Early use of non-vitamin K antagonist oral anticoagulants after cardiac surgery compared with warfarin for postoperative atrial fibrillation
Abstract
Background
The introduction of non-vitamin-K-antagonist oral anticoagulants (NOAC) has shifted the landscape of anticoagulation in the setting of atrial fibrillation (AF), as an alternative to warfarin. Despite extensive evidence for NOACs in non-perioperative and non-valvular AF, there remains little consensus on anticoagulation choice for patients with postoperative atrial fibrillation (POAF) after cardiac surgery.
Methods
This retrospective, observational study included 2263 patients who underwent cardiac surgery between 1 March 2016 and 13 January 2023 at a tertiary cardiac centre. Patients with pre-existing AF, valvular AF and transcatheter interventions were excluded. Short- and long-term outcomes were compared between patients who received a NOAC and those who received warfarin for POAF. A Cox regression model was constructed to identify independent predictors for time-to-mortality. Subgroup analysis was performed based on the type of surgery, including CABG-only, aortic valve replacement (AVR)-only, and combined surgery cohorts.
Results
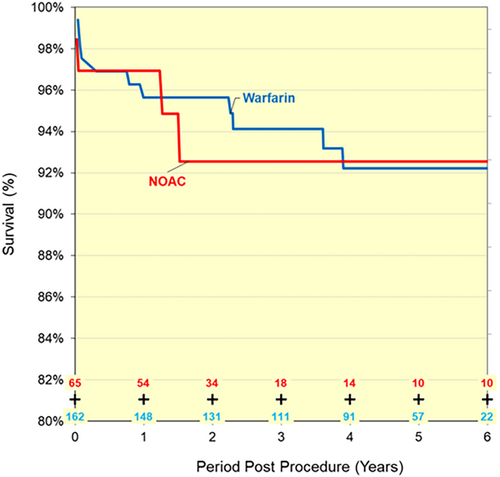
Of the 2263 patients, 556 (24.5%) developed POAF. Of those who developed POAF, 162 were anticoagulated with warfarin and 65 were anticoagulated with a NOAC, including apixaban, rivaroxaban and dabigatran. There were three cases of permanent stroke in the warfarin group compared with no cases in the NOAC group. All-cause 30-day and one-year readmission rates were similar between groups. The use of NOAC or warfarin did not impact overall survival in the Kaplan–Meier analysis. Subgroup analysis demonstrated similar outcomes in CABG-only, AVR-only and combined surgery groups.
Conclusions
Warfarin and NOAC performed similarly in short- and long-term complications, suggesting NOAC as a plausible alternative to warfarin for anticoagulation in POAF.
Introduction
Postoperative atrial fibrillation (POAF) is common following cardiac surgery, occurring in 20% to 42% of patients, most frequently within the first 3 days.1, 2 While POAF is usually self-limiting, it is associated with up to a fivefold risk of recurrent atrial fibrillation (AF) in the following 5 years.2, 3 It is also a risk factor for thromboembolism, myocardial infarction and mortality, compared with non-POAF patients.4 Despite extensive evidence for Non-vitamin-K-antagonist Oral Anticoagulants (NOAC) in the non-perioperative setting, there remains no clear consensus on anticoagulation choice for patients with POAF after cardiac surgery.
Warfarin, a vitamin K antagonist, was used as a first-line choice of anticoagulation from the 1950s until the introduction of NOACs. The narrow therapeutic range, frequency of monitoring, dietary and drug interactions are important limitations of the anticoagulant. However, warfarin remains first-line for patients with valvular AF. The NOACs, which include rivaroxaban, apixaban and dabigatran in Australia, mitigate the disadvantages of warfarin, offering fixed dosing, fewer interactions and less need for monitoring. Given these benefits and non-inferiority to warfarin, NOACs are the first-line therapy to reduce thromboembolic risk in non-valvular AF. However, the landmark trials for NOACs excluded any reversible cause of AF, such as the postoperative cohort. Thus, the anticoagulant choice for POAF remains largely based on clinician preference.
Current international guidelines do not provide specific recommendations on the use of NOACs or warfarin in the setting of POAF after cardiac surgery. The American Heart Association (AHA) 2023 Guidelines recommend anticoagulation for 60 days after surgery as category IIa evidence, with little elaboration on anticoagulation choice.5 The European Society of Cardiology 2020 Guidelines also proposed class IIb evidence that long-term oral anticoagulant therapy may be considered in POAF after cardiac surgery, considering the clinical benefit and patient preferences.6 These recommendations were based on expert consensus and small retrospective studies.
In recent years, studies comparing NOACs and warfarin in POAF after cardiac surgery have been limited by small samples, lack of generalizability, exclusion of valve procedures and inconsistent data definitions in the literature.1 Despite the lack of substantial evidence, NOAC use after bioprosthetic valve replacement has increased from 6.6% to 32.1% between 2011 and 2014 to 2015 and 2018, respectively.7 Given the evolving landscape with the introduction of NOAC reversal agents, a contemporary review of anticoagulation choice for POAF after cardiac surgery is warranted. We aimed to compare early and long-term outcomes of patients who are prescribed warfarin or a NOAC for POAF after cardiac surgery. Specifically, the main outcome measures were operative mortality, permanent stroke or transient ischemic attack, all-cause readmission, readmission for anticoagulant complication and postoperative length of stay.
Methods
This retrospective, single-institutional study has been approved with a waiver of consent by the Gold Coast University Hospital Human Research Ethics Committee (LNR/2022/QGC/90325), in accordance with the principles of the Declaration of Helsinki. Data were collected from the cardiothoracic surgical database of a single tertiary cardiac centre from 1st March 2016 to 13th January 2023. The exclusion criteria were mechanical valve replacements, mitral stenosis, pre-existing AF and those who underwent transcatheter interventions. The rationale for excluding those with pre-existing AF was twofold. Firstly, while poorly understood, the pathophysiology of intrinsic pre-existing/permanent/paroxysmal AF differs from that which occurs after cardiac surgery, where there has been significant manipulation of the heart and physiological alterations such as cardioplegia. Secondly, the preference for anticoagulation in these patients was to return them to the preadmission anticoagulant in the absence of any indications for warfarin, representing an inherent bias towards NOAC as it is the anticoagulant of choice for paroxysmal AF. Of the 2584 consecutive patients, 321 were excluded according to the above criteria.
The local cardiothoracic surgical database corresponds to the Australian and New Zealand Society of Cardiac and Thoracic Surgeons (ANZSCTS) Cardiac Surgery Database, to maintain the consistency of data definitions.8 POAF was defined as a new onset of AF requiring treatment, which excludes the recurrence of AF that was present preoperatively. The decision for warfarin or a NOAC was based on surgeon preference. Permanent stroke was defined as a central neurological deficit persistent for more than 72 h peri- or postoperatively caused by an ischemic or hemorrhagic event. Transient stroke or transient ischemic attack was defined as a new transient central neurological deficit that was completely resolved within 72 h. Anticoagulant complication refers to any bleeding, haemorrhage and/or embolic events related to anticoagulant therapy. Readmission with anticoagulant complication refers to an inpatient readmission within 30 days of surgery due to an anticoagulant complication (i.e., haemorrhage associated with demonstrated over anticoagulation or thrombosis or embolism associated with demonstrated under-anticoagulation). Readmission for pericardial effusion is defined as an inpatient readmission within 30 days of surgery for the treatment of pericardial effusion.
All statistical analyses were conducted using SPSS Statistics software (IBM, SPSS Inc.) and Microsoft Excel. Demographic and clinical variables were summarized with descriptive statistics. Time-to-event analyses were performed on the long-term mortality data obtained via linkage with the Australian Births, Deaths and Marriages registry. A Cox proportional hazards model was constructed to identify independent predictors for time-to-mortality. The census date was 30 March 2023. Subgroup analysis was performed based on the type of surgery (i.e., CABG, valve or both).
Results
Of the 2263 patients undergoing cardiac surgery, 556 patients (24.5%) developed POAF. Of the patients who developed POAF, 162 were anticoagulated with warfarin and 65 were anticoagulated with a NOAC. The choice of NOAC used was apixaban in 16 patients, rivaroxaban in 19 patients and dabigatran in 30 patients. There was no significant difference between the warfarin and NOAC group in age, BMI, Indigenous status, hypertension, smoking history, diabetes, dyslipidemia, cerebrovascular disease, previous MI, NYHA class or urgency of surgery (Table 1).
