Hemi-macular detachment: EnFace optical coherence tomography characteristics and clinical implications
A definitive diagnosis of foveal attachment in retinal detachment (RD) can only be obtained by preoperative optical coherence tomography (OCT). Herein, we report the incidence and characteristics of RD patients with hemi-macular detachment (HMD), a distinct clinical subgroup, and its particular postoperative evolution. HMD is defined as a partially detached macula on preoperative OCT with subretinal fluid (SRF) covering up to half of the foveal region and extending continuously towards the retinal periphery.
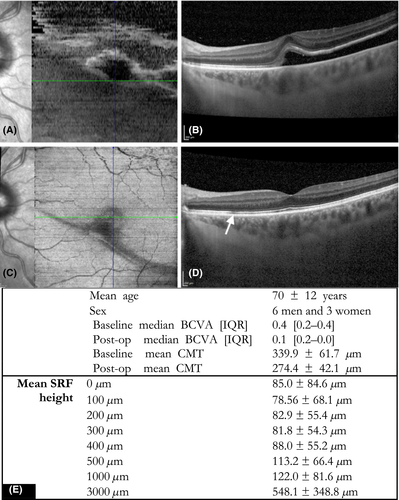
A prospective study of 204 patients with primary RD showed nine cases with distinct HMD on OCT images at presentation (4.4%). Patients underwent 23-gauge pars plana vitrectomy with internal tamponade. EnFace OCT images were taken preoperatively and 1 month after surgery, and central macular thickness (CMT) and height of SRF were measured. The maximal SRF height was determined for the following 8 radii measured from the fovea (0 (subfoveal), 100, 200, 300, 400, 500, 1000 and 3000 μm). LogMAR best-corrected visual acuity (BCVA) was measured preoperatively and at 1 month at which time blurriness or distortions in the central vision were recorded if present.
Most RDs (7/9) and all retinal breaks were superior temporal and the symptoms were of short duration (4 days). Preoperatively SRF formed a circular subfoveal pocket (height 85 ± 85 μm), decreasing at peripheral border of the fovea (82.9 ± 55.4 μm at 200 μm). Shallow RD persisted paracentrally (113.2 ± 66.4 μm at 500 μm) up to the vascular arcades, where SRF height increased (548.1 ± 348.8 μm at 3000 μm). Postoperative BCVA at month 1 was 0.1 [0.2–0.0] logMAR, and some patients described metamorphopsia (5/8) and blurred vision (6/8). Hyporeflective zones within the ellipsoid layer were visible on EnFace OCT forming a watermark along the former RD border (Fig. 1).
These visual disturbances may correspond to structural modifications in the retina due to mechanically induced alterations at the border between the attached and detached retina and by a delayed localized glial reaction to the kinking of the retina along the border of RD (Fisher et al. 2005). From clinical experience, an extension of a peripheral RD into the macula is considered inevitable with time, but surprisingly, the conversion from HMD into full-blown macula-OFF RD while awaiting surgery is rare (Ho et al. 2006). In animal models of RD induced by injection of fluid into the subretinal space, strong intraretinal adhesions were described and a similar resistance was noted in humans during macular translocation surgery (Mruthyunjaya et al. 2004), indicating that these adhesions are sufficiently strong to impede RD extension and conversion into total RD in certain circumstances.
It is interesting to note that the foveal RD remained very shallow in all patients only increasing peripherally towards the vascular arcades. We observed a parafoveal ring which appears to contain submacular fluid accumulation. In postoperative images, the former limit of RD extension is clear, presenting as modifications in the outer retinal layers. These changes may be due to photoreceptor outer segment degeneration or apoptosis during RD (Fisher et al. 2005). Modifications such as parafoveal thinning, hyporeflectivity and/or pigment migrations in the ellipsoid layer using standard OCT have been described in addition to demarcation lines, which are present in 30% of patients with RD (Saleh et al. 2014). These changes were associated with poorer visual function and particularly with persistent metamorphopsia, which corresponds well with our results (Murakami et al. 2017).
It is not clear why the extension beyond HMD is inhibited in such a limited number of cases. Postoperatively HMD is in all cases associated with a watermark at the border of RD in the macular area which presents as hyporeflective zones or tissue densifications in the ellipsoid layer on OCT. These changes may be representative of other cellular mechanisms during the development of the RD in the macula thus limiting its progression.