Efficacy of aflibercept for polypoidal choroidal vasculopathy in Caucasians
Polypoidal choroidal vasculopathy (PCV) is characterized by polypoidal lesions of the choroid with distinct epidemiological and genetic differences between Asians and Caucasians (Lima et al. 2011; Liu et al. 2015). Very few studies have explored the Caucasian PCV and its treatment. Here, we report the outcome of aflibercept treatment on Caucasian patients with PCV beyond the first year.
Twenty-nine eyes of 26 patients (aged 71 ± 9 years, 59% females) with PCV were prospectively included for this study. All patients underwent a complete ophthalmic examination: dilated fundus examination, measurement of best-corrected visual acuity (BCVA) using Early Treatment of Diabetic Retinopathy Study (ETDRS) chart, spectral domain optical coherence tomography (SD-OCT) and retinal angiography. Polypoidal choroidal vasculopathy (PCV) was diagnosed where ≥1 polyps were detected in early-phase indocyaninegreen angiography with or without a branching vascular network. Lesions were mostly extramacular (48% peripapillary; 14% peripheral) and the greatest linear dimension was 2.567 ± 2.148 μm. As an induction treatment, all patients received three consecutive monthly intravitreal aflibercept. During the maintenance phase, intravitreal aflibercept was repeated on a PRN basis. Injections were given by physicians or specially trained injecting nurses (Rasul et al. 2016). Patients were assessed continuously after each set of injections. Photodynamic therapy (PDT) was administered in cases with lack of or little response to anti-VEGF treatment. The majority of patients were treatment-naïve. Twelve eyes had received ranibizumab prior to switching to aflibercept, and the time from aflibercept change was considered baseline.
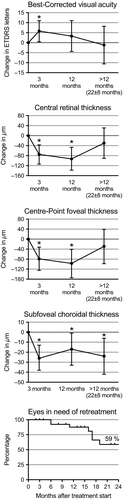
Baseline BCVA was 62 ± 17 ETDRS letters. Treatment improved BCVA with one line after 3 months, but not on long term (Fig. 1). Although BCVA on average could be held at a stable level at >12 months, every third patient experienced extreme changes at >12 months: four eyes (20%) had a worsening of 3 + lines and three eyes (15%) had an improvement in 3 + lines.
Worse baseline BCVA predicted better long-term response in ΔBCVA after 12 months (R2=0.356; p = 0.002) and >12 months (R2=0.269; p = 0.019). Baseline BCVA correlated with early response, which we defined as ΔBCVA after 3 months (Pearson's ρ = −0.794; p < 0.001). Better early response predicted a better long-term response in ΔBCVA after 12 months (R2=0.409; p < 0.001) and >12 months (R2=0.419; p = 0.002).
Centre-point foveal thickness (CPFT), central retinal thickness (CRT) and subfoveal choroidal thickness (SCT) were measured using OCT scans (Subhi et al. 2016). CRT thickness decreased from 396 ± 134 μm at onset of treatment, but the decrease did not persist after >12 months (Fig. 1). A similar pattern was observed for CPFT. SCT decreased from 245 ± 57 μm at treatment start and remained decreased throughout the follow-ups.
On average, 7.6 ± 3.4 injections were given per eye. Only seven eyes (24%) needed additional PDT. No major adverse events, retinal detachment or endophthalmitis were observed. A Kaplan–Meier analysis showed that eyes in need of retreatment were 88% after 12 months and 59% after 24 months (Fig. 1).
This is one of few studies to report treatment results of PCV in Caucasians and the first study to report results of aflibercept treatment beyond the first year. We ran the analyses separately for the treatment-naïve, which did not change the direction of the results or the conclusions. Overall, we found a short-term improvement in the BCVA, which on long term was more of a stabilization. Unlike in our Caucasian patients, lesions are more often located macular in Asians, which may explain why Asians present with a worse baseline BCVA but also experience a better treatment response (Kikushima et al. 2017; Lee et al. 2017). Hence, the relative worse response in terms of BCVA improvement in our Caucasian patients is likely a question of more peripherally located lesions that remains relatively unaffected by anatomical improvements from the treatment.