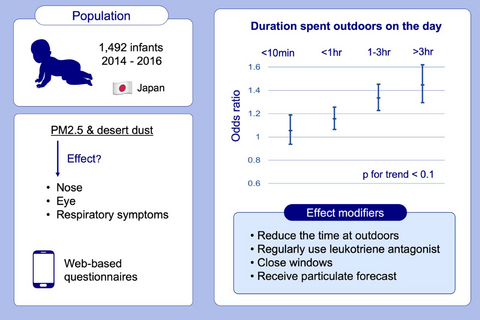
The impact of exposure to desert dust on infants’ symptoms and countermeasures to reduce the effects
Funding information
This work was supported by the Environment Research and Technology Development Fund from the Ministry of the Environment, Japan [5-1555(2015-2017)], and the Environmental Restoration and Conservation Agency, Japan (2014-2016), and was conducted as an adjunct study to the Japan Environment and Children Study (JECS). The findings and conclusions of this article are solely the responsibility of the authors and do not represent the official views of the Japanese government.
Abstract
Background
The association between particulate matter (PM), including desert dust, and allergic symptoms has not been well studied. We examined whether PM exacerbated nose/eye/respiratory symptoms in infants, with a focus on the desert dust element, and assessed possible countermeasures.
Methods
We conducted a panel study of 1492 infants from October 2014 to July 2016 in 3 regions in Japan as an adjunct study of the Japan Environment and Children's Study. Infants’ daily symptom scores and behaviors were acquired by web-based questionnaires sent to mothers, who answered within a day using mobile phones. Odds ratios (OR) for symptom development per increased fine PM or desert dust exposure were estimated. Regular use of medications and behaviors on the day of exposure were investigated as possible effect modifiers.
Results
Infants developed nose/eye/respiratory symptoms significantly more often in accordance with fine particulate levels (adjusted OR per 10 µg/m3 increase: 1.04, 95% confidence interval [CI]: 1.01-1.07). A model including both fine particulates and desert dust showed reduced OR for fine particulates and robust OR for desert dust (adjusted OR per 0.1/km increase: 1.16, 95% CI: 1.09-1.23). An increased OR was observed both in infants who had previously wheezed and in those who had never wheezed. Receiving information on the particulate forecast, reducing time outdoors, closing windows, and regular use of leukotriene receptor antagonists were significant effect modifiers.
Conclusions
Transborder desert dust arrival increased the risk of nose/eye/respiratory symptoms development in infants. Regular use of leukotriene receptor antagonists and other countermeasures reduced the risk.
Graphical Abstract
This is the first study to clearly demonstrate that desert dust was associated with an increased risk of nose/respiratory symptoms in infants. Reducing outdoor duration on the day and regular use of leukotriene receptor antagonists significantly reduces the risk at the exposure. Other effect modifiers include keeping windows closed and receiving particulate forecast.
CONFLICT OF INTEREST
All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf.