Prevalence of myopic retinopathy in rural Central India
Abstract
Purpose
The aim of this study was to determine the prevalence of myopic retinopathy (MR) in rural Central India.
Methods
The population-based Central India Eye and Medical Study included 4711 subjects (aged 30+ years). The participants underwent a detailed eye examination, including fundus photography. Myopic retinopathy was defined according to the Pathologic Myopia Study Group.
Results
Readable fundus photographs were available on 4561 (96.8%) subjects (8846 eyes). Myopic retinopathy was present in 15 (0.17 ± 0.04%; 95% confidence interval (CI):0.08%, 0.26%) eyes of 11 (0.24 ± 0.07%; 95%CI: 0.01, 0.04) individuals. Myopic retinopathy occurred only in eyes with an axial length of >26 mm. Eyes with MR had significantly larger optic discs than eyes without MR (3.69 ± 1.22 mm2 versus 2.52 ± 0.77 mm2; p < 0.001). In binary regression analysis, higher prevalence of MR was associated with longer axial length (p < 0.001; odds ratio (OR): 19.6; 95%CI: 4.6, 82.9), higher prevalence of open-angle glaucoma (p = 0.02; OR: 16.1; 95%CI: 1.51, 170), lower best-corrected visual acuity (expressed in logMAR) (=0.03; OR: 0.06; 95%CI: 0.004, 0.75) and female gender (p = 0.002). If level of education was added to the model, educational level was not significantly associated with MR (p = 0.17; OR: 0.53; 95%CI: 0.22, 1.31). If gender was dropped from the model, higher prevalence of MR was associated with lower educational level (p = 0.04; OR: 0.44; 95%CI: 0.20, 0.97).
Conclusions
Prevalence of MR in rural Central India was low (11/4561 or 0.2%), and correlated with a 16 times higher risk of open-angle glaucoma, after adjusting for axial length and gender. If gender was excluded from the analysis, higher prevalence of MR was associated with lower educational level. This latter finding distinguishes adult MR from today′s school children myopia which is strongly associated with higher educational level.
Introduction
In East Asia and South East Asia, the prevalence of myopia has profoundly increased during the last three decades (Xu et al. 2005; Morgan et al. 2012; Wu et al. 2015). In studies from metropolitan regions such as Beijing, Shanghai and Seoul, 80–90% of the 18-year-old school children were myopic, and approximately 10–20% of the school children were highly myopic with a myopic refractive error of more than −6 dioptres (Sun et al. 2012; You et al. 2014; Wu et al. 2015). These figures for the school children generation were considerably higher than those for the elderly generation living in the same geographical regions (Xu et al. 2005). Although myopia was much less common in the generation of the parents than in the generation of the school children and university students, myopia was already one of the three most common causes for visual impairment, blindness and visual field defects in the elderly population in East Asia (Xu et al. 2005). To cite examples, myopic retinopathy was the second most frequent cause of visual impairment and blindness in the Taiwanese Shihpai Eye Study (Hsu et al. 2004). The Singapore Tanjong Pagar survey showed that 9% of unilateral or bilateral blindness was due to degenerative myopia (Wong et al. 2000). Taking into account that myopia-related sequels such as myopic maculopathy and high myopia associated glaucomatous optic neuropathy usually develop after an age of 30 or 40 years, and extrapolating the figures of the prevalence of high myopia in today′s school children into the future, when these school children have grown older, one may anticipate a further increase in the prevalence of myopia as blinding disease. It has remained unclear, however, whether today′s school children myopia is congruent to, or will develop into, the type of high myopia which is associated with pathological retinopathy in today′s elderly individuals.
Since the marked increase in the prevalence of myopia mostly occurred in fast developing regions and countries such as China, Singapore and South Korea, we performed this study to examine the prevalence of myopic retinopathy in a population mostly untouched by technological and infrastructural development. We therefore conducted this population-based study in rural Central India close to the Indian tribal belt. Searching for differences in the prevalence of myopic retinopathy and its associations between populations living in East Asian metropolitan regions and in a population living in rural Central India may help to address the questions whether today′s school children myopia differs from today′s adult myopia.