| Patient characteristics | NOAC | Warfarin | Total | P-value | |||
|---|---|---|---|---|---|---|---|
| Age | 72 | (63–77) | 71 | (64–76) | 71 | (64–76) | 0.737 |
| Gender (Male) | 52 | 80.0% | 123 | 75.9% | 175 | 77.1% | 0.509 |
| Height | 174 | (165–180) | 172 | (166–178) | 173 | (166–178) | 0.589 |
| Weight | 85 | (75–94) | 81 | (71–92) | 82 | (73–93) | 0.152 |
| BMI | 28.4 | (26.3–31.3) | 27.2 | (24.9–30.4) | 27.7 | (25.2–30.7) | 0.131 |
| Indigenous | 2 | 3.1% | 3 | 1.9% | 5 | 2.2% | 0.570 |
| Hypertension | 44 | 67.7% | 115 | 71.0% | 159 | 70.0% | 0.624 |
| Smoking history | 37 | 56.9% | 88 | 54.3% | 125 | 55.1% | 0.722 |
| Diabetes | 16 | 24.6% | 23 | 14.2% | 39 | 17.2% | 0.060 |
| Hypercholesterolemia | 35 | 53.8% | 98 | 60.5% | 133 | 58.6% | 0.358 |
| Cerebrovascular disease | 3 | 4.6% | 19 | 11.7% | 22 | 9.7% | 0.102 |
| Peripheral vascular disease | 1 | 1.5% | 10 | 6.2% | 11 | 4.8% | 0.142 |
| Infective endocarditis | 0 | 0.0% | 1 | 0.6% | 1 | 0.4% | 0.526 |
| Respiratory disease | 10 | 15.4% | 16 | 9.9% | 26 | 11.5% | 0.239 |
| Previous MI | 17 | 26.2% | 39 | 24.1% | 56 | 24.7% | 0.742 |
| History of CHF | 11 | 16.9% | 19 | 11.7% | 30 | 13.2% | 0.296 |
| Cardiogenic shock | 2 | 3.1% | 7 | 4.3% | 9 | 4.0% | 0.664 |
| LVEF percentage | 60 | (49–65) | 60 | (53–64) | 60 | (52–65) | 0.854 |
| LVEF estimate | 0.248 | ||||||
| Normal (LVEF >60%) | 26 | 44.8% | 61 | 41.2% | 87 | 42.2% | - |
| Mild (LVEF 46–60%) | 21 | 36.2% | 70 | 47.3% | 91 | 44.2% | - |
| Moderate (LVEF 30–45%) | 10 | 17.2% | 13 | 8.8% | 23 | 11.2% | - |
| Severe (LVEF <30%) | 1 | 1.7% | 4 | 2.7% | 5 | 2.4% | - |
| Missing | 7 | - | 14 | - | 21 | - | - |
| CCS class | 0.550 | ||||||
| 0 | 33 | 50.8% | 90 | 55.6% | 123 | 54.2% | - |
| 1 | 7 | 10.8% | 27 | 16.7% | 34 | 15.0% | - |
| 2 | 8 | 12.3% | 15 | 9.3% | 23 | 10.1% | - |
| 3 | 9 | 13.8% | 15 | 9.3% | 24 | 10.6% | - |
| 4 | 8 | 12.3% | 15 | 9.3% | 23 | 10.1% | - |
| NYHA class | 0.813 | ||||||
| I | 31 | 47.7% | 87 | 53.7% | 118 | 52.0% | - |
| II | 17 | 26.2% | 41 | 25.3% | 58 | 25.6% | - |
| III | 13 | 20.0% | 27 | 16.7% | 40 | 17.6% | - |
| IV | 4 | 6.2% | 7 | 4.3% | 11 | 4.8% | - |
| Preoperative haemoglobin | 139 | (129–146) | 139 | (128–147) | 139 | (129–147) | 0.943 |
| Preoperative creatinine | 82 | (68–102) | 84 | (73–99) | 84 | (72–101) | 0.782 |
| Renal dialysis | 0 | 0.0% | 1 | 0.6% | 1 | 0.4% | 0.526 |
| Status | 0.568 | ||||||
| Elective | 35 | 53.8% | 101 | 62.3% | 136 | 59.9% | - |
| Urgent | 20 | 30.8% | 45 | 27.8% | 65 | 28.6% | - |
| Emergency | 7 | 10.8% | 12 | 7.4% | 19 | 8.4% | - |
| Salvage | 3 | 4.6% | 4 | 2.5% | 7 | 3.1% | - |
| Type of procedure | |||||||
| CABG | 42 | 64.6% | 73 | 45.1% | 115 | 50.7% | 0.008 |
| Valve | 29 | 44.6% | 100 | 61.7% | 129 | 56.8% | 0.019 |
| Aortic valve | 26 | 40.0% | 86 | 53.1% | 112 | 49.3% | 0.075 |
| Mitral valve | 4 | 6.2% | 13 | 8.0% | 17 | 7.5% | 0.628 |
| Other cardiac | 9 | 13.8% | 16 | 9.9% | 25 | 11.0% | 0.388 |
| Cardiopulmonary bypass | 64 | 98.5% | 158 | 97.5% | 222 | 97.8% | 0.666 |
| Cumulative cross clamp time | 74 | (47–97) | 80 | (64–100) | 78 | (61–99) | 0.042 |
| Cardiopulmonary bypass time | 92 | (71–130) | 106 | (85–136) | 103 | (84–134) | 0.030 |
| IABP | 4 | 6.2% | 3 | 1.9% | 7 | 3.1% | 0.090 |
When considering operative characteristics, the warfarin group had longer cumulative cross clamp and cardiopulmonary bypass time, reaching statistical significance (P = 0.042 and P = 0.03 respectively), however, this was not thought to be a clinically important difference. There was no significant difference in the use of intra-aortic balloon pumps between the two groups. A higher proportion of the CABG subgroup received NOAC over warfarin (64.6% vs. 45.1%, P = 0.008), while a higher proportion of the valve surgery subgroup received warfarin over NOAC (61.7% vs. 44.6%, P = 0.019).
