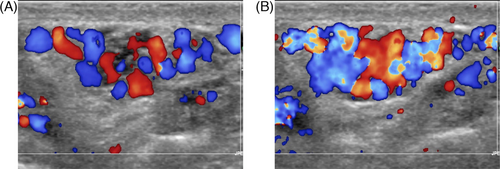
Role of multiparametric ultrasound in testicular focal lesions and diffuse pathology evaluation, with particular regard to elastography: Review of literature
Abstract
Background
Ultrasound is the main requested technique for the assessment of traumatic, vascular, neoplastic, and inflammatory testicular pathology. Moreover, the role of ultrasound has broadened over the years along with the introduction of new techniques, such as contrast enhanced ultrasound and ultrasound elastography.
Objective
An updated representation of the pre-existing Literature evidence for multiparametric ultrasound imaging with particular regard to elastography, in the evaluation of focal and diffuse testicular pathologies, has been presented.
Methods
The search was performed in PubMed, Cochrane, EMBASE, Web of Science and Scopus databases from the earliest available article (1977) until January 2021. Based on the evidence of the Literature, the current role of US imaging for focal and diffuse testicular pathologies has been reported and illustrated, with emphasis on examination technique, classification, and pitfalls. Results: Multiparametric Ultrasound has a recognized role for testicle focal and diffuse disease. Elastography is nowadays recognized as an essential part of the multiparametric ultrasound examination. However, in the setting of testicular pathology this method showed some promising results in the setting of varicocoele and for focal lesions characterization. In the remaining field its role is still under debate.
Discussion
B-mode ultrasound and color Doppler ultrasound have been for a long time the diagnostic gold standard for testicular pathologies. The introduction of both contrast enhanced ultrasound and elastography in the last two decades has brought to the emergence of the multiparametric ultrasound concept. These methods are currently able to increase diagnostic confidence especially for testicular lesions characterization, with different relevance depending on the pathology under consideration.
Conclusion
Multiparametric ultrasound testis assessment, with specific regard to elastography is nowadays recommended for focal and diffuse disease evaluation. Further and larger studies are however needed to validate these results and to understand if the role of elastography in testicular pathology may be broadened.
1 BACKGROUND
1.1 Ultrasonographic techniques
Ultrasound is the main and primarily used technique in the assessment of testicular pathology. Its use has proven to be pivotal in case of traumatic, vascular, neoplastic, and inflammatory diseases. Moreover, the role of ultrasound has broadened over the years along with the emergence of new techniques such as contrast-enhanced ultrasound (CEUS) and elastography; hence, it is correct to talk about all these methods as multiparametric ultrasound examination.1
The introduction of second-generation contrast agents in CEUS allowed ultrasound to better assess vascular features, such as microvascular architecture, and contrast enhancement patterns of lesions. The display of different behaviors of nodules after contrast-agent injection is similar to what is observed in contrast-enhanced computed tomography (CT) and contrast-enhanced magnetic resonance (MRI), with two important differences. The first one is that during CEUS, the contrast enhancement pattern through the different phases can be witnessed in real time, rather than at certain pre-selected temporal intermissions. The second difference is that ultrasound contrast media are “blood pool agents,” which means that microbubbles are retained in the vascular space without any enhancement of the extracellular spaces.2, 3
Elastography is a technique aimed at evaluating the stiffness of a tissue quantifying its deformation or measuring the speed of propagation of shear waves when a force is applied. This differentiation is the key factor in the classification of the different elastography methods, which fall under two categories: strain elastography (SE) and shear wave elastography (SWE).4, 5
SE is based on display and calculation of tissue displacement; this alteration may be produced through active external pressure with the ultrasound transducer or exploiting physiological internal tissue motion (both these methods fall under the quasi static elastography category) or it may be induced by an ultrasound focused radiation force impulse (ARFI, which falls under the dynamic elastography category).4, 5
In SWE, an acoustic pulse is used to cause displacement on a target tissue; however, this technique does not aim to measure the strain but rather the speed of propagation of the shear waves produced by the acoustic pulse. These waves propagate in a cone-shaped area around the target of the acoustic pulse; their speed depends on tissue stiffness and can be measured (m/s) and converted in kilopascal using the Young's module. All shear wave techniques fall under the dynamic elastography category.4-6
The aim of the present review is to show the diagnostic performance of multiparametric ultrasound, with particular regard to elastography, in the evaluation of focal and diffuse testicular pathologies.
