Etiology, risk factors, and prognosis of patients with syncope: A single-center analysis
Tingting Feng and Xiaofeng Xue are co-first authors.
Funding information
The present study was supported by Chinese Foundation for Hepatitis Prevention and Control (TQGB20190079)
Abstract
Objective
To investigate the main causes, risk factors, and prognosis of patients hospitalized with syncope.
Methods
The patients admitted due to syncope were included. We analyzed the etiology, risk factors, and prognosis of patients with an average follow-up of 15.3 months.
Results
High-risk factors for cardiogenic syncope included age ≥60, male, hypertension, palpitation, troponin T-positive, abnormal ECG, CHD history, and syncope-related trauma. Mortality rate was 4.6%, recurrence rate of syncope was 10.5%, and the rehospitalization rate was 8.5%. Univariate analysis showed that prognosis of syncope was related to age ≥60 years old, hypertension, positive troponin T, abnormal electrocardiogram, and coronary heart disease (p < .05). Multivariate Cox proportional hazard analysis showed that age ≥60 years old (p = .021) and high-sensitivity troponin-positive (p = .024) were strongly related to the prognosis of syncope. Kaplan–Meier curve showed statistical difference in the survival rate between the groups divided by age ≥60 years (p = .028), hs-TnT-positive (p < .001), abnormal ECG (p = .027), and history of CHD (p = .020).
Conclusion
High-risk factors for cardiogenic syncope included age ≥60, male, hypertension, palpitation, troponin T-positive, abnormal ECG, CHD family history, and syncope-related trauma. Age, hypertension, troponin T-positive, abnormal ECG, and CHD history were associated with the prognosis of syncope.
1 INTRODUCTION
Syncope is a sudden, transient loss of consciousness caused by various reasons. Due to a transient hypoperfusion of the brain, the patient appears to be unable to maintain posture tension (Goldberger et al., 2019). Syncope often has a sudden onset without obvious incentives, which has a short duration and recovers quickly. There are some characteristics of syncope, including a wide range of patients' ages, poor reproducibility of symptoms, and variable induced conditions. These characteristics bring difficulty to the diagnosis of clinical syncope and the identification of high-risk patients (Smyth et al., 2020). Some causes of syncope are high risk, such as cardiogenic syncope, which need to be treated as soon as possible (Brignole et al., 2018).
Syncope has many causes and clinical presentations; the incidence depends on the population being evaluated. Studies of syncope report prevalence rates as high as 41%, with recurrent syncope occurring in 13.5% (Lamb et al., 1960). Predictors of recurrent syncope in older adults are aortic stenosis, impaired renal function, atrioventricular (AV) or left bundle-branch block, male sex, chronic obstructive pulmonary disorder, heart failure (HF), atrial fibrillation (AF), advancing age, and orthostatic medications (Ruwald et al., 2012), with a sharp increase in incidence after 70 years of age (Soteriades et al., 2002). Reflex syncope was most common (21%), followed by cardiac syncope (9%) and orthostatic hypotension (OH) (9%), with the cause of syncope unknown in 37% (Soteriades et al., 2002). However, interpretation of the symptoms varies among the patients, observers, and healthcare providers. The evaluation is further obscured by inaccuracy of data collection and by improper diagnosis.
The current study focused on patients admitted to hospital due to syncope and investigated the main causes, risk factors, and prognosis of patients hospitalized with syncope.
2 METHODS
2.1 Patients
Patients who were hospitalized due to syncope or near syncope in the cardiology department of our hospital from January 2018 to December 2018 were selected. Inclusion criteria were patients with complete medical history collection and syncope or near syncope within 6 months before admission. Patients who cannot cooperate to complete the screening of the cause of syncope were excluded. The diagnosis of syncope was according to Guidelines for the diagnosis and management of syncope (Moya et al., 2009).
2.2 Data collection
The patients' syncope-related symptoms, gender, age, clinical complications, personal history, family history, etc. were recorded. The results of blood test, blood pressure, and routine electrocardiogram within 24 h after admission were recorded. Other examinations including 24-h ECG, continuous ECG monitoring, echocardiography, cranial CT/MRI, TCD, upright tilt test, carotid ultrasound, coronary CTA, chest CT, etc. were also performed and recorded. Cardiac electrophysiological examination and coronary angiography would also be performed if necessary. The etiology of syncope in hospitalized patients and high-risk factors in patients with cardiogenic syncope were analyzed.
2.3 Follow-up
All patients were followed up after discharge from the hospital by telephone. Follow-up end points included all-cause death, relapsed syncope, and rehospitalization, and we analyzed the prognosis of patients with syncope. The primary endpoint was all-cause death.