The postoperative outcomes have been summarized in Table 2. There were three cases of permanent stroke in the warfarin group compared with 0 cases in the NOAC group. There was a higher rate of readmission within 30 days in the warfarin group compared with the NOAC group, although this did not reach statistical significance (16.7% vs. 10.8%, P = 0.26). This rate of readmission was not driven by anticoagulant complications. The all-cause 1-year readmission rate was similar between groups (33.8% in NOAC vs. 32.6% in the warfarin group). The median postoperative length of stay was 9 days for patients on NOAC, compared to 8 days in the warfarin group (P = 0.03). The all-cause mortality was similar between the two groups at 30 days (3.1% NOAC vs. 1.9% warfarin, P = 0.340) and 90 days (3.1% NOAC vs. 2.5% warfarin, P = 0.796).
| Early postoperative outcomes | NOAC | Warfarin | Total | P-value | |||
|---|---|---|---|---|---|---|---|
| New permanent stroke | 0 | 0.0% | 3 | 1.9% | 3 | 1.3% | 0.269 |
| New transient ischemic attack | 1 | 1.5% | 1 | 0.6% | 2 | 0.9% | 0.502 |
| 30-day all-cause readmission | 7 | 10.8% | 27 | 16.7% | 34 | 15.0% | 0.260 |
| 30-day readmission for anticoagulant complication | 0 | 0.0% | 1 | 0.6% | 1 | 0.4% | 0.526 |
| 30-day readmission for arrhythmia management | 2 | 3.1% | 9 | 5.6% | 11 | 4.8% | 0.432 |
| 1-year all-cause readmission | 22 | 33.8% | 52 | 32.1% | 74 | 32.6% | 0.800 |
| Postoperative length of stay | 9 | (7–14) | 8 | (7–14) | 9 | (7–14) | 0.030 |
| Mortality during admission | 2 | 3.1% | 2 | 1.2% | 4 | 1.8% | 0.340 |
| Mortality within 30 days | 2 | 3.1% | 3 | 1.9% | 5 | 2.2% | 0.570 |
| Mortality within 90 days | 2 | 3.1% | 4 | 2.5% | 6 | 2.6% | 0.796 |
Of the 556 patients who developed POAF, 339 were not anticoagulated. Those who were on anticoagulation (either NOAC or warfarin) had a significantly higher one-year all-cause readmission rate (32.6% vs. 1.8%, P < 0.05), but the reasons for readmission were widely variable and not limited to anticoagulation complications. There was no difference between those who were or were not anticoagulated in the incidence of new permanent stroke (1.2% vs. 1.3%, respectively, P = 0.881), transient ischemic attack (0.3% vs. 0.9%, respectively, P = 0.347), 30-day mortality (2.4% vs. 1.8%, P = 0.628) and 90-day mortality (2.9 vs. 2.6%, P = 0.829).
The Cox regression analysis found that the main factors impacting survival are age, BMI and NYHA class and emergent/salvage surgery (Table 4, Fig. 2). The use of NOAC or warfarin did not significantly impact overall survival in the time-to-event analysis (Fig. 1). The subgroup analyses of CABG-only, valve-only or CABG and valve surgery demonstrated no significant difference in early or late outcomes including stroke, 30-day and one-year readmission rate and postoperative length of stay (Table 3).
| CABG-only | AVR-only | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Early postoperative outcomes | NOAC | Warfarin | Total | P | NOAC | Warfarin | Total | P | ||||||
| New permanent stroke | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | N/A | 0 | 0.0% | 1 | 1.9% | 1 | 1.5% | 0.618 |
| New transient ischemic attack | 1 | 2.4% | 1 | 1.4% | 2 | 1.7% | 0.690 | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | N/A |
| 30-day all-cause readmission | 7 | 16.7% | 8 | 11.0% | 15 | 13.0% | 0.382 | 0 | 0.0% | 11 | 20.8% | 11 | 16.7% | 0.072 |
| 30-day readmission for anticoagulant complication | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | N/A | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | N/A |
| 30-day readmission for arrhythmia management | 2 | 4.8% | 1 | 1.4% | 3 | 2.6% | 0.272 | 0 | 0.0% | 5 | 9.4% | 5 | 7.6% | 0.249 |
| 1-year all-cause readmission | 14 | 33.3% | 22 | 30.1% | 36 | 31.3% | 0.722 | 5 | 38.5% | 15 | 28.3% | 20 | 30.3% | 0.475 |
| Postoperative length of stay | 10 | 8–15 | 0 | 7–13 | 9 | 8–14 | 0.138 | 9 | 7–9 | 7 | 6–10 | 8 | 6–10 | 0.384 |
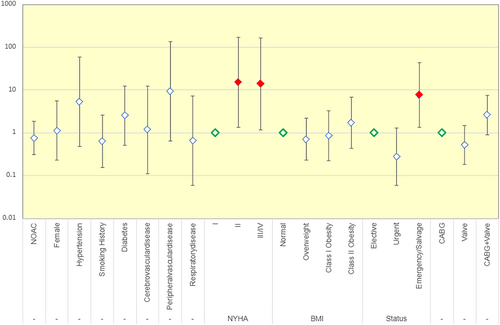
| B | SE | Wald | df | Sig. | Exp(B) | |
|---|---|---|---|---|---|---|
| Age | 0.13 | 0.047 | 7.515 | 1 | 0.006 | 1.139 |
| NYHA Class I | 9.751 | 3 | 0.021 | |||
| NYHA Class II | 1.918 | 1.21 | 2.513 | 1 | 0.113 | 6.808 |
| NYHA Class III | 2.31 | 1.184 | 3.804 | 1 | 0.051 | 10.076 |
| NYHA Class IV | 4.21 | 1.401 | 9.036 | 1 | 0.003 | 67.373 |
| Mitral valve surgery | 3.04 | 0.898 | 11.472 | 1 | 0.001 | 20.905 |
| BMI | 0.213 | 0.073 | 8.399 | 1 | 0.004 | 1.237 |
| Type | 0.24 | 0.347 | 0.475 | 1 | 0.49 | 1.271 |
Discussion
Given the increasing use of NOACs after cardiac surgery, our aim was to compare the short- and long-term outcomes of patients on warfarin and NOACs for POAF. The incidence of POAF in this study was 24.5%, which is comparable to extensively published incidence rates in the literature.1 The proportion of patients who developed POAF that were anticoagulated was 36.2%, which is consistent with the previously published range from 4% to 43%, although slightly higher than the overall mean of 21%.1
This study demonstrated that there was no significant difference in short-term outcomes, including transient or permanent stroke, rate of readmission at 30 days or 1 year, and all-cause mortality at 1 year. This is consistent with findings from a large multicentre retrospective study investigating NOAC use after CABG and bioprosthetic valve replacement, which found no significant differences between NOAC and warfarin in 30-day mortality, reoperation for bleeding, readmission, pleural effusion requiring drainage.7 The time-to-event analysis also showed no significant difference between groups in long-term mortality outcomes.
In this study, the postoperative length of stay was greater in the NOAC group compared with the warfarin group by 1 day, reaching statistical significance (median of 9 vs. 8 days, respectively, P = 0.03). This contrasts with previous studies reporting a longer postoperative and total length of stay in the warfarin group, suggesting reasons such as a less complex postoperative course in NOAC patients or delay in reaching therapeutic international normalized ratio (INR) levels.7, 9, 10 Other studies found no difference in length of stay, achieving therapeutic anticoagulation with or without bridging on postoperative day five.11-13 A cost analysis study found that warfarin was associated with a lower drug cost ($20.04 vs. $377.91) but higher anticoagulant-related costs ($782.32 vs. $377.99), yielding a higher overall cost for warfarin use in the first 30 days.13 This was attributed to the higher costs of INR assays and ground transportation required for laboratory testing.
