Corneal confocal microscopy alterations in Sjögren's syndrome dry eye
Abstract
Purpose
To evaluate light backscattering (LB) in corneal layers in patients with primary Sjögren's syndrome dry eye (SSDE) utilizing in vivo corneal confocal microscopy (IVCM) and to determine the eventual association with the lacrimal functional test values.
Methods
A complete ophthalmic evaluation, Schirmer test with and without stimulation, break-up time (BUT) and IVCM were performed on 55 patients affected by SSDE and in an age- and sex-matched cohort of healthy participants (HP). Light backscattering, measures as light reflectivity unit (LRU), detected by IVCM at Bowman's membrane (BM) at 50 μm, at 100 μm and at 200 μm deeper than BM was compared in the two groups. The correlations between LB values and lacrimal function results were evaluated.
Results
In patients affected by SSDE, LB was significantly higher (p < 0.001) in each corneal layer examined (+14 ± 6.33 LRU at BM), compared with HP. A good reverse correlation between the light reflectivity measures at BM with Schirmer test with (r = −0.91) and without (r = −0.90) stimulation and BUT (r = −0.88) was found. Correlations were lower in the deeper corneal layers.
Conclusion
Even if our results should be confirmed in further studies with a larger population, these findings show that IVCM is a device able to detect alterations in corneal layers in SSDE patients related to the lacrimal function. Light backscattering (LB) could be very useful for clinical diagnosis and management of SSDE.
Introduction
Sjögren's syndrome is a chronic autoimmune disease characterized by inflammation and loss of secretory function of the exocrine glands (Peri et al. 2012). It is possible to observe a primary Sjogren syndrome, not associated with other autoimmune disease, or a secondary one, associated to connective tissue alterations as rheumatoid arthritis or systemic lupus erythematosus (Peri et al. 2012). Symptoms traditionally include oral and ocular dryness (Afonso et al. 1999; Pflugfelder et al. 1999; Solomon et al. 2001; Subcommittee of the International Dry Eye Workshop 2007a,b; Tincani et al. 2013). According to the concept of the lacrimal functional unit (Stern et al. 1998), the infiltration of lymphocytes and the release of inflammatory cytokines lead to ocular surface alterations. These changes can bring to neural network destruction and be responsible of reflex tear secretion activation, and this could lead the clinical scenario to evolve in Sjögren syndrome dry eye (SSDE) (Afonso et al. 1999; Pflugfelder et al. 1999; Solomon et al. 2001; Subcommittee of the International Dry Eye Workshop 2007a,b; Tincani et al. 2013). For many years, SSDE has been related to the reduced secretion of the aqueous component in tears (Subcommittee of the International Dry Eye Workshop 2007a,b). Today, there is an undeniable evidence that several factors are involved in the pathogenesis of this disease: inflammation, changes in tears osmolarity, alterations in corneal sensitivity and innervations (Mathers 1998; Stern et al. 1998; Subcommittee of the International Dry Eye Workshop 2007a,b; Tincani et al. 2013).
Devices currently available are often unsatisfactory in the clinical and functional evaluation of SSDE (Mathers 1998; Villani et al. 2007a,b); for this reason, it is very important to test new devices and new parameters to improve the possibilities of an early detection and better management of the disease. New methods to evaluate tear film in dry eye have been purposed: evaluation of high-order aberrations, to measure the refractive influence of unstable tear film (Koh et al. 2014), tear meniscus height topographic measurements (Koh et al. 2015) and tear film thickness measurement with optical coherence tomography (Kaya et al. 2015).