Patients and Methods
The Central India Eye and Medical Study (CIEMS) is a population-based cross-sectional study in rural Central India (Nangia et al. 2010). The Medical Ethics Committee of the Medical Faculty Mannheim of the Ruprecht-Karls-University Heidelberg and the ethics committee of the Suraj Eye Institute/Nagpur approved the study; all participants gave informed consent, according to the Declaration of Helsinki. Of a total population of 13 606 villagers, 5885 subjects met the inclusion criterion of an age of 30+ years, and were thus eligible for the study. Of these 5885 subjects, 4711 participated, resulting in a response rate of 80.1%.
The study participants were examined in the hospital during a full day of evaluations. These included a detailed ophthalmologic examination with refractometry and visual acuity assessment, keratometry, Goldmann applanation tonometry, slit lamp biomicroscopy and photography of the cornea, lens, optic disc and macula. Ocular pachymetry and biometry were carried out via sonography using the Pacscan (Sonomed, Lake Success, NY, USA). The anterior chamber was assessed by the technique of Herrick and by gonioscopy. Gonioscopy was performed for all study participants in dim illumination using the magnaview single mirror gonio lens (Ocular Instruments, Bellevue, WA, USA). Fundus photographs were graded in a masked manner for signs of myopic retinopathy by experienced ophthalmologists (RG, KB, VN, JBJ). In cases of doubt, the photographs were re-examined by a panel (VN, JBJ). The fundus photographs were digitized and the optic disc structures were measured. The optic disc was defined as all area within the parapapillary ring. The image magnification caused by the optic media of the eye and by the fundus camera was corrected applying method of the Littmann and Bennett (Littmann 1982; Bennett et al. 1994). Myopic retinopathy was defined as described recently by the Pathologic Myopia Study Group (Ohno-Matsui et al. 2015). Myopic retinopathy was graded into five categories including ‘no myopic retinal lesion’ (Category 0), ‘tessellated fundus’ (Category 1), ‘diffuse chorioretinal atrophy’ (Category 2), ‘patchy chorioretinal atrophy’ (Category 3) and ‘macular atrophy’ (Category 4). Four additional features to supplement these categories were defined as ‘plus’ lesions, namely, lacquer cracks, myopic choroidal neovascularization Fuchs′ spot and posterior staphyloma. Using fundus photographs, we assessed also the presence of retinal vein occlusions, diabetic retinopathy and glaucomatous optic neuropathy, as defined and described in detail previously (Nangia et al. 2008, 2013; Jonas et al. 2010).
Only those subjects with assessable fundus photographs were included in the study described herein. Statistical analysis was performed using a commercially available statistical software package (spss for Windows, version 22.0, SPSS, Chicago, IL, USA). We first calculated the mean prevalence of myopic retinopathy, expressed as mean ± standard error. We then assessed associations between the prevalence of myopic retinopathy and other ocular and general parameters in a univariate manner. Finally, we carried out a multivariate binary regression analysis with the prevalence of myopic retinopathy as dependent parameter and all parameters, which were significantly associated with myopic retinopathy in the univariate analysis, as independent variables. We calculated the odds ratios (OR) and the 95% confidence intervals (CI). All p-values were two-sided and were considered statistically significant when the values were <0.05.
Results
Of the 4711 individuals, readable fundus photographs were available on 4561 (96.8%) subjects (8846 eyes). Myopia defined as a myopic spherical equivalent of equal to or >−1.00 dioptres was present in 1352 (15.3%) eyes of 759 (16.6%) individuals. High myopia defined as a refractive error ≤−8 dioptres was present in 46 (0.5%) eyes, and an axial length ≥26.0 mm was present in 35 (0.4%) eyes.
