Infusion flow related retinal breaks in 25G vitrectomy
The details of four patients with infusion jet flow-related breaks during macular hole surgery are provided in Table 1. Individual cases are as discussed below.
| Patient number | Age/sex | Eye | Best-corrected vision | Tamponade | Macular hole closure | Lens status | IRB site | Follow-up months | |
|---|---|---|---|---|---|---|---|---|---|
| Pre-op | Post-op | ||||||||
| 1 | 57 yr/F | OS | 20/60 | 20/60 | C3F8 | Type-2 | Phakic | SNQ | 3 |
| 2 | 52 yr/M | OD | 20/60 | 20/30 | SOI | Type-1 | Phakic | SNQ | 9 |
| 3 | 64 yr/F | OS | 20/80 | 20/30 | C3F8 | Type-1 | Pseudophakia. | ITQ | 10 |
| 4 | 57 yr/M | OD | 20/400 | 20/200 | SOI | Type-2 | Phakic | SNQ | 7 |
- OD = right eye, OS = left eye, yr = year, M = male, F = female, HTN = hypertension, DM = diabetes mellitus, pre-op = preoperative, post-op = postoperative, C3F8 = perfluoropropane, SOI = silicone oil, SNQ = superonasal quadrant, ITQ = inferotemporal quadrant, IRB = iatrogenic retinal break.
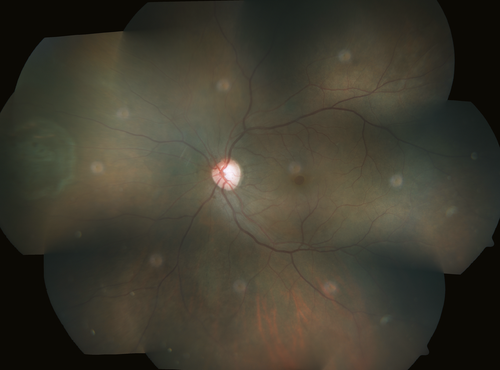
Case 1
A 57-year-old gentleman underwent combined phacoemulsification with intraocular lens implantation and vitrectomy for idiopathic full thickness macular hole (FTMH). After 25G core vitrectomy, posterior vitreous detachment (PVD) was induced by suction from vitreous cutter and extended till the vitreous base. Intraocular pressure (IOP) was maintained at 30 mmHg with aspiration rate of 400–450 mmHg. Brilliant blue G (BBG) 0.05% dye (Ocublue Plus; Aurolab, Madurai, India) was used to stain the internal limiting membrane (ILM) in air-filled eye for 1 minute. Infusion fluid was restarted to exchange air with fluid to proceed for ILM peeling. A radial full thickness retinal break developed at the mid-peripheral retina in the supero-nasal quadrant (SNQ) along the jet of fluid from infusion cannula during the process of air–fluid exchange. Internal limiting membrane (ILM) peeling was performed around the macular hole with inverted flap technique and laser photocoagulation performed around the peripheral retinal break. Fourteen percentage C3F8 gas tamponade was used. Six weeks after surgery, macular hole was closed (type 2) and retina remained attached to the last follow-up, 3 months following surgery (Fig. 1).
Case 2
A 52-year-old male underwent 25G vitrectomy for idiopathic FTMH in right eye. Intraocular pressure (IOP) was maintained at 30 mmHg with aspiration rate of 400–450 mmHg. After triamcinolone assisted PVD induction with active suction, fluid–air exchange was performed to stain the ILM with BBG0.05% dye (Ocublue Plus; Aurolab). Infusion fluid was restarted to exchange the air with fluid. A sudden, transient hypotony led to a pressurized visible jet of fluid from infusion cannula creating a radial iatrogenic retinal break (IRB) in the upper nasal quadrant in the mid-peripheral retina with a localized retinal detachment and trapped subretinal air. Internal limiting membrane (ILM) was peeled around the macular hole, sub-retinal fluid was drained through the peripheral retinal break, fluid–air exchange was performed, laser retinopexy was done around the peripheral break, and silicone oil was injected for endotamponade. Six weeks following surgery, retina was attached with type 1 closure of macular hole. Nine months following vitrectomy, silicone oil was removed with phacoemulsification and intraocular lens implantation, improving the vision to 20/30.
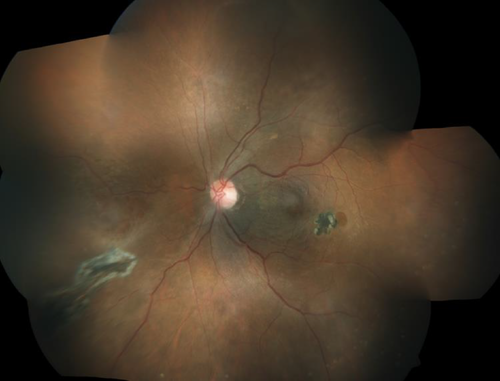
Case 3
A 64-year-old lady underwent vitrectomy in her pseudophakic right eye for idiopathic FTMH. Intraocular pressure (IOP) was maintained at 30 mmHg with aspiration rate of 400–450 mmHg. Following vitrectomy, fluid–air exchange was performed to stain the ILM with BBG 0.05% dye (Ocublue Plus; Aurolab). As the air was exchanged with fluid, a jet of fluid created a radial IRB in the infero-temporal quadrant along the trajectory. The ILM was peeled around the macular hole, and laser photocoagulation was performed around the peripheral retinal break. Perfluoropropane (C3F8; 14%) gas tamponade was used. Six weeks after surgery, type 1 macular hole closure was achieved and best-corrected vision improved to 20/30 that was maintained till the last follow-up of 10 months. Later, the patient developed an atrophic retina hole near the preexisting chorioretinal scar temporal to fovea (Fig. 2).
