective in design with a relatively small sample size. Furthermore, the observation period was only 3 months after surgery, which is not an adequate period. It has been reported that both improvement of metamorphopsia and reduction in EIFL thickness continue up to a maximum of 12 months after ERM surgery in some patients (Govetto et al. 2019; Coppola et al. 2021). Further study with a larger sample size and longer observation period is requited to verify the present findings. Since no device with functions that automatically detect EIFL and measure its thickness is available, CRT and EIFL thickness were measured manually on OCT image using the calliper function, which posed a problem with reproducibility. Moreover, measurement error may increase when determination of the foveal centre is difficult. Further methodological improvement is required to address these issues. Technical improvement in differentiating and measuring retinal layers on OCT will also be important.
In conclusion, the results of this study suggest that EIFL thickness after ERM surgery is a potential indicator of postoperative metamorphopsia, and continued research is warranted.