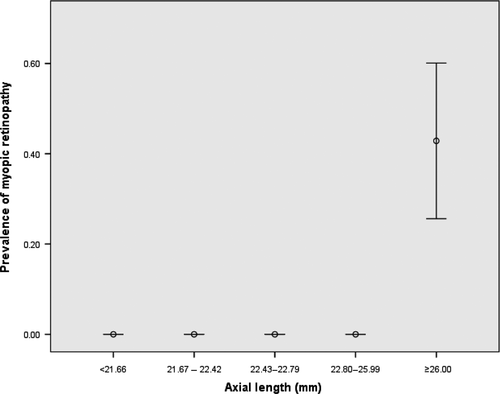
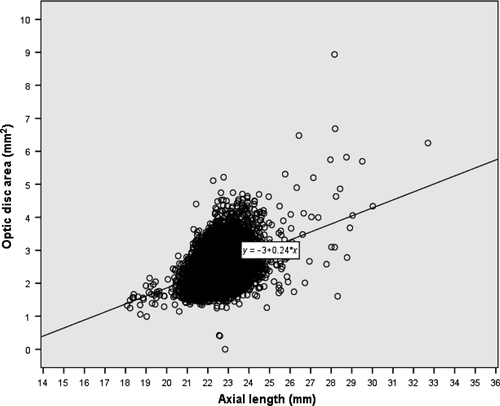
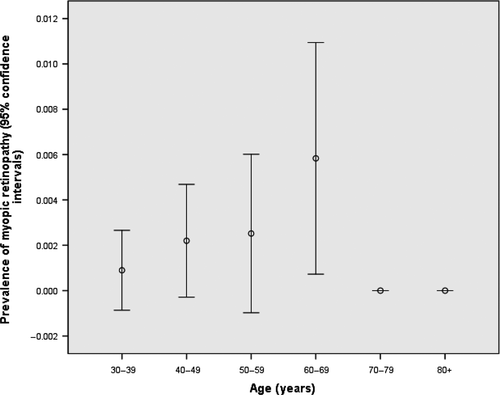
Myopic retinopathy was present in 15 (0.17 ± 0.04%; 95%CI: 0.08%, 0.26%) eyes of 11 (0.24 ± 0.07%; 95%CI: 0.01, 0.04) individuals (Table 1). Subjects with myopic retinopathy had significantly worse best-corrected visual acuity (p < 0.001) than did those without myopic retinopathy. In the eyes with myopic retinopathy, eight (53%) eyes had a best-corrected visual acuity of worse than 20/60 and equal to or better than 20/400, and five (33%) eyes had a best-corrected visual acuity of worse than 20/400. Correspondingly, four (36%) subjects had low vision (best-corrected visual acuity in the better eye of worse than 20/60 and equal to or better than 20/400) and one (9%) subject was blind (best-corrected visual acuity in the better eye <20/400). Using the United States (US) standard and defining blindness as best-corrected visual acuity in the better-seeing eye of <2/20 and defining visual impairment as best-corrected vision of <20/40 and equal to or better than 2/20, 6 (54%) subjects had low vision and 1 (9%) subject was blind. The prevalence of myopic retinopathy increased significantly with longer axial length (p < 0.001) and with increasing myopic refractive error (p < 0.001). Myopic retinopathy occurred only in eyes with an axial length of more than 26 mm (Fig. 1). Eyes with myopic retinopathy had significantly larger optic discs than eyes without myopic retinopathy (3.69 ± 1.22 mm2 versus 2.52 ± 0.77 mm2; p < 0.001) (Fig. 2). In a parallel manner, the vertical disc diameter was significantly longer in the myopic retinopathy group (2.46 ± 0.43 mm versus 1.85 ± 0.90 mm; p = 0.003), whereas the horizontal disc diameter did not differ significantly (p = 0.10) between both groups. Subsequently, the ratio of vertical disc diameter to horizontal disc diameter was significantly higher in the group with retinopathy (1.32 ± 0.23 versus 1.09 ± 0.50; p = 0.02). Taking the whole study population, the individuals with myopic retinopathy and those without myopic retinopathy did not vary significantly regarding gender (p = 0.07) and age (p = 0.14) (Table 1). If only individuals with an age of <70 years were included, the prevalence of myopic retinopathy significantly increased with older age (p = 0.02). For the individuals with an age of 70+ years, prevalence of myopic retinopathy was zero and thus not related with age (Fig. 3).