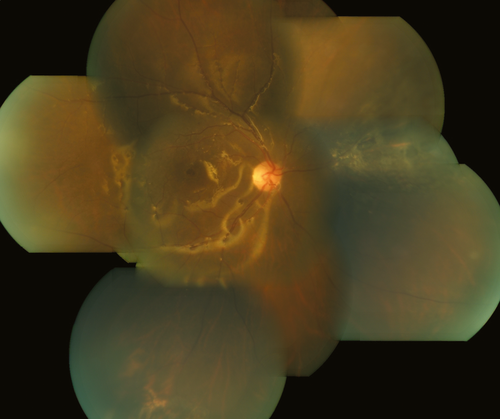
Case 4
A 57-year-old gentleman presented with idiopathic FTMH. He underwent vitrectomy with 25G Microincision vitrectomy system (MIVS). Intraocular pressure (IOP) was maintained at 30 mmHg with aspiration rate of 400–450 mmHg. The ILM was stained with BBG 0.05% dye (Ocublue Plus; Aurolab) in air-filled eye. Fluid was restarted to exchange the air to proceed with ILM peeling but there was a transient hypotony followed by a jet of fluid landing in the supero-nasal quadrant that created a radial retinal break with subretinal trapped air and a localized retinal detachment. After the ILM peeling, retina was settled with fluid–air exchange and endo-drainage through the IRB. Laser retinopexy was done around the peripheral break, and silicone oil was injected for endotamponade. Six weeks following surgery, type II closure of macular hole was noted, and retina was attached, with a vision of 20/200, maintained till the last follow-up at 7 months (Fig. 3).
Despite the advances in instrumentation and surgical techniques, IRBs remain a serious intraoperative complication resulting in additional surgical steps and possibly poor visual results (Steel & Charles 2011; Bilgin et al. 2015). New-generation vitrectomy machines have refined the pressure control system to stabilize intraoperative pressure compensation and maintain constant IOP independent of aspiration flow rates during cutting/aspiration modes. The infusion pressure is increased as near to real time as possible to allow rapid infusion pressure changes required to be instituted (Sugiura et al. 2013).
These set-ups can have bizarre flow rates if instruments are taken off from the ports or ports are non-valved. The sudden drop in intraocular pressure alerts the IOP control system which automatically increases the inflow, resulting in rapidly evolving fountain effect from the ports. This inflow–outflow mismatch can be more serious while performing air–fluid exchange through 25G system using active aspiration or when the sclerotomy port is left open. Air outflow can be extremely high under these circumstances, while fluid inflow is low by comparison. This leads to sudden but transient hypotony, activating the IOP compensation mechanism leading to a dramatic increase in inflow which may result in mechanical injury to retina at the diagonally opposite quadrant of infusion port where the fluid jet falls. In all the four described cases in this series, we observed a specific situation where the infusion flow in an air-filled eye while using a vitrectomy machine with IOP compensation mechanism and 25G ports created IRB. All the surgeries were carried out using non-valved port system and the relatively narrow 25G inflow tubings, where the time taken to compensate for pressure changes is sometimes disproportionate, as mentioned above. Bilgin et al. (2015) had recently discussed three patients where insult by infusion jet of fluid precipitated new breaks. The indication of vitrectomy was different in these patients, and retina was already compromised by primary pathology such as retinal detachment, diabetic retinopathy and oil-filled eye after primary retinal detachment surgery. Authors blamed high inflow limit of 6 ml/min causing retinal injury and recommended decreasing inflow rate to 4 ml/min.
Sugiura et al. (2015) studied intra-operative IOP fluctuation during different surgical maneuvers in experimental animals using Alcon constellation vision system. Authors noted that with 25G vitrector in cutting mode under standard flow rates, it took 2.6 seconds to return to preset IOP levels after the initial drop. The same preset pressure of 30 mmHg dropped to 12.2 mmHg under aspiration mode and took 2.6 seconds to return to preset levels under default flow rates. During both these observations, authors did not find any complications as the time to compensate IOP change remains negligible (Sugiura et al. 2013). In contrast, dynamic control of IOP may differ with air–fluid exchange and may create IRBs on normal or diseased retina.
Kim et al. (2014) in intraocular jet flow analysis observed that in air-filled vitreous cavity, the pressure measured at vulnerable points (area of retina diagonal to direction of infusion jet) was approximately twofold to threefold greater than infusion pressure. The pressure initially increased to 62.6, 130.2 and 184.2 mmHg at infusion pressure of 20, 40 and 60 mmHg, respectively. Infusion of pressurized air can be damaging to retina in the opposite quadrant of infusion, and there is a correlation between location of visual field defect and that of infusion cannula placement (Hirata et al. 2000). All four surgeries in the present series used infusion pressure setting of 30 mmHg, and reducing the settings further to 20–25 mmHg may further reduce the chances of IRB.
We caution the surgeons to reduce the infusion flow rates in Alcon Constellation vitrectomy system in the 25G MIVS settings to address this potential problem of infusion flow-related IRB. We also recommend valved port systems and suggest avoiding rapid aspiration of air during air–fluid exchange to prevent unexpected hypotony. In addition, we suggest caution while leaving the ports open during air–fluid exchange in non-valved 25G MIVS.
Infusion of pressurized fluid jet from infusion cannula in air-filled eyes with 25G vitrectomy systems with IOP compensation mechanism has the potential to create iatrogenic retinal break in healthy attached retina. Refinement in inflow rate by real-time change especially in the beginning of different modes may address this problem. There should be a co-ordination between different modes, inflow and outflow match and various small gauge vitrectomy systems under different conditions including air–fluid or fluid–air dynamics.