1.2 Testicular neoplasms
The World Health Organization classifies testicular neoplasms in several groups, among them germ cell tumors (GCT) represent the most common one and is further divided into seminoma and non-seminomatous germ cell tumors (NSGCT), including embryonal cell carcinoma, choriocarcinoma, yolk sac tumor, teratoma, and mixed germ cell tumor neoplasm of the testicle. Another clinically and epidemiologically relevant entity is the Leydig cell tumor, which falls in the sex cord-stromal tumor group.7 Testicular neoplasms have an incidence of three to six cases per 100,000 males per year in Western countries, 95% of which are primitive testicular tumors, with a rising trend in the last 30 years.8, 9 Although counting for a small part of the total male population neoplastic pathology (1%–1.5%), GCT actually are the most frequent neoplasm in the 15–40 years age group.9
Risk factors include ethnicity (with Caucasians being affected more than African Americans with a 9:1 ratio), previous tumor in contralateral testis, family history of GCT, cryptorchidism, Klinefelter syndrome, and immunosuppression (organ transplant, HIV infection). Survival rates are reported to be excellent in localized stage cases (95%–100%) and high in cases with mestastases (70%–90%).10, 11
2 METHOD
2.1 Literature search protocol and eligibility criteria
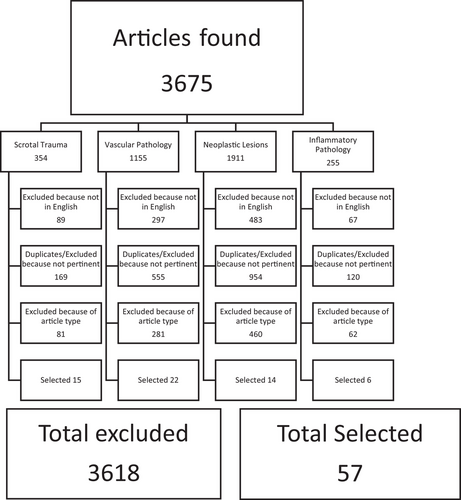
The search was performed by six operators (one radiologist and five radiology residents of our institution) in PubMed, Cochrane, EMBASE, Web of Science, and Scopus databases from the earliest available article (1977) until January 2021. Each method included in the multiparametric ultrasound examination and their variations, abbreviations, and subgroups (ultrasound, B-mode ultrasound, grayscale ultrasound, color-Doppler, CD, CDUS, contrast-enhanced ultrasound, CEUS, elastography, elastosonography, shear wave, SWE, strain elastography, SE) were singularly used followed by the term testicle and one term at a time from the following list of pathologies: tumor, neoplasm, nodule, Leydig, leydigioma, germ cell tumor, seminoma, non-seminomatous germ cell tumors, orchitis, orchiepididymitis, varicocele, testicular torsion, trauma.
A list with the titles and abstracts of all acquired articles was created and were screened one by one for eligibility by a group of four operators (two radiologists and two radiology residents in our institution). Exclusion criteria were being letters to the editor, commentaries, posters, oral presentations, and/or being written in other languages than English. During this evaluation, duplicates and articles not meeting the focus of our study were also excluded (Diagram 1).
2.2 Multiparametric ultrasound examination protocol
Although slight diversities may exist among different institutions and authors on how to perform ultrasound examination of the scrotum, a series of common indications also supported by guidelines is reported below.
The patient is arranged in supine position with a support to stabilize his scrotum; he is asked to keep his penis stuck to the anterior abdominal wall and abundant ultrasound gel is used. The exam is performed with high-frequency linear probes (>10 MHz), although when the scrotum is markedly swollen a convex probe can also be used to obtain a more panoramic view.