| Myopic retinopathy | No myopic retinopathy | p-value | |
|---|---|---|---|
| Number eyes | 15/8846 | 8831/8846 | |
| Number of individuals | 11 | 4550 | |
| Men/Women | 3/8 | 2111/2439 | 0.07 |
| Age (Years) | 52.8 ± 10.7 | 48.5 ± 12.8 | 0.14 |
| Body height (cm) | 150 ± 11 | 157 ± 9 | 0.04 |
| Body weight (kg) | 43.5 ± 8.7 | 48.9. ± 10.4 | 0.03 |
| Body mass index | 19.1 ± 2.9 | 19.8 ± 3.4 | 0.40 |
| Level of education | 0.9 ± 1.1 | 1.4 ± 1.3 | 0.10 |
| Anterior corneal curvature radius (mm) | 7.53 ± 0.27 | 7.58 ± 0.28 | 0.51 |
| Central corneal thickness (μm) | 506 ± 27 | 514 ± 33 | 0.26 |
| Anterior chamber depth (mm) | 3.22 ± 0.23 | 3.24 ± 0.35 | 0.79 |
| Lens thickness (mm) | 4.25 ± 0.47 | 3.97 ± 0.47 | 0.06 |
| Axial length (mm) | 29.0 ± 2.4 | 22.6 ± 0.8 | <0.001 |
| Refractive error (Dioptres) | −10.6 ± 8.2 | −0.05 ± 1.59 | <0.001 |
| Best-corrected visual acuity (LogMAR) | 1.38 ± 0.90 | 0.11 ± 0.27 | <0.001 |
| Intraocular pressure (mm Hg) | 15.9 ± 2.9 | 13.7 ± 3.3 | 0.01 |
| Optic disc area (mm2) | 3.69 ± 1.21 | 2.52 ± 0.77 | <0.001 |
| Early age-related macular degeneration | 0/15 | 2.8 ± 0.2% | 1.00 |
| Late age-related macular degeneration | 0/15 | 0.1 ± 0.03% | 1.00 |
| Retinal vein occlusion | 0/15 | 36/8580 (0.4 ± 0.1%) (95%CI: 0.3, 0.6) | 1.00 |
| Diabetic retinopathy | 0/15 | 20/8583 (0.2 ± 0.1%) (95%CI: 01, 0.3) | 1.00 |
| Open-angle glaucoma | 11/4 (73 ± 12) (48, 97) | 145/8831 (1.6 ± 1.4) (1.4, 1.9) | <0.001 (OR: 165 (95%CI: 52, 524)) |
| Angle-closure glaucoma | 0/15 | 16/8831 (0.2 ± 0.05) (0.1, 0.3) | 1.00 |
The multivariate binary regression analysis included the presence of myopic retinopathy as dependent variable and as independent variables all those parameters for which the p-value in the univariate analysis was ≤0.10. Step by step, we first dropped refractive error due to its collinearity with axial length. We then dropped lens thickness (p = 0.96), body weight (p = 0.72), level of education (p = 0.57), intraocular pressure (p = 0.95) and optic disc area (p = 0.53), so that in the final model, higher prevalence of myopic maculopathy was associated with longer axial length (p < 0.001; OR: 19.6; 95%CI: 4.6, 82.9), higher prevalence of open-angle glaucoma (p = 0.02; OR: 16.1; 95%CI: 1.51, 170), lower best-corrected visual acuity (expressed in logMAR) (p = 0.03; OR: 0.06; 95%CI: 0.004, 0.75) and female gender (p = 0.002; OR: 257; 95%CI: 7.4, 8937). If level of education was added to the model, educational level was not significantly associated with the prevalence of myopic maculopathy (p = 0.17; OR: 0.53; 95%CI: 0.22, 1.31). If gender was dropped from the model, higher prevalence of myopic maculopathy was associated with lower educational level (p = 0.04; OR: 0.44; 95%CI: 0.20, 0.97).
In a reverse manner, higher prevalence of glaucomatous optic neuropathy was significantly associated with higher prevalence of myopic retinopathy (p < 0.001; OR: 24.5; 95%CI: 5.7, 105), larger optic disc size (p < 0.001; OR: 1.99; 95%CI:1.40, 2.83), higher intraocular pressure (p < 0.001; OR: 1.23; 95%CI: 1.18, 1.29) and worse best-corrected visual acuity (logMAR) (p < 0.001; OR: 5.01; 95%CI: 3.52, 7.14). Axial length, if added to the model, was not significantly associated with glaucoma prevalence.