In vivo corneal confocal microscopy (IVCM) has been widely utilized to study corneal microscopic morphology in SSDE and non-Sjögren dry eye (Tuisku et al. 2008; Labbé et al. 2013; Villani et al. 2013). Most of the studies performed so far analyse corneal morphology and corneal innervations (Tuominen et al. 2003; Benítez del Castillo et al. 2004, 2007; Zhang et al. 2005; Villani et al. 2007a,b, 2008; Lin et al. 2010). Light backscattering (LB) measured by IVCM has been proven to be a valid parameter to evaluate corneal inflammation in different clinical situations (Marchini et al. 2006; Morishige et al. 2009; Hillenaar et al. 2012; Schiano-Lomoriello et al. 2014). Assuming the recognized role of inflammation in SSDE pathogenesis (Mathers 1998; Stern et al. 1998; Subcommittee of the International Dry Eye Workshop 2007a,b; Tincani et al. 2013), purpose of this study was to investigate whether LB measured by IVCM in patients with SSDE could be a useful parameter in the diagnosis and management of this disease.
Patients and Methods
In this study, data were collected from 55 patients (54 women and one man) with a mean age of 49.25 ± 11.54 years (range from 24 to 72 years) affected by SSDE and 55 HP, age- and sex-matched. Patients with SSDE were referred at Rheumatology Unit of Santa Maria del Popolo degli Incurabili Hospital (Napoli, Italy) and were monitored for 6 consecutive months. The patients were diagnosed primary Sjogren's syndrome according to the 2012 American-European Classification Criteria (Shiboski et al. 2012). Healthy participants were selected among the subjects routinely screened to undergo refractive surgery during the same period of time at Centro di Servizi di Ateneo ‘Grandi Apparecchiature’ Seconda Università di Napoli (Napoli, Italy).
Exclusion criteria were ocular infection, lymphoma, acquired immune deficiency syndrome (AIDS), sarcoidosis, diabetes mellitus, corneal dystrophies and inflammations, systemic therapy with drugs having corneal toxicity, glaucoma, recent use of drugs with anticholinergic properties, use of contact lenses (within 1 month from the enrolment), history of ocular surgery. None of the patients enrolled was in treatment with glucocorticoid and/or immunosuppressive drugs.
Both patients and HP underwent a refraction test, ocular adnexa and anterior segment evaluation, Schirmer test with (ST I) and without (ST II) stimulation, break-up time (BUT) according to International Dry Eye Workshop 2007 guidelines (Subcommittee of the International Dry Eye Workshop 2007a,b) and finally IVCM; the visit ended with intraocular pressure measurement and fundus evaluation under pupil dilatation. To reduce bias in collecting and analysing data, one physician performed ST1 (SI), a second physician performed ST 2 (GV), a third performed BUT (MB), a fourth performed IVCM (ML) and a fifth analysed data (UAGC).
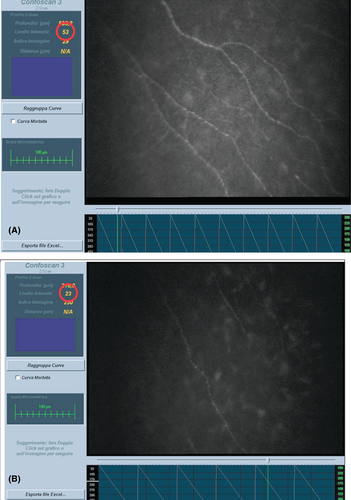
In vivo corneal confocal microscopy (IVCM) was performed using a Confoscan 3 (Nidek technologies, Vigonza, Italy), 20 min after the end of the lacrimal functional tests, to let the corneal surface to be as clear as possible.
The patient sat with chin and forehead supported to stabilize the head, and a drop of anaesthetic (oxybuprocaine chloride 0.4%) was instilled in lower conjunctival fornix before examination. Before starting the scan, the objective lens of the device was covered with gel (hydroxypropyl methylcellulose 0.3%) to avoid the direct contact with corneal surface. A drop of antibiotic (ofloxacin 0.3%) was instilled in the lower conjunctival fornix at the end of each examination and the eye was re-examined at the slit lamp to verify the integrity of the corneal surface.
At full-thickness setting, this device captures 350 images of 440 × 330 μm within 12 seconds at a focal plane along the z-μm. Evaluations for this study have been performed in semi-automatic mode, with a distance between every scan settled at 2 μm; a reference light intensity of 160 was always used, because at this setting, the corneal endothelium was visualized optimally, without image saturation with an average 8-bit pixel intensity. The backscattered and reflected light at the focal plane was captured by a charge-coupled device (CCD) camera with a standard 40× object lens. The Z-scan is a graph showing the depth co-ordinate, expressed in micrometres, on the z-axis and the level of reflectivity expressed in arbitrary numerical units, called light reflectance units (LRU), on the y-axis for each corneal image included in the scan (McLaren et al. 2007, 2010; Labbe et al. 2012). Each scan was carefully evaluated and images of the first stromal layer after the subbasal epithelium, identified as the Bowman's membrane (Schiano-Lomoriello et al. 2014) and the ones at 50 μm, 100 μm and 200 μm deeper from the first one selected, were studied on the Z-scan axis. Three scans per patients were performed and the mean of LRU values at every depth was recorded (Fig. 1), with a 10-min break between every measurement. To reduce the axial movement-related bias, central cornea scans were acquired and evaluated depths up to 200 μm from the basal membrane: patients usually move the eye more at the end of the exam. Moreover, semi-automatic mode was selected to have more reliability in central cornea detection and scans in which possibly bias-related movement was detected and low-quality ones were excluded from this study (three SSDE and four HP).
Statistical analysis
The normal data distribution was verified by Kolmogorov–Smirnov test. For data which did not meet normality, appropriate nonparametric tests were used to evaluate differences and correlations. In particular, Schirmer and LRU values between patients with SSDE and healthy subjects were compared using Mann–Whitney nonparametric U-test and correlations of LRU with BUT, ST I and ST II were studied with the Spearman's rank order correlation method. For all tests, the level of significance was set at p < 0.05. All analyses were performed using spss software (IBM Corp., Armonk, New York, NY, USA) version 18.0.
The study was performed in accordance with the ethical standards stated in the 1964 Declaration of Helsinki and approved by the Santa Maria del Popolo degli Incurabili Hospital, (Napoli, Italy) IRB. Informed consent was obtained from all subjects before examination.
Results
Average values of age and lacrimal function tests performed in patients with SSDE and healthy subjects (HS) are summarized in Table 1.
| SSDE | Healthy controls | Mann–Whitney U-test | |
|---|---|---|---|
| Mean ± SD | Mean ± SD | ||
| Age (years) | 49.25 ± 11.54 | 49.47 ± 11.50 | p > 0.8 |
| Schirmer test I (mm) | 3.60 ± 2.30 | 16.27 ± 4.64 | p < 0.001 |
| Schirmer test II (mm) | 2.07 ± 1.84 | 12.58 ± 3.90 | p < 0.001 |
| BUT (seconds) | 4.15 ± 2.12 | 11.25 ± 1.77 | p < 0.001 |
- SSDE = Sjogren's syndrome dry eye, BUT=break up time.
Optical reflectivity values between patients with SSDE and HP showed a statistically significant difference (p < 0.001) in every layer compared (Table 2) to SS values, higher also in the deepest stromal layers examined.
| SSDE | Healthy controls | Mann-Whitney U test | |
|---|---|---|---|
| Mean ± SD | Mean ± SD | ||
| BM | 34.85 ± 6.33 | 20.89 ± 1.21 | p < 0.001 |
| 50 μm | 29.89 ± 4.50 | 18.91 ± 0.89 | p < 0.001 |
| 100 μm | 27.85 ± 4.10 | 18.07 ± 0.90 | p < 0.001 |
| 200 μm | 26.36 ± 4.90 | 16.89 ± 0.83 | p < 0.001 |
In patients with SSDE, the increase in reflectivity in all layers showed a good reverse correlation with ST I, ST II and BUT (p < 0.001). These correlations appeared to be weaker in the deeper stromal layers (Table 3).