Sagittal and axial scans are acquired and comparison with the unaffected testis is carried out about echostructure and volume. Vascularity is compared as well and color-Doppler module should be set with appropriate gain (no appearance of random color artifacts), low wall filter (<100 Hz), and low pulse repetition frequency (<4 cm/s).1, 12-14
SE assessment is performed by applying slight and regular pressure to the testis through the ultrasound probe. The intensity and rhythm of the manual compressions are usually adjusted with the aid of a real-time quality control system, which varies depending on the ultrasound equipment. B-mode and elastographic images are simultaneously displayed on the screen and the strain ratios between testicle and subcutaneous fat tissue or affected and unaffected testicle are calculated, using regions of interest (ROI) of the same dimension placed at similar depth.15, 16
SWE evaluation is performed by keeping a firm contact with the cutaneous plan without applying pressure, in order to avoid compression artifacts. A series of pulses is sent to the ROI, thus creating a colorimetric overlay on the B-mode image within the elastogram box, which on linear transducers has 2–3 cm side length. Data are usually presented as meters per second but, depending on the system, they can also be converted in kilopascal by means of Young's modulus.4
In order to perform CEUS examination a 20 gauge or larger cannula (to minimize microbubble disruption) is arranged on one forearm vein of the patient and a fast bolus of contrast medium is hand-injected, followed by 10 ml of saline flush. Ultrasound equipment setting includes low mechanical index (0.04–0.1). Above all if the first injection has been used to portray a focal lesion, usually a second bolus is carried out to perform a more panoramic evaluation and/or assess the contralateral testicle. The examination is digitally recorded to allow subsequent re-evaluation and to eventually perform a quantitative analysis (time/intensity curves).17
3 RESULTS
3.1 Scrotal trauma
Scrotal injury accounts for 1% trauma referred to emergency departments and most commonly occurs in under 30 years old median age patients as results of penetrating injuries or severe blunt trauma, which are sport related in 50% of cases. Clinical examination is usually able to uniquely detect scrotal swelling and pain and, given that urgent surgery is often necessary for testicular salvage, diagnostic imaging role becomes crucial. In this setting, CT and MRI are expensive, impractical, and often inconclusive or unavailable as well, and also because of the superficial localization of the scrotal structures, ultrasound modalities represent the diagnostic gold standard.8, 9, 14, 15
In the aftermath of testicular trauma, several situations may be present, including scrotal wall hematoma, hematocele, testicular hematoma, or testicular rupture.
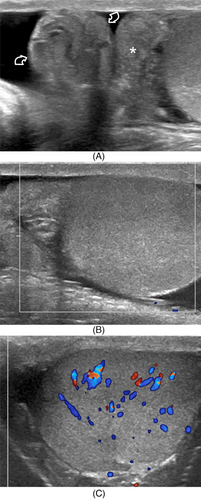
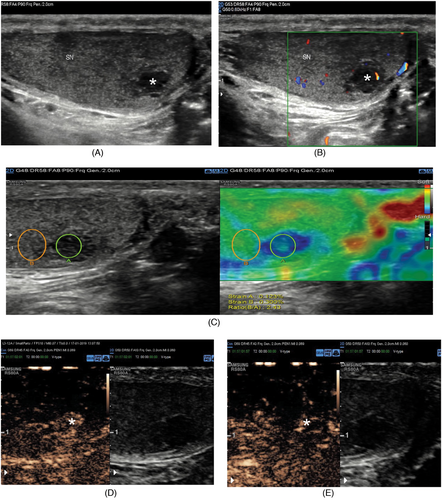