2.4 Statistical analysis
SPSS 22.0 software was used for statistical analysis. Measurement data were expressed as mean ± standard deviation (x ± s). Comparison of means between groups was performed using independent t-test. Count data were expressed by rate, and comparison of rates was expressed by chi-square test. p < .05 was considered as significant statistically different. Univariate analysis and multivariate Cox proportional hazard model were used to analyze the variables related to the prognosis of syncope. Kaplan–Meier curve was performed for variables identified by multivariate Cox analysis.
3 RESULTS
3.1 Basic characteristics
A total of 155 patients who were hospitalized due to syncope or near syncope in the cardiology department of our hospital from January 2018 to December 2018 were included. The basic characteristics of 155 patients with syncope are shown in Table 1. There were 84 males and 71 females. The average age was 62.6 ± 16.4 years old.
| Index | Number/Ration |
|---|---|
| N | 155 |
| Male (%) | 84 (54%) |
| Age (years) | 62.6 ± 16.4 |
| Hypertension (%) | 47.7% |
| Diabetes (%) | 18.1% |
| Hyperlipidemia (%) | 7.7% |
| Carotid plaque (%) | 18.7% |
| Hemoglobin (g/L) | 135.35 ± 12.85 |
| Triglyceride (mmol/L) | 2.58 ± 0.52 |
| Total cholesterol (mmol/L) | 4.82 ± 0.91 |
| Creatinine (µmol/L) | 69.26 ± 14.26 |
| Alanine aminotransferase (U/L) | 35.62 ± 10.26 |
| Hs-Troponin T (µg/L) | 32.99 ± 12.25 |
| NT-ProBNP (pg/ml) | 256.42 ± 63.72 |
| Echocardiogram ejection fraction (%) | 59.53 ± 13.45 |
3.2 Etiology of syncope
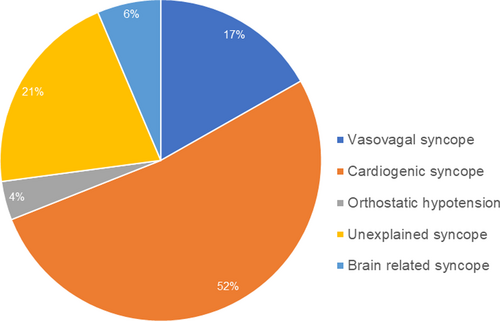
The cause of syncope has been found in 123 patients of all patients, with a diagnosis rate of 79.3%. Twenty-six (16.8%) patients were considered as vasovagal syncope, 81 (52.2%) patients were diagnosed with cardiogenic syncope, 6 (3.9%) patients were diagnosed with orthostatic hypotension, 10 (6.4%) patients were diagnosed with brain-related syncope, while 32 (20.7%) were considered as unexplained syncope (Figure 1).
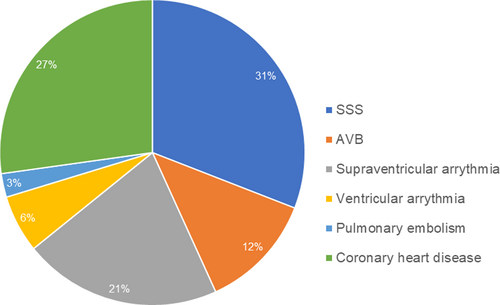
In cardiogenic-related syncope, 35 patients were diagnosed with bradycardia, including 25 (30.9%) patients of sick sinus syndrome (SSS) and 10 (12.3%) patients with atrioventricular block (AVB). Thirty-three patients received permanent pacemaker implantation. Twenty-two patients were diagnosed with tachycardia, including 17 (21%) patients of supraventricular arrhythmia and 5 (6.1%) cases of ventricular arrhythmia. Of all the tachycardia patients, six patients received radiofrequency ablation and five patients received event monitor implantation. There were two patients (2.5%) with pulmonary embolism and 22 patients (27.2%) with coronary heart disease. The causes of cardiac syncope are shown in Figure 2.
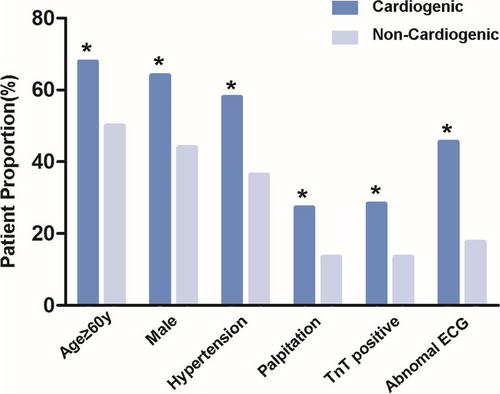
3.3 High risk of cardiogenic syncope
Age ≥60 years, male gender, hypertension, palpitations before syncope, high-sensitive troponin T-positive, abnormal electrocardiogram, positive family history, and trauma caused by syncope were high-risk factors of cardiogenic syncope (p < .05 vs. non-cardiogenic syncope) (Figure 3). Diabetes, hyperlipidemia, carotid plaque, increased NT-proBNP, decreased ejection fraction, liver, and kidney dysfunction showed no significant differences between the patients of cardiogenic syncope and the patients of non-cardiogenic syncope (p > .05).
