25, 50 and 75 years ago
25 years ago
Cho CS, Buckingham JM, Pierce M, Hardman DT. Computed tomography in the diagnosis of equivocal appendicitis ANZ J. Surg. 1999;69:664–667
The clinically obscure right iliac fossa (RIF) pain remains a diagnostic problem. The present study examines the use of computed tomography (CT) in improving the accuracy of clinical assessment in these difficult surgical cases. The trial design was a retrospective review of all patients admitted under one surgeon with suspected acute appendicitis, between 1 January 1995 and 30 June 1997. The study setting was a district hospital (Calvary Hospital) that received patients from both an urban and rural environment. The patient cohort was identified from the Unit Registry and an International Classification of Diseases-based review of medical records. Twenty-one prospective data points were obtained from patient records. Those patients admitted with RIF pain and equivocal symptoms and signs subsequently underwent a CT and/or ultrasound (US) examination, conducted by the attending radiologist. For those patients who proceeded to appendicectomy, the histopathological findings were correlated with the imaging report. Those patients who were discharged after imaging without proceeding to operation were not readmitted to any regional hospital during the course of the study. A total of 84 patients were identified. Thirty-three patients (39%) underwent appendicectomy without imaging and were excluded from further analysis. A total of 51 patients (61%) underwent 61 imaging procedures. The CT scan was correct in 35/36 patients (97%), while US was correct in 17/25 patients (68%). The present study suggests that CT can be used to improve the accuracy of diagnosis of obscure RIF pain. As a pilot study, it supports the development of a randomized controlled trial in a multicentre regional study.
Hughes TMD. The diagnosis of gastrointestinal tract injuries resulting from blunt trauma ANZ J. Surg. 1999;69:770–777
This review studies the efficacy of the methods of assessment of the abdomen in blunt trauma for the detection of gastro-intestinal tract injuries (GITI). MEDLINE searches of English language publications on the subjects of diagnostic peritoneal lavage, abdominal computed tomography (CT) in blunt trauma and gastrointestinal tract injuries between 1980 and 1998 were used to identify relevant material. Earlier publications were identified from reference lists. The methodology, data and conclusions of all studies were examined in detail. The contemporary roles of clinical assessment, diagnostic peritoneal lavage, CT and other diagnostic modalities in detection of significant GITI were determined based on the best available evidence. The most accurate and safest methods of assessment of the abdomen in haemodynamically unstable patients with suspected abdominal injuries following blunt trauma are immediate laparotomy or diagnostic peritoneal lavage (DPL). The goal of assessment of the abdomen in stable patients is to accurately define the site and extent of intra-abdominal injury, in order that further management may be tailored to the specific injuries. The most recent evidence suggests that CT of the abdomen fulfils these criteria better than the other modalities of assessment available. The risk of overlooking a significant GITI on CT scan is minimal provided that unexplained free fluid, bowel wall thickening or enhancement, mesenteric fat streaking and bowel dilatation are taken as evidence of GITI. When scan quality is suboptimal or expert interpretation is unavailable, DPL is recommended. Fully cooperative patients with negligible abdominal signs can be safely observed clinically.
50 years ago
Moss DI. Adenocarcinoma of the vermiform appendix. ANZ J. Surg. 1974;44:140–142
Adenocarcinoma of the appendix commonly presents as appendicitis and in many instances is not recognized macrosropically by either the surgeon or the pathologist. It was seen in 0.3% of 3989 appendicectomy specimens. Thirteen such cases are reviewed. The age incidence is over 40 years in 90% of cases. Most patients present with appendicitis, and the condition is not detected macroscopically. Improved prognosis has been shown to follow right hemicolectomy in preference to simple appendicectomy (which may suffice in the presence of non-invasive carcinoma-in-situ). Histological section of all appendices removed from patients in the susceptible age-group is therefore mandatory.
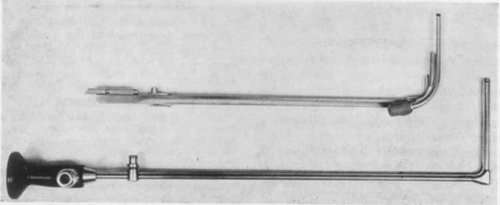
Leslie DR. Endoscopy of the bile duct: an evaluation. ANZ J. Surg. 1974;44:340–342
Both cholangiography and choledochoscopy have a place in biliary surgery. Operative cholangiography is of value in defining the need to explore the bile duct in any individual patient. Choledochoscopy has much more to offer and can practically eliminate the problem of the residual stone. It has, through technical advances, now reached the stage where it is safe, rapid and easy. The most satisfactory instrument by far has proved to be the present Storz instrument. This is a rigid right-angled instrument, with the objective end of a length of either 7 cm or 5 cm and an external measurement of 5 cm × 3 cm (Fig. 1). The 7-cm model is by far the better, as the 5-cm model cannot always reach the duodenum. It has fibre-optic illumination. It uses the revolutionary Hopkins rod-lens system, with excellent resolution, brilliant light transmission, extreme depth of field (contact to infinity), and a wide viewing angle of 90′. As with other choledochoscopes, an irrigating channel is provided. It should be used as a routine as a ‘postscript’ to conventional duct exploration, helping to avoid the problem of leaving residual stones.
75 years ago
Ross D. Segmental pulmonary resection. ANZ J. Surg. 1949;18:218–223
My purpose is to record experience confirming the practicability in many cases of limiting the amount of pulmonary tissue resected to units smaller than the five major lobes. This is obviously an advantage, particularly in such conditions as bilateral bronchiectasis, in which the patient needs any good lung tissue he has on his tree. It so happens also that the methods devised for this purpose may be used to facilitate lobectomy itself where the limits of the lobe are obscured or absent on account of failure of the normal fissures to develop, or their later obliteration by adhesions. The recognition of anatomical and functional broncho-pulmonary segments within the five larger lobes has proceeded steadily since bronchoscopy and thoracic surgery have been practised freely. The detailed anatomical work relating to the divisions of the pulmonary artery and vein, and to the external appearances of the bronchi in their respective hila came later. On a basis of six cases segmental pulmonary resection is found to be eminently practicable at least as far as the middle lobe, lingula, apical or first dorsal and lower basal segments go. Convalescence on the whole has been good to excellent. In three of the cases post-operative bronchograms show healthy bronchi in the portions conserved, but no late results are available. The principle of securing bronchus and vessels and then peeling the segment off through an avascular plane has also been applied with success in lobectomy in cases with poor or absent fissures.