Scrotal and testicular hematoma usually present as a heterogeneous echo pattern area without inner vascularity and with well-defined borders within the scrotal wall and testis parenchyma, respectively.1, 16, 17 On CEUS, hematomas appear as sharply defined, non-enhancing areas, although some enhancing septations may be seen; perilesional parenchyma can be hypervascular.5,9 Follow-up imaging is indicated to document the evolution of the lesion, which in the majority of cases changes in shape, reduces in size, and eventually disappears or results in a residual scar17 (Figure 1). The ability of CEUS to precisely depict the hematoma grants a more accurate evaluation of the lesion size, allowing better decision-making in the patient management. In this setting, the absence of focal enhancement alterations on CEUS is sufficient. On the other hand, this method is able to detect high-sensitivity complications, such as areas of secondary ischemia (Figure 2).1, 16 The presence of inner contrast enhancement and the lack of progression toward resolution in subsequent follow-up examinations should raise the suspicion of an incidentally found neoplasm; in this circumstance SE may play a role in order to increase diagnostic confidence, as testicular tumors usually appear as “hard” lesions, while hematomas have lower strain ratio levels.18-20
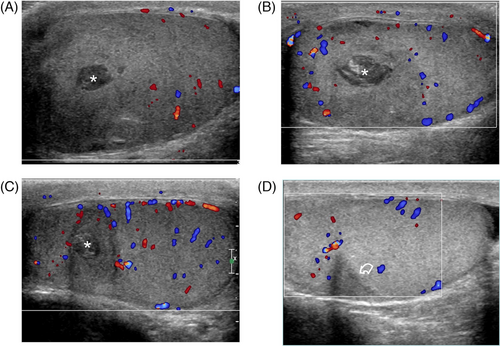
In the study by Lobianco et al., the relevance of data added by the use of CEUS was classified as high in four of 40 (10%) cases, moderate in nine of 40 (22.5%), low in 13/40 (32.5%), and none in the remaining 14/40 (35%).13
3.2 Vascular pathology
3.2.1 Varicocoele
Varicocoele is a pathology affecting 15% of the male population; this percentage can rise up to 19%–41% in males evaluated for infertility, even when the correlation between varicocoeles and infertility is still debated.21-26 It is defined as an abnormal dilatations of the pampiniform plexus with reflux of venous blood flow (>2–3 mm in diameter) caused by insufficiency or absence of valves; however, when diagnosed during adult age, it could be correlated to several conditions (hydronephrosis, hepatic cirrhosis, nutcracker syndrome27) including neoplastic mass compressing spermatic veins, so exams to rule out a secondary varicocoele should be performed (Figure 3). Varicocoele is in general asymptomatic, but may present with pain, enlarged scrotum, and infertility/subfertility, and a “bag of worms” appearance is often detected on palpation.28-31

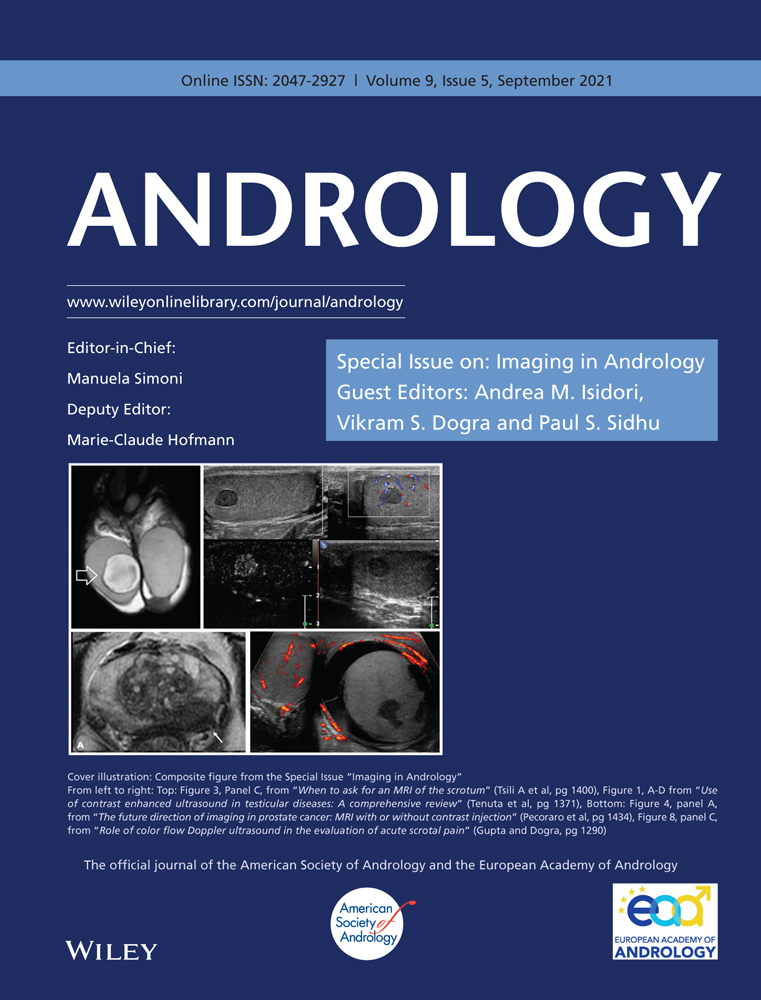
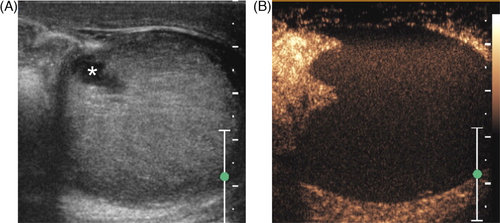
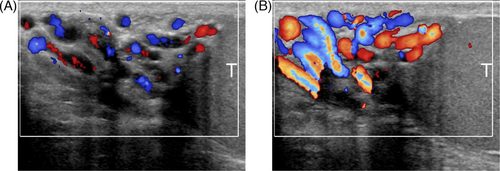
B-mode ultrasound is able to detect venous dilation with varicose appearance both within scrotum and along inguinal canal, while CDUS with spectral analysis allows to visualize vein flow and persistent reflux both in basal conditions and during Valsalva maneuver, in clinostatism, and in standing position, thus allowing grading of varicocoele, for which the Sarteschi classification is the most widely used system (Figures 4 and 5).21, 22, 32-36
