How to perform duodenojejunostomy in addition to Roux-en-Y reconstruction following total gastrectomy to facilitate future duodenal surveillance
Graphical Abstract
Following total gastrectomy, reconstruction is required to restore gastrointestinal continuity. Roux-en-Y reconstruction is a commonly utilized technique following total gastrectomy,1 with acceptable weight regain and low rates of reflux oesophagitis reported in the post-operative setting.2
Roux-en-Y reconstruction following gastrectomy is problematic in the clinical scenario where duodenal surveillance is necessary. For example, regular endoscopic duodenal surveillance is indicated in familial adenomatous polyposis (FAP) syndrome,3 or in a situation where endoscopic resection of a duodenal adenoma requires surveillance but is made difficult due to gastric resection for cancer. In such cases, procedures such as double balloon enteroscopy are necessary to access the duodenum. Such procedures are time-consuming and require access to advanced endoscopic skillsets not available at all centres, and success rates for reaching the target site following Roux-en-Y reconstruction have been reported to be around 71%.4
We describe a novel technique of reconstruction following total gastrectomy: a proximal duodenojejunostomy as an additional step to the classical Roux-en-Y as a means of providing endoscopic access to the duodenum in clinical situations that demand future duodenal surveillance.
Total gastrectomy is performed with or without lymphadenectomy depending on the pathology. In cases involving gastric malignancy, radical control of gastric and gastroepiploic vascular pedicles is warranted, as is lymphadenectomy in keeping with the Japanese Gastric Cancer treatment guidelines.5 After application of a pursestring suture to the distal oesophagus, the distal oesophagus is transected. Six simple interrupted stay sutures with 3/0 prolene are evenly placed circumferentially along the transected distal oesophagus, intended to splay out the mucosa such that the anvil of the circular stapler can be placed in the distal oesophagus. The pursestring applicator is applied around the anvil of the stapler.
Next, Roux-en-Y reconstruction is performed by transection of the jejunum 30–40 cm distal to the ligament of Treitz with a linear stapler (Aeon™, Lexington Medical Inc., Bedford, MA, USA). The distal (alimentary) Roux limb is advanced in retrocolic fashion to the oesophageal stump, where oesophagojejunostomy is performed using a circular stapler (ECS25B or ECS29B, Ethicon™, Cincinnati, OH, USA). The staple line of the alimentary jejunal limb is excised, and the circular stapler enters the jejunal lumen. The pin is advanced through the jejunal wall to facilitate an end-to-side stapled oesophagojejunostomy. The circular stapler is removed, anastomotic donuts inspected, and a linear stapler is used to close the stump of the alimentary jejunum that had previously admitted the circular stapler.
The biliopancreatic limb is anastomosed to the alimentary limb 60–70 cm distal to the oesophagojejunostomy in the infracolic compartment. This jejunojejunostomy is performed using a linear stapler to form the anastomosis, and the resultant common defect is closed in two layers with 4/0 PDS.
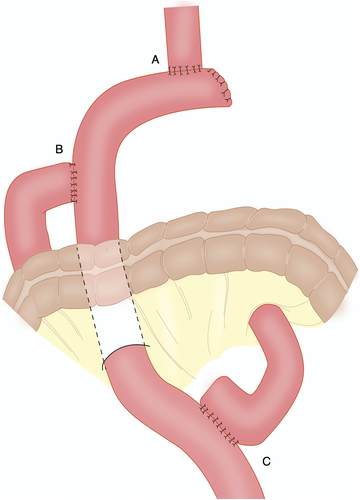
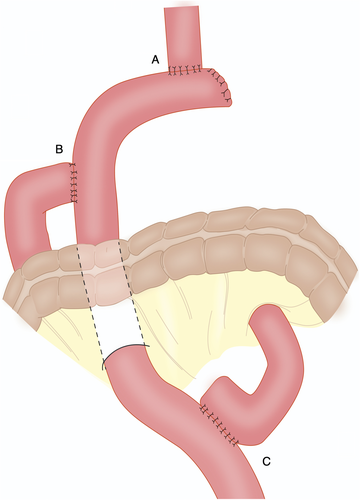
Finally, end-to-side duodenojejunostomy is performed by anastomosing the transected duodenal stump to the side of the alimentary limb, around 20 cm from the oesophagojejunostomy. This anastomosis is hand-sewn in two-layers with 4/0 PDS. Final configuration is demonstrated in Figure 1. Feeding jejunostomy is routinely placed 30 cm distal to the jejunojejunostomy in the left abdomen in Witzel fashion.
We describe a technique involving the addition of a proximal duodenojejunostomy following total gastrectomy and Roux-en-Y reconstruction in clinical situations that requires future endoscopic surveillance of the duodenum. We describe two such cases, elaborated upon further in the Online Supplementary version of this manuscript, where proximal duodenojejunostomy was performed as described. Neither patient had post-operative complications or complaints of bile reflux or other functional symptoms at follow-up. Postoperative endoscopic surveillance was easily permitted through a widely patent duodenojejunostomy. In clinical situations that necessitate future endoscopic duodenal surveillance, we would suggest that an additional proximal duodenojejunostomy is a feasible and safe technique.
Acknowledgement
Open access publishing facilitated by The University of Sydney, as part of the Wiley - The University of Sydney agreement via the Council of Australian University Librarians.