| Correlations in SSDE | |||||
|---|---|---|---|---|---|
| BM | 50 μm | 100 μm | 200 μm | ||
| ST I | Spearman's rho | −0.913 | −0.701 | −0.651 | −0.558 |
| Sig. (2-tailed) | p < 0.001 | p < 0.001 | p < 0.001 | p < 0.001 | |
| N | 55 | 55 | 55 | 55 | |
| ST II | Spearman's rho | −0.901 | −0.670 | −0.643 | −0.506 |
| Sig. (2-tailed) | p < 0.001 | p < 0.001 | p < 0.001 | p < 0.001 | |
| N | 55 | 55 | 55 | 55 | |
| BUT | Spearman's rho | −0.878 | −0.622 | −0.581 | −0.585 |
| Sig. (2-tailed) | p < 0.001 | p < 0.001 | p < 0.001 | p < 0.001 | |
| N | 55 | 55 | 55 | 55 | |
To evaluate eventual influence of age on backscatter, correlations have been analysed both in SSDE than in HP eyes in age-divided groups (Tables 4, 5). No different correlations have been observed compared to the overall statistical study.
| BM | 50 | 100 | 200 | |||
|---|---|---|---|---|---|---|
| SSP age 24–40 | ||||||
| Spearman's rho | SCHIRMER I | Spearman's rho | −0.8193 | −0.5091 | −0.7582 | −0.6109 |
| Sig. (2-tailed) | 0.001 | 0.001 | 0.004 | 0.035 | ||
| N | 12 | 12 | 12 | 12 | ||
| SCHIRMER II | Spearman's rho | −0.6971 | −0.5182 | −0.6400 | −0.5236 | |
| Sig. (2-tailed) | 0.012 | 0.014 | 0.025 | 0.081 | ||
| N | 12 | 12 | 12 | 12 | ||
| BUT | Spearman's rho | −0.8066 | −0.5000 | −0.6073 | −0.5527 | |
| Sig. (2-tailed) | 0.002 | 0.008 | 0.036 | 0.062 | ||
| N | 12 | 12 | 12 | 12 | ||
| SSP age 41–45 | ||||||
| Spearman's rho | SCHIRMER I | Spearman's rho | −0.8951 | −0.7278 | −0.6380 | −0.2999 |
| Sig. (2-tailed) | 0.000 | 0.000 | 0.001 | 0.154 | ||
| N | 24 | 24 | 24 | 24 | ||
| SCHIRMER II | Spearman's rho | −0.8897 | −0.7015 | −0.6322 | −0.3034 | |
| Sig. (2-tailed) | 0.000 | 0.000 | 0.001 | 0.149 | ||
| N | 24 | 24 | 24 | 24 | ||
| BUT | Spearman's rho | −0.9195 | −0.6571 | −0.5171 | −0.3675 | |
| Sig. (2-tailed) | 0.000 | 0.000 | 0.010 | 0.077 | ||
| N | 24 | 24 | 24 | 24 | ||
| SSP age 56–72 | ||||||
| Spearman's rho | SCHIRMER I | Spearman's rho | −0.8892 | −0.7049 | −0.3540 | −0.5466 |
| Sig. (2-tailed) | 0.000 | 0.001 | 0.137 | 0.015 | ||
| N | 19 | 19 | 19 | 19 | ||
| SCHIRMER II | Spearman's rho | −0.9454 | −0.7086 | −0.4936 | −0.6249 | |
| Sig. (2-tailed) | 0.000 | 0.001 | 0.032 | 0.004 | ||
| N | 19 | 19 | 19 | 19 | ||
| BUT | Spearman's rho | −0.6425 | −0.4759 | −0.3100 | −0.5681 | |
| Sig. (2-tailed) | 0.003 | 0.039 | 0.196 | 0.011 | ||
| N | 19 | 19 | 19 | 19 | ||
| BM | 50 | 100 | 200 | |||
|---|---|---|---|---|---|---|
| HS age 26–40 | ||||||
| Spearman's rho | SCHIRMER I | Spearman's rho | −0.5022 | −0.4415 | −0.1124 | −0.4414 |
| Sig. (2-tailed) | 0.139 | 0.201 | 0.757 | 0.202 | ||
| N | 10 | 10 | 10 | 10 | ||
| SCHIRMER II | Spearman's rho | −0.3529 | −0.2958 | −0.0869 | −0.3969 | |
| Sig. (2-tailed) | 0.317 | 0.407 | 0.811 | 0.256 | ||
| N | 10 | 10 | 10 | 10 | ||
| BUTC | Spearman's rho | −0.1011 | 0.1569 | 0.3823 | −0.6212 | |
| Sig. (2-tailed) | 0.781 | 0.665 | 0.276 | 0.055 | ||
| N | 10 | 10 | 10 | 10 | ||
| HS age 41–55 | ||||||
| Spearman's rho | SCHIRMER I | Spearman's rho | −0.0587 | −0.0112 | 0.0360 | −0.0029 |
| Sig. (2-tailed) | 0.776 | 0.957 | 0.861 | 0.989 | ||