In a study by Turna and Aybar, SWE was able to show that the stiffness of left testicle in patients affected with varicocoele was higher both in the group with normal sperm count (Group A, 4.77 ± 1.16 kPa) and in the group with oligospermia (Group B, 6.15 ± 1.96 kPa) in comparison with the healthy controls (3.79 ± 0.94 kPa) (p < 0.001). Moreover, mean SWE value of the left testes in group B (6.15 ± 1.96 kPa) was higher than group A (4.77 ± 1.16 kPa) (p = 0.002). No correlation was demonstrated between SWE values and the grade of varicocoele (r = 0.102, p = 0.423).37
Nevertheless, a statistical significance close to importance (p = 0.153) between SWE values and varicocoele grade was reported by Jedrzejewski et al. in patients with grade III pathology: 2.80 ± 0.72 kPa in affected testes versus 2.42 ± 0.85 kPa in contralateral healthy testes. Moreover, a statistically significant difference in stiffness between affected and unaffected testes was reported in patients with >20% testicles volume difference: 2.77 ± 0.75 kPa versus 2.37 ± 0.65 kPa (p < 0.05).38
In another study conducted by Fuschi et al., SWE values, along with testicular size and spermiogram, demonstrated a statistically significant positive correlation between the pre- and post-surgery assessments (p-value < 0.0001).39
The use of SE has found as well that testicles affected by varicocoele are stiffer than contralateral healthy ones or case controls.40, 41
Caretta et al. assessed with CEUS 90 patients affected by varicocoele and found that a mean transit time higher than 36 s was correlated with oligospermia, with 78% sensitivity and 58% specificity.42
3.2.2 Testicular torsion
Testicular torsion is a urological emergency caused by twisting of the spermatic cord, thus leading to vascular obstruction; in low-degree cases only venous drainage is involved and arterial vascularity can still be seen within testicular parenchyma, whereas in high-degree or complete torsion both venous and arterial flows are not visible. Because the chance of salvage of the testis is time related and testicular torsion may mimic orchiepididymitis at clinical examination, diagnostic imaging plays a crucial role in patient management.43
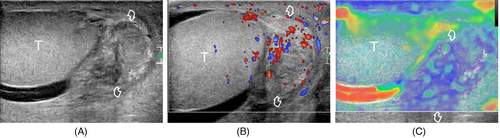
B-mode framework includes signs such as testis and epididymis enlargement, heterogeneous echotexture, and reactive hydrocele, which do not allow to clearly distinguish between inflammatory pathology and testicular torsion and/or spontaneously or intermittently detorted testis. Doppler findings however are more specific. In high-degree torsion, testis is avascular at color Doppler interrogation (Figure 6), whereas in low-degree torsion arterial flows may be present, but blood flow alterations are recorded, such as monophasic waveforms, post-stenotic flows, diastolic flow reversal, reduction of diastolic flow velocities with increase of resistive index. The ‘‘whirlpool sign,’’ which consists of a layered mass (twirling mass) above the affected testicle representing the coiled spermatic cord,44 is identified both in high-degree (without flow) and low-degree (with twirling vessels) torsion.