Discussion
In our population-based study in rural central India, myopic retinopathy was present in 11 (0.02%) out of 4561 individuals. Myopic retinopathy occurred only in eyes with an axial length of more than 26 mm. Eyes with myopic retinopathy had significantly larger optic discs than eyes without myopic retinopathy (p < 0.001). In multivariate analysis, higher prevalence of myopic maculopathy was correlated with longer axial length (p < 0.001), higher prevalence of open-angle glaucoma (p = 0.02), lower best-corrected visual acuity (p = 0.03) and female gender (p = 0.002). If gender was dropped from the model, higher prevalence of myopic maculopathy was associated with lower educational level (p = 0.04) (Jonas et al. 2016a).
The prevalence of myopic retinopathy in our study was considerably lower than in previous investigations performed in East Asia or Australia, with a prevalence of myopic retinopathy 3.1% in the Beijing Eye Study on individuals aged 45+ years, a prevalence of 1.2% in the Australian Blue Mountains Eye Study and a prevalence of 11.3% a recent study from Hong Kong (Vongphanit et al. 2002; Lai et al. 2008; Liu et al. 2010). This finding is paralleled by the markedly lower prevalence of myopia and of high myopia in the rural Central Indian population as compared to the populations in the East Asian metropolitan regions (Wong et al. 2000; Hsu et al. 2004; Xu et al. 2005; Nangia et al. 2010; Jung et al. 2012; Morgan et al. 2012; Sun et al. 2012; Wu et al. 2015). In particular, our Central Indian rural study population was markedly less myopic than the Indian population in Singapore as examined in the Singapore Indian Eye Study (Pan et al. 2011) in which additionally the prevalence of myopia among second-generation (or higher) Indian immigrants in Singapore was higher than among first-generation immigrants (Pan et al. 2012).
As in the previous studies, the prevalence of myopic retinopathy in our study increased with the amount of myopia (Gözüm et al. 1997; Liu et al. 2010; Neelam et al. 2012) (Fig. 2). Interestingly, if the whole study population was considered, the prevalence of myopic retinopathy in our study was not significantly associated with age (Table 1) (Fig. 3). This finding was in contrast to an observation made in previous studies such as the Blue Mountains Study and an investigation from Hong Kong (Vongphanit et al. 2002; Lai et al. 2008). Besides a relatively low number of patients with myopic retinopathy in our study population, another reason for the discrepancy between our study and the previous investigations might have been the effect of a confounding factor. In the younger subgroup with an age of <70 years, however, the prevalence of myopic retinopathy increased with older age, whereas none of the elderly individuals aged 70+ years showed myopic retinopathy. One may postulate that individuals with myopic retinopathy in our rural study setting might have had a lower life expectancy due to the retinopathy associated reduction in vision. This association would have led to a decrease in the prevalence of myopic retinopathy in the elderly population group. A similar observation was made in a previous analysis of our study population which showed an age-related decrease in the prevalence of diabetes mellitus beyond an age of 65 years (Jonas et al. 2010). Also for this, unexpected, decline in the prevalence of an age-related disease such as diabetes mellitus, a disease-associated reduced life expectancy was discussed to be responsible for the observation.
A preponderance of women in the group of patients with myopic retinopathy as present in our study agrees with findings of the study by Lai and colleagues from Hong Kong, and is contrary to the results of the Blue Mountains Study and Beijing Eye Study (Vongphanit et al. 2002; Lai et al. 2008). As the previous studies, also our study showed a marked decrease in visual acuity in the individuals with myopic retinopathy. Reasons for the reduction in vision were the morphological changes associated with myopic retinopathy, namely the diffuse and localized chorioretinal atrophic lesions in association with a marked thinning of the choroid as shown by the degree fundus tessellation (Morgan et al. 2012; Shao et al. 2014; Ohno-Matsui et al. 2015; Yan et al. 2015). The association between myopic retinopathy with a larger optic disc agrees with former histo-morphometric investigations and clinical studies (Jonas & Dichtl 1997). The large optic discs in eyes with myopic retinopathy have been referred to as secondary or acquired macrodiscs (Jonas & Dichtl 1997). The finding of the enlargement of the optic nerve head in eyes with myopic retinopathy suggests that the myopic stretching of the globe occurred mainly in the posterior part of the eye, whereas the anterior segment was not markedly affected. Correspondingly, the central corneal thickness in our study as well as in other investigations did not differ significantly between eyes with myopic retinopathy and those without myopic retinopathy (Table 1) (Pedersen et al. 2005).