3.4 Follow-up
All patients were followed up for an average of 15.3 months. Three cases were lost to follow-up. The main follow-up endpoints included all-cause mortality, relapsed syncope, and rehospitalization. There were seven deaths, with a mortality rate of 4.6%. Syncope of sixteen patients recurred, and the recurrence rate was 10.5%. Thirteen patients were re-hospitalized, and the rehospitalization rate was 8.5%. Univariate analysis showed that the death prognosis of syncope was related to age ≥60 years, hypertension, positive hs-TnT, abnormal electrocardiogram, and CHD (p < .05) (Table 2).
| Groups | Number | Survive | Deaths | X2 | p value |
|---|---|---|---|---|---|
| Age ≥60 years | 92 | 86 | 7 | 4.655 | .029* |
| Gender (male) | 83 | 78 | 5 | 0.838 | .36 |
| Hypertension | 71 | 65 | 6 | 4.485 | .034* |
| diabetes | 27 | 26 | 1 | 0.061 | .8 |
| Hyperlipidemia | 12 | 12 | 0 | 0.629 | .428 |
| Carotid plaque | 28 | 28 | 0 | 1.657 | .198 |
| Premonitory symptoms | 72 | 70 | 2 | 1.040 | .308 |
| Palpitations | 30 | 29 | 1 | 0.139 | .711 |
| Trauma | 55 | 53 | 2 | 0.184 | .668 |
| hs-TnT-positive | 33 | 29 | 4 | 5.42 | .02* |
| Family history | 28 | 26 | 2 | 0.503 | .478 |
| Abnormal ECG | 50 | 45 | 5 | 4.936 | .026* |
| Cardiogenic syncope | 78 | 72 | 6 | 3.475 | .062 |
| CHD | 22 | 19 | 3 | 4.776 | .029* |
- * p < .05.
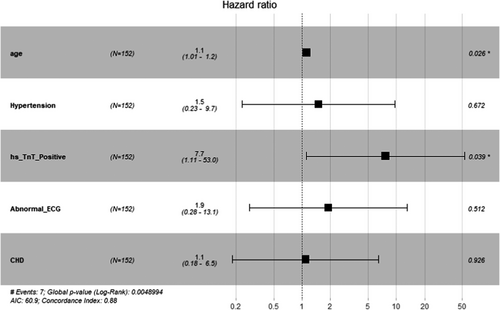
Multivariate Cox proportional hazard model was used to analyze the variables related to the prognosis of syncope. The variables were incorporated into the model by step-by-step method. Taking death as the dependent variable and age ≥60 years old, hypertension, high-sensitivity troponin-positive, abnormal ECG, and history of coronary heart disease as the independent variables, the results of multivariate Cox proportional hazard analysis showed that age ≥60 years old (p = .021) and high-sensitivity troponin-positive (p = .024) were the influencing factors related to the prognosis of syncope death (Figure 4).
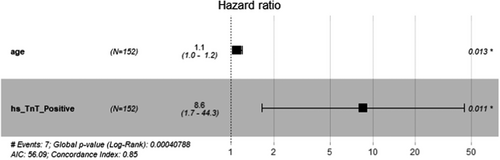
Further Cox risk proportional analysis model including age ≥60 years and high-sensitivity troponin-positive as the independent variable and death as the dependent variable showed that the two factors were still strong influencing factors related to the prognosis of syncope, with a respective p value of .013 and .011 (Figure 5).
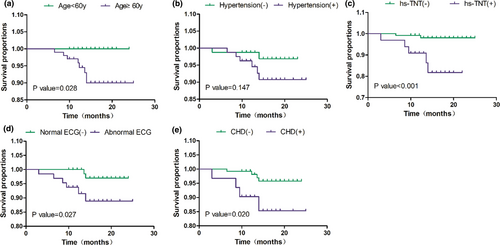
Average follow-up period was 15.3 months. Kaplan–Meier curve was performed for variables identified by multivariate Cox analysis, including age ≥60 years, hypertension, hs-TNT (+), abnormal ECG, and history of CHD. Results showed that there was statistical difference in the survival rate between the groups divided by age ≥60 years (p = .028), hs-TNT-positive (p < .001), abnormal ECG (p = .027), and history of CHD (p = .020) (Figure 6; Table 3).