| N | 26 | 26 | 26 | 26 | ||
| SCHIRMER II | Spearman's rho | −0.0906 | −0.0234 | −0.0102 | −0.0729 | |
| Sig. (2-tailed) | 0.660 | 0.910 | 0.960 | 0.723 | ||
| N | 26 | 26 | 26 | 26 | ||
| BUTC | Spearman's rho | −0.1110 | 0.0486 | −0.0086 | −0.1659 | |
| Sig. (2-tailed) | 0.589 | 0.814 | 0.967 | 0.418 | ||
| N | 26 | 26 | 26 | 26 | ||
| HS age 56–73 | ||||||
| Spearman's rho | SCHIRMER I | Spearman's rho | −0.0139 | −0.1596 | −0.3928 | −0.5146 |
| Sig. (2-tailed) | 0.955 | 0.514 | 0.096 | 0.024 | ||
| N | 19 | 19 | 19 | 19 | ||
| SCHIRMER II | Spearman's rho | −0.0864 | −0.2205 | −0.4833 | −0.5986 | |
| Sig. (2-tailed) | 0.725 | 0.364 | 0.036 | 0.007 | ||
| N | 19 | 19 | 19 | 19 | ||
| BUTC | Spearman's rho | 0.0953 | −0.1614 | −0.1830 | −0.4027 | |
| Sig. (2-tailed) | 0.698 | 0.509 | 0.453 | 0.087 | ||
| N | 19 | 19 | 19 | 19 | ||
Discussion
Sjogren's syndrome is an autoimmune systemic disease mainly characterized by the hypofunction of salivary and lacrimal glands, resulting in the most commonly reported symptoms of the syndrome: dry eyes and mouth (Peri et al. 2012). The diagnostic devices available today for the clinical evaluation of dry eye patients have low sensibility and little reproducibility, especially in the advanced stages of the disease (Villani et al. 2007a,b; Tincani et al. 2013). Some of the major difficulties in patients with SSDE or dry eye patients are related to early diagnosis and management of the disease because the symptoms reported are very generic and the available tests to evaluate them are not always reliable, although considered as gold standard (Villani et al. 2007a,b; Tincani et al. 2013). Even after diagnosis, the subjective response to therapy and the sensations referred by patients are very different (Tincani et al. 2013). For this reason, it would be important to find a parameter able to reliably measure corneal suffering levels. Corneal inflammation has been recognized to have a role both in the pathogenesis and progression of the disease (Mathers 1998; Stern et al. 1998; Subcommittee of the International Dry Eye Workshop 2007a,b; Villani et al. 2007a,b; Tincani et al. 2013) so, if we could measure it with a reliable parameter, we would have a more objective evaluation of corneal stress. Even if IVCM cannot be considered a new device, LB provided by this instrument has never been examined in patients with SSDE. Although IVCM has some limitations in the evaluation of quantitative parameters, LB measurements are considered reliable in estimating corneal inflammation that occurs after lamellar keratoplasty (Marchini et al. 2006; Schiano-Lomoriello et al. 2014), cataract surgery (phacoemulsification) (Morishige et al. 2009), herpetic stromal keratitis (Hillenaar et al. 2012) or corneal haze (McLaren et al. 2010). Inflammation levels in patients with SSDE are extremely inferior compared with the clinical situations previously mentioned; this is the reason why in this study the values of LB observed were significantly lower (Marchini et al. 2006; Morishige et al. 2009; McLaren et al. 2010; Hillenaar et al. 2012).