As in other studies, prevalence of myopic retinopathy was strongly associated with a higher prevalence of open-angle glaucoma although myopic retinopathy prevalence was not associated with intraocular pressure (Table 1). This finding suggests that normal-intraocular pressure glaucoma was more common in the eyes with myopic retinopathy than in those without retinopathy. A similar observation has been made in previous population-based studies such as the Beijing Eye Study (Xu et al. 2007; Jonas et al. 2009). These findings conform to histomorphometric investigations, in which axially markedly elongated eyes as compared with eyes with normal axial length showed a significantly thinner lamina cribrosa, a shorter distance between the intraocular pressure compartment and the retrobulbar compartment of the orbital cerebrospinal fluid pressure, and a thinner peripapillary sclera (Jonas et al. 2004, 2012, 2016b). Both features, thinning of the lamina cribrosa and thinning and elongation of the peripapillary scleral flange as the biomechanical anchor of the lamina cribrosa have been discussed to increase glaucoma susceptibility (Burgoyne & Morrison 2001). In a reverse manner, higher prevalence of glaucomatous optic neuropathy was associated with higher prevalence of myopic retinopathy (p < 0.001; OR: 24.5) and larger optic disc size (p < 0.001; OR: 1.99) after adjusting for intraocular pressure and best-corrected visual acuity, whereas axial length was not significantly associated with glaucoma prevalence in that model. It confirms a recent hospital-based study on 172 highly myopic patients, in which glaucoma prevalence (which was 28%) was primarily associated with axial myopia associated disc enlargement and not with axial elongation itself (Nagaoka et al. 2015).
Similar to a finding of a previous analysis of our study population, in which the prevalence of high myopia was not significantly with the level of education, this study revealed that the presence of myopic retinopathy was not significantly associated with the level of education in multivariate analysis (Jonas et al. 2016a). If age was dropped from the analysis, higher prevalence of myopic retinopathy was associated even with a lower level of education. These findings agree with the Beijing Eye Study in which the prevalence of myopic retinopathy was neither related with the educational level (Liu et al. 2010). In a high number of recent studies of the young generations of East Asia, a marked increase in the prevalence of myopia and high myopia was strongly associated with higher level of education of the children and teenager and of their parents (Morgan et al. 2012; Wu et al. 2015). Although myopic retinopathy is strongly associated with axial length, the generation examined for school children myopia is yet too young to have developed myopic retinopathy so that there is no evidence that myopic retinopathy is associated with the education in these young populations. The results of our study on adult individuals and the results of the investigations on school children can therefore not directly be compared with each other.
Potential limitations of our study should be mentioned. First, as in any population-based study, selection bias could have accentuated some estimates and masked others. The overall participation rate in our survey was 80.1% what is comparable to other population-based studies. Second, our study was performed in a very rural location which bordered to so-called tribal regions in Central India. Our study population is therefore definitely not typical for the population of India as a whole. The peculiarity of our study was its study population for which the living conditions have not markedly changed within the last 100 years. Our study population may thus be considered as an extreme in the spectrum of study populations living at different levels of socioeconomic development. Third, our study as cross-section investigation did not allow statements on a longitudinal association between myopic retinopathy and other parameters, in particular the level of education.
In conclusion, prevalence of myopic retinopathy in rural Central India was low (11/4561 or 0.2%) and correlated with higher frequency of open-angle glaucoma, after adjusting for axial length and gender. If gender was excluded from the analysis, higher prevalence of myopic retinopathy was associated with lower educational level. This finding distinguishes adult myopic maculopathy from today′s school children myopia which is strongly associated with higher educational level.