Although in cases of complete torsion, CDUS is usually sufficient to reach a diagnosis and CEUS does not add relevant information, it might play a role in cases of low-degree or intermittent torsion, even when identification of the twirling mass and of pathological testicular arterial waveforms are clue for diagnosis. In this setting, CEUS may facilitate the diagnostic process by showing a clear disequilibrium of enhancement between affected and healthy testicle, also because there is a minor need for equipment setting. On the other hand, a correct interpretation of CDUS may be more challenging, because a weak blood flow within testis parenchyma or in peritesticular tissue might be present.45, 46
Xue et al. have studied the diagnostic efficiency of SWE in the differential diagnosis of testicular torsion and acute orchiditis; they demonstrated higher stiffness within the twisted spermatic cord and testicular capsule in patients affected by testicular torsion, while no statistically significant difference was found in testicular parenchyma.47
Herek et al. demonstrated on an animal model statistically significant differences in SE colorimetric map patterns and strain ratio values in different degrees of testicular torsion at 8 and 24 h.48
3.3 Neoplastic lesions
CEUS applications in the setting of focal testicular lesion have been assessed in the last decades. As previously stated, this method has been shown to be useful in the differentiation between testicular hematoma or segmental infarction and neoplastic lesions (Figures 7 and 8).43 Moreover, some data have been gathered by different authors about the possibility of discriminating different types of neoplastic lesions with CEUS, in particular benign from malignant ones (Figure 9). These studies showed that using CEUS quantitative analysis with time–intensity curves and wash-in and wash-out curves may help in this task, as a rapid wash-in and a prolonged wash-out were observed in Leydig cell tumors in comparison with seminoma.49, 50
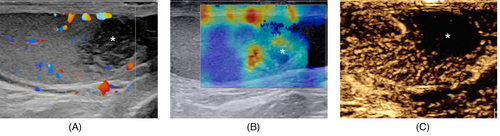
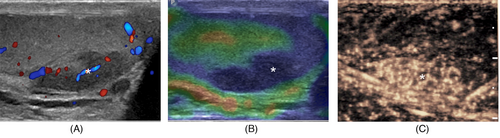
In 2020, Roy et al. used SWE to assess elastographic values of normal testicular parenchyma in comparison with various testicular diseases, such as tumors. They found that neoplasms presented a median stiffness value of 21.02 kPa with a 16.1 kPa cut-off, while normal testicular tissue had a median value of 4.55 ± 2.54 kPa and in fibrosis cases it reached a 30.03 kPa value with a cut-off of 26.3 kPa.50
In 2017, a similar evaluation had been carried out by Pedersen et al., who found in cases of testicular neoplastic lesions a mean velocity of 1.92 m/s (95% CI: 1.82–2.03), while a mean velocity of 0.76 m/s (95% CI: 0.75–0.78) was scored by the control group and a value of 0.79 m/s (95% CI: 0.77–0.81) was reached by patients affected by testicular microlithiasis.52 One year later, the same authors confirmed these results combining SWE with MRI diffusion weighted imaging (MRI-DWI). They observed that both MRI and DWI were not able to find a statistically significant difference between the healthy patients’ group and the one with microlithiasis, whereas the neoplastic lesions demonstrated significantly different values on both the techniques (healthy, microlithiasis, tumor; SWE: 0.77, 0.78, 1.95 m/s; DWI: 0.929 × 10−3, 0.978 × 10−3, 0.743 × 10−3 mm2/s).53
Trottmann et al. have used virtual touch tissue imaging quantification (VTIQ) in two different studies. They demonstrated a mean shear wave velocity of 1.94 m/s in GCT with a mean value of 2.42 m/s in seminoma, while benign lesions reached a value of 2.37 m/s.54 Marcon et al. also seem to suggest that VTIQ technique delivers higher mean values than SWE in healthy patients, possibly because of its smaller ROI: SWE 0.81 m/s, VTIQ 1.07 m/s.55
Another study conducted by Dikici et al. revealed a statistically significant difference in SWE value between normal testicular parenchyma (4.4 ± 3.9 kPa), seminomas (10.6 ± 3.9 kPa), and non-seminomatous germ cell tumors (47.0 ± 14.5 kPa).56
Other authors have assessed the diagnostic performance of SE. Among these there were Aigner et al., who found at qualitative SE analysis that all neoplasms in their patient population (n = 50) were detected as blue (hard) on the colorimetric map, along with three non-neoplastic lesions (one post-biopsy scar, one cyst, and one partial infarction), whereas the other non-neoplastic lesions were color-coded as soft. In their study, SE demonstrated a sensitivity of 100%, a specificity of 81%, a negative predictive value of 100%, a positive predictive value of 92%, and an accuracy of 94% in the diagnosis of testicular tumors.58