Of particular note, dabigatran was the most frequently used NOAC in this study (46%), followed by rivaroxaban (29%) and apixaban (24%). This is markedly different from previous studies, such as Anderson et al. (2015) who reported only one of 27 (3.7%) patients on dabigatran, Yu et al. (2019) who reported four of 64 (6.2%) and Woldendorp et al. (2012) who reported 19 of 29 (17.2%) of patients on dabigatran.11-13 The variability in NOAC choice reflects the lack of evidence surrounding its use in POAF and is largely based on surgeon preference. Due to the delicate balance of the coagulopathic state after cardiac surgery, dabigatran was favoured in this institution due to the presence of an available reversal agent. This study therefore provides additional insight into the influence of NOACs including dabigatran after cardiac surgery, which was previously heavily skewed towards apixaban and rivaroxaban. Even with a larger proportion of patients on dabigatran, this study demonstrated similarly low rates of bleeding complications or stroke in both NOAC and warfarin groups. Only one patient in the entire cohort required readmission for an anticoagulant complication, which highlights that, whatever the anticoagulant chosen, significant complications appear to be rare.
Despite a large cohort of patients, there were only three cases of postoperative stroke, representing 1.3% of the patients who developed postoperative atrial fibrillation, comparable to that which is reported in the literature.14 A meta-analysis by Gaudino et al.14 including 174, 969 patients, investigated early versus delayed stroke after cardiac surgery and found that the pooled event rate for early and delayed stroke were 0.98% and 0.93% respectively.14 While this represents an excellent outcome for this cohort of patients that is comparable to the literature, the low incidence of permanent stroke limits the extent of statistical analysis.
While most studies are retrospective cohort studies in current literature, there are ongoing randomized controlled trials (RCT) to investigate the outcomes of warfarin and NOAC in the cardiac postoperative setting. The NEW AF trial is a prospective, multi-centred RCT comparing rivaroxaban and warfarin with a primary outcome of postoperative length of stay.15 The largest RCT to date is the DANCE Trial, comparing the safety of NOAC and warfarin after cardiac surgery in the first 30 days postoperatively, with target completion in 2027.16 Further prospective studies will provide more refining insight into anticoagulation choice, safety, duration and outcomes. In recent years, there has been an increasing tendency towards a NOAC due to its lesser burden of monitoring for the patient. While the consensus in the literature remains unclear, it would be interesting to perform a survey of current practices and anticoagulation preferences.
This is the largest cohort study with long-term mortality analysis comparing warfarin and NOAC in POAF in Australia, to our knowledge. The main limitation of this study is its single-centre and retrospective nature, which can predispose to selection bias. However, a single institution also offers more control of external factors that may impact outcomes, such as the system and available resources. A major limitation of previous studies is the inconsistent definition of POAF, with over 12 different definitions and variable time frames.1 This study uses a clinically relevant definition that is consistent with the national ANZSCTS database, which allows comparison with other institutions and for more meaningful meta-analysis in the future. Previous cohort studies were limited by its strict inclusion criteria, with the majority of studies investigating CABG-only cohorts and therefore limiting the generalizability of the results to patients undergoing valve or other cardiac surgery.
Conclusions
With increasing use of NOAC and availability of reversal agents, there remains sparse evidence regarding its use in POAF. The use of a NOAC in patients with POAF did not appear to increase short-term postoperative complications, including bleeding, stroke, readmission rates and mortality, compared with warfarin. Warfarin and NOACs performed similarly in long-term all-cause mortality, suggesting NOACs as a plausible alternative to warfarin for anticoagulation in POAF. Consideration of patient-specific factors and preference remains essential in anticoagulation choice.
Ethical approval
This study has been approved with a waiver of consent by the Gold Coast University Hospital Human Research Ethics Committee (LNR/2022/QGC/90325).
Acknowledgement
Open access publishing facilitated by Griffith University, as part of the Wiley - Griffith University agreement via the Council of Australian University Librarians.
Author contributions
Shantel Chang: Conceptualization; data curation; investigation; methodology; project administration; writing – original draft; writing – review and editing. Alexander Lombardo: Data curation; project administration; writing – original draft. Ian Smith: Data curation; formal analysis; methodology; software; writing – review and editing. Samuel Lawler: Data curation; project administration. Cheng He: Conceptualization; resources; supervision; writing – review and editing. Andrie Stroebel: Conceptualization; resources; supervision; writing – review and editing.
Conflicts of interest
None declared.