In vivo corneal confocal microscopy (IVCM) has the advantage of being a non-invasive, quickly executed and safe examination (Tuisku et al. 2008; Labbé et al. 2013; Villani et al. 2013).
Limits of this study could be addressed in the technique used: IVCM scans can be affected by many artefacts coming from corneal properties and from the device limitations, especially when trying to measure LB. In some cases, it can be difficult to accurately identify the corneal centre; this is the reason why in this study semi-automatic acquisition mode has been chosen: after a much trained physician (ML) detected the better centred endothelial image possible, the scans were acquired without any other interaction with operator. Only high-quality scans, without signs of eye movements that could reduce the LB reliability, were included in the study. In Table 6, variation of LB values of five SSDE eyes included in the study is represented. In vivo corneal confocal microscopy (IVCM) was performed after Schirmer test with and without stimulation and after BUT, to avoid altering corneal transparency and biasing LB measurements, 20 min, occurred between BUT and IVCM, to restore the complete corneal clearness.
| First measurement | Second measurement | Third measurement | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SSP | Age | Sex | BM | 50 | 100 | 200 | BM | 50 | 100 | 200 | BM | 50 | 100 | 200 |
| 3 | 38 | F | 36 | 28 | 27 | 29 | 32 | 29 | 23 | 24 | 29 | 29 | 22 | 23 |
| 14 | 47 | F | 47 | 42 | 46 | 46 | 46 | 46 | 44 | 45 | 47 | 42 | 43 | 40 |
| 23 | 65 | F | 34 | 29 | 29 | 24 | 36 | 32 | 26 | 27 | 36 | 31 | 27 | 26 |
| 36 | 55 | F | 35 | 36 | 26 | 30 | 35 | 39 | 29 | 31 | 36 | 35 | 30 | 28 |
| 50 | 24 | F | 33 | 35 | 26 | 21 | 28 | 32 | 28 | 23 | 30 | 30 | 28 | 23 |
In this study, LB resulted to be higher in patients with SSDE compared to sex- and age-matched HP, therefore this parameter could be useful in differentiating SSDE corneas from healthy ones. The difference in LB could depend on the higher level of inflammation present in SSDE corneas. Correlations observed between LRU values at different corneal levels and lachrymal function tests suggest that LB in the anterior cornea could be related to inflammation level at those stages. Thus, IVCM seems to be able to provide reliable information about cornea of patients with SSDE and it could be used to detect eventual early alterations in the ones of patients showing generic symptoms. It is very common, to underestimate symptoms and signs of these patients when physicians do not find any significant sign at slit lamp examinations (Tincani et al. 2013). If these data would be confirmed in further studies, more focusing on early-stage SSDE patients, LB measurement could be considered a parameter to keep in consideration quantifying corneal suffering without any specific slit lamp sign or symptom referred.
In fact, patients often describe their condition as a ‘gritty’ or ‘sandy’ sensation in their eyes with low correlation with the information coming from slit lamp examination or lachrymal function test (Tincani et al. 2013). This may represent a problem for the physician who first prescribes or modifies a therapy. Light backscattering (LB) evaluation could change the traditional approach and management to SSDE and other kind of dry eye diseases; moreover, it could lead to new research perspectives.
Of course, attention must be paid in applying standard approach to the examinations, to achieve reliable information; results provided by IVCM about corneal subbasal nerve analysis, for example, are still conflicting (Labbe et al. 2012).
In conclusion, even if these results should be confirmed in further studies with a larger population, these data show that LB, provided by IVCM, could be very useful for better understanding the correlation between functional and structural anomalies in SSDE.