Pozza et al. assessed both SE qualitative and quantitative analyses. They used a 3-point elastographic scale, with grade 3 including grades 3, 4, and 5 of the 5-point scale by Itoh57; none of the 37 malignant lesions scored grade 1, while seven scored grade 2 and the remnant ones grade 3. At the quantitative assessment, malignant lesions showed higher strain ratio values than benign lesions (median 1.48 vs. 1.25), and overall neoplastic lesions demonstrated higher strain ratios than non-neoplastic ones (median 1.37 vs. 1.11); however, ROC curves analysis showed that qualitative assessment was superior than strain ratio values both in diagnosing neoplasms and in identifying non-neoplastic lesions.59
On the other hand, Konstantatou et al. reached different conclusions, as in their study a strong correlation between strain ratio and qualitative analysis was found but comparison of the ROC curves showed that strain ratio was superior in diagnosing malignancies, while there was no significant difference in identifying neoplastic lesions.60
SE performed well also in the study by Reginelli et al., although five malignant lesions in their patient population, all diagnosed as teratomas, showed a “soft” pattern; it has been supposed that this elastographic behavior could be connected to a high content of adipocytes in this kind of malignancies.61
Goddi et al.62 using SE found 87.5% sensitivity, 98.2% specificity, 93.3% positive predictive value, 96.4% negative predictive value, and 95.8% accuracy in the differential diagnosis between malignancies and benign lesions using the color-coded score by Itoh.
3.4 Inflammatory pathology
In case of inflammatory involvement of the testicle and epididymis, clinical examination can be challenging because of the non-specific nature of findings such as scrotal enlargement, erythema, and pain. B-mode imaging usually shows increased volume of epididymis (epididymitis) or of both testicle and epididymis (orchiepididymitis) with heterogenous echostructure, while CDUS and CEUS show an intensification of vascularity, although abscessual non-enhancing areas may be present (Figure 10), and the parenchymal edema could lead to venous compression and ischemic alterations.14
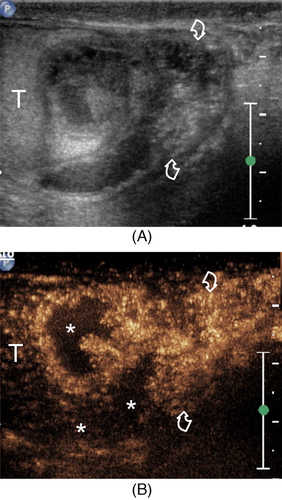
Elastographic evaluation of inflammatory pathology shows increased stiffness of involved parenchyma (Figure 11); in case of abscess, a focal soft area is usually detected, although a more heterogeneous appearance with small stiff regions may be present if there are phenomena of colliquation.44
Chen et al. assessed the use of SWE in evaluating stiffness of epididymal inflammatory tail masses and found significant changes of elasticity during several measurements between initial diagnosis and 2 weeks after therapy and remission.63
Roy et al. found in patients with acute orchitis slightly higher SWE values, although this difference was not statistically significant.51
4 DISCUSSION
B-mode ultrasound and CDUS have been for a long time the diagnostic gold standard for testicular pathologies. The introduction of both CEUS and elastography in the last two decades has led to the emergence of the multiparametric ultrasound concept. These methods are currently able to increase diagnostic confidence in several settings, with different relevance depending on the pathology under consideration.64
In case of testicular trauma, the first role of CEUS is to precisely establish the eventual rupture of the tunica albuginea and the amount of salvageable tissue. These accurate data delivered by CEUS are helpful in defining if surgery is needed; moreover the exam can be repeated, allowing rigorous management and follow up of the patient.1
Elastography is not currently reported to have a significant impact in the diagnostic process of scrotal trauma and the sole indication might be adding data in case of a suspect incidentally found neoplastic lesion.29
In patients affected by varicocoele both SWE and SE have demonstrated a statistically significant difference in stiffness between affected and unaffected testis, with some correlation between elastographic values and varicocoele grade.34-37 However, studies with larger patients’ populations are needed in order to validate and categorize these results.