4 DISCUSSION
Syncope is a transient cerebral hypoperfusion caused by a variety of diseases, usually manifested as a sudden onset of reversible transient loss of consciousness (Brignole et al., 2018; Goldberger et al., 2019; Smyth et al., 2020). The diagnosis of syncope is difficult due to the poor reproducibility of symptoms, which brings certain difficulties to the risk assessment of patients with clinical syncope. The European Society of Cardiology proposed a method for assessing syncope, including carotid sinus massage, upright tilt test, autonomic nerve function test, ECG monitoring, video recording of suspected syncope, electrophysiological examination, endogenous adenosine assessment, echocardiography, exercise stress test, and coronary angiography (Anderson et al., 2016; Barón-Esquivias et al., 2020; Kapoor & Hanusa, 1996; Varosy et al., 2017; Yoshimoto et al., 2020). It aims to improve the diagnostic decision level of clinical syncope, reduce missed diagnosis and misdiagnosis, identify high-risk patients in time and deal with them, and reduce the consequences of life-threatening situation. Current study has analyzed the patients hospitalized for syncope, determined the cause of syncope, and analyzed the relevant clinical features and prognosis.
Totally 155 patients were enrolled in this study. The age of onset of syncope was wide, and the age distribution was 27–88 years old, with an average age of 62 years. Hypertension, diabetes, hyperlipidemia, and carotid plaques were the most common comorbidities. Among the causes of syncope, neuro-mediated syncope accounted for 16.8%, while cardiogenic syncope accounted for 52.2%. Cardiac syncope was still one of the main causes of hospitalized patients with syncope. The cardiogenic syncope was mainly caused by arrhythmia and coronary heart disease, and timely treatment of such patients, including pacemaker implantation, radiofrequency ablation, cardiac event recorder implantation, coronary angiography, or stent implantation, was expected to reduce the recurrence of such cardiogenic high-risk syncope.
Risk factors for cardiogenic syncope included age ≥60, male, hypertension, palpitation, troponin T-positive, abnormal ECG, heart family history, and syncope-related trauma. 20.7% of patients with unidentified causes of syncope were followed up. Patients with syncope have a risk of recurrence and need to be closely followed up. Monitoring of rhythm and blood pressure, timely checking immediate ECG, dynamic electrocardiogram, etc. were reported to reduce the risk of syncope (Ng et al., 2019; Probst et al., 2020; Roca-Luque et al., 2019; Russo et al., 2018; Thiruganasambandamoorthy et al., 2020). Univariate analysis showed that the prognosis of syncope was related to age ≥60 years old, hypertension, positive troponin T, abnormal electrocardiogram, and coronary heart disease. Sun et al. (Sun et al., 2009) assessed the occurrence of a pre-defined serious event within 30 days after an ED evaluation for syncope or near syncope. In a cohort including 2584 patients, 173 patients (7%) with an age ≥60 experienced a 30-day serious event. High-risk predictors included age greater than 90 years, male gender, history of an arrhythmia, triage systolic blood pressure greater than 160 mmHg, abnormal electrocardiogram, and abnormal troponin I level.
Multivariate analysis showed that age ≥60 years and positive troponin T were independently correlated with the prognosis of syncope death. Advanced age is associated with increased susceptibility to syncope due to impairments of heart rate and blood pressure regulation and increased incidence of cardiac arrhythmias (Galizia et al., 2009; McIntosh et al., 1993). In addition, cerebral auto-regulation is impaired with aging particularly in the presence of hypertension rendering moderate declines in blood pressure of any cause symptomatic (Lipsitz, 1989). Although several studies have questioned the routine ordering of cardiac enzymes (Grossman et al., 2003; Link et al., 2001), we found that an abnormal troponin I level was associated with serious outcomes.
In conclusion, current study summarizes the clinical features, high-risk factors, and prognosis-related factors of patients with clinical syncope in our center. Our aim is to provide some data support for the diagnosis and treatment of clinical syncope patients.
CONFLICT OF INTEREST
None.
AUTHOR CONTRIBUTION
Guarantor of integrity of the entire study: LL; Study concepts: LL, TF; Study design: LL, TF; Definition of intellectual content: XX; Literature research: ZL; Clinical studies: LL, TF; Experimental studies: XX; Data acquisition: LL, XX; Data analysis: LL, ZL; Statistical analysis: LL, TF; Manuscript preparation: LL, TF, XX; Manuscript editing: LL; Manuscript review: ZL, LM.
ETHICAL APPROVAL
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study is approved by the Ethics Committee of First Affiliated Hospital of Suzhou University. Written informed consent was obtained.
CONSENT FOR PUBLICATION
Informed consent was obtained from all individual participants included in the study.
Open Research
DATA AVAILABILITY STATEMENT
The datasets used or analyzed during the current study are available from the corresponding author on reasonable request.