In the differential diagnosis between inflammatory pathology and testicular torsion, higher SWE values have been found in the latter when assessing the spermatic cord and testicular capsule, while no significant difference was found in testicular parenchyma stiffness.47
In focal lesions several studies have constantly found that neoplasms demonstrate higher stiffness using both SWE and SE; a soft pattern was however detected in some cases. Pedersen et al. also discovered a correlation between SWE and MRI-DWI values, meaning that within stiff lesions a higher impediment to water molecules diffusion is present.53
Marcon et al. found that stiffness of focal testicular lesions is increased in comparison with normal parenchyma both at SWE and VTIQ, with the values of the latter being higher than the ones of the former, because of technical differences between the two methods.55
Some authors made further research trying to discriminate benign from malignant lesions using SE; they had good feedbacks although controversial. Indeed, malignant lesions showed higher scores in the Itoh scale at qualitative assessment and higher strain ratio values at the quantitative evaluation; however, ROC curves analysis showed qualitative SE being superior to strain ratio values in the paper by Pozza et al.,59 while in the study conducted by Konstantatou et al.60 quantitative analysis reached better results.
Currently, elastography does not show a relevant clinical application in inflammatory pathologies, as the studies performed so far did not find any significant result.51
There are some limitations to the use in daily clinical practice of the techniques included in multiparametric ultrasound. Among the main ones there is an increase in the time needed to perform the examination, which is even more important in emergency settings. Another limitation is the need for a higher number of staff members and the fact that they need to be properly trained. In the case of CEUS in particular, at least two operators are needed: one performing the scan and one doing the contrast medium injection. Training is particularly crucial in the case of SE, because this is a technique with high difference in interoperator reliability, and it requires to learn how to properly perform free-hand compression. Another limitation is the higher economic burden in comparison with the baseline ultrasound evaluation: besides the higher number of staff members required for multiparametric ultrasound, the cost of contrast medium and of both software and hardware to perform CEUS and elastography has to be taken into account. Finally, in the case of elastography there are significant discrepancies among the results of different brand of equipments and standardization is thus difficult.3, 4
5 CONCLUSION
Elastography is nowadays recognized as an essential part of the multiparametric ultrasound examination. However, in the setting of testicular pathology this method showed some promising results only in two fields. One is varicocoele, where differences between affected and unaffected testicles were found, along with some correlation between elastographic values and varicocoele grade. The second is focal lesions, as several studies found that this technique may have a role in differentiating focal non-neoplastic lesions (such as abscesses) from tumors and even in discriminating benign from malignant neoplasms.
Further and larger studies are however needed to validate these results and to understand if the role of elastography in testicular pathology may be broadened.
ACKNOWLEDGMENTS
The authors would like to thank the respective Institutions.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHOR CONTRIBUTIONS
Vito Cantisani and Nicola Di Leo conceived the format of the article and wrote the initial draft of the manuscript. Antonio Granata, Francesco Maria Drudi, Carlo Catalano, and Michele Bertolotto revised the article and made corrections and additions. Giorgia Polti, Eleonora Polito, and Nicola Di Leo conceived the literature search protocol and performed the research of the articles. Giorgia Polti and Eleonora Polito also contributed to the writing of the manuscript. Daniele Fresilli, Patrizia Pacini, Olga Guiban, Giovanni Del Gaudio, and Vincenzo Dolcetti contributed to the design and implementation of the research, established the eligibility criteria, and examined the articles extrapolated from the literature search. Vito D'Andrea, Giovanni Battista Di Pierro, and Marco Verrengia provided figures and legends, worked out the technical details, and made additions and corrections to the manuscript.