Absence of evidence that respiratory viral infections influence pediatric lung transplantation outcomes: Results of the CTOTC-03 study
Abstract
Based on reports in adult lung transplant recipients, we hypothesized that community-acquired respiratory viral infections (CARVs) would be a risk factor for poor outcome after pediatric lung transplant. We followed 61 pediatric lung transplant recipients for 2+ years or until they met a composite primary endpoint including bronchiolitis obliterans syndrome/obliterative bronchiolitis, retransplant, or death. Blood, bronchoalveolar lavage, and nasopharyngeal specimens were obtained with standard of care visits. Nasopharyngeal specimens were obtained from recipients with respiratory viral symptoms. Respiratory specimens were interrogated for respiratory viruses by using multiplex polymerase chain reaction. Donor-specific HLA antibodies, self-antigens, and ELISPOT reactivity were also evaluated. Survival was 84% (1 year) and 68% (3 years). Bronchiolitis obliterans syndrome incidence was 20% (1 year) and 38% (3 years). The primary endpoint was met in 46% of patients. CARV was detected in 156 patient visits (74% enterovirus/rhinovirus). We did not find a relationship between CARV recovery from respiratory specimens and the primary endpoint (hazard ratio 0.64 [95% confidence interval: 0.25-1.59], P = .335) or between CARV and the development of alloimmune or autoimmune humoral or cellular responses. These findings raise the possibility that the immunologic impact of CARV following pediatric lung transplant is different than that observed in adults.
-
- AbbreviationsACR
-
- acute cellular rejection
-
- autoAbs
-
- autoantibodies
-
- BAL
-
- bronchoalveolar lavage
-
- BOS
-
- bronchiolitis obliterans syndrome
-
- CARV
-
- community-acquired respiratory virus infections
-
- CI
-
- confidence interval
-
- CLAD
-
- chronic lung allograft dysfunction
-
- CMV
-
- cytomegalovirus
-
- ColV
-
- collagen type V
-
- CTOT-C
-
- clinical trials in organ transplant in children
-
- DSA
-
- donor-specific human leukocyte antigen antibody
-
- ELISPOT
-
- enzyme-linked immunosorbent spot assay
-
- HR
-
- heart rate
-
- IFN
-
- interferon
-
- IL
-
- interleukin
-
- ISHLT
-
- International Society for Heart and Lung Transplantation
-
- Kα1T
-
- K-alpha 1 tubulin
-
- LAS
-
- lung allocation score
-
- LRTI
-
- lower respiratory tract infection
-
- LRT
-
- lower respiratory tract
-
- LTR
-
- lung transplant recipient
-
- MFI
-
- mean fluorescence index
-
- NP
-
- nasopharyngeal
-
- OB
-
- obliterative bronchiolitis
-
- PBMC
-
- peripheral blood mononuclear cell
-
- PCR
-
- polymerase chain reaction
-
- PGD
-
- primary graft dysfunction
1 INTRODUCTION
Advancements in recipient selection, surgical techniques, evolving immunosuppressive regimens, and more effective infection prophylaxis over the past 25 years have led to improved perioperative survival in pediatric lung transplant recipients (LTRs). However, long-term graft and patient survivals have not improved substantially over the same period and remain significantly worse than outcomes for recipients of heart, liver, and kidney allografts. Beyond the first posttransplant year, chronic lung allograft dysfunction (CLAD) is the most common cause of graft failure. The incidence of bronchiolitis obliterans syndrome (BOS), the most common form of CLAD, is 50% at 5 years in children and roughly 80% between 5 and 10 years in adults.1-3 Between 25% and 40% of lung transplant recipients will die directly or indirectly from CLAD.3 Although retransplant for CLAD is feasible, its utility is limited by organ availability and poorer survival after the second transplant.4-6
The etiology of CLAD remains unclear, but a common theme throughout the spectrum of clinical risk factors that include primary graft dysfunction, recurrent and/or severe acute cellular rejection (ACR), viral infections including cytomegalovirus (CMV), bacterial infection (particularly Pseudomonas aeruginosa), fungal infection, and gastroesophageal reflux, is allograft injury. Acute and chronic lung allograft injury in adults was also associated with the development of autoantibodies (autoAbs) in cross-sectional studies.7 Given accumulating data suggesting a role for both donor-specific anti-HLA antibodies (DSAs) and autoAbs reactive to collagen type V (ColV) and k-alpha 1 tubulin (Kα1T) in the development of CLAD, it is possible that the development of DSAs and autoAbs in response to allograft injury serves as a common pathway.7, 8 The mechanistic link between antibody formation/binding and chronic graft injury remains unclear, although complement-mediated injury, cytokine/macrophage–mediated injury, and direct effects of antibody binding on endothelial or epithelial growth/proliferation may be involved.9-13
Community-acquired respiratory viral infections (CARVs) are frequently reported after lung transplant and cause significant morbidity. Studies of viral isolation from adult LTRs have identified infection with both established respiratory viruses such as rhinovirus, respiratory syncytial virus, parainfluenza virus, and influenza virus14-18 and emerging respiratory viruses, including human metapneumovirus and human coronavirus.17, 19, 20 CARVs are associated with poor long-term outcomes in adult LTRs.21-25
Based on these findings, we hypothesized that CARV infections directly activate the immune system by inducing a proinflammatory environment and thus could (1) directly damage the lung allograft, (2) augment innate immunity leading to direct lung allograft damage, (3) augment innate immunity leading to enhanced adaptive cellular and humoral alloimmunity and or autoimmunity and resultant lung allograft injury, and (4) induce antiviral immunity that could cross-react with lung allograft antigens to mediate graft injury (heterologous immunity).
Despite accumulating evidence in adults, the role the CARVs play in the long-term outcome of pediatric LTRs remains uncertain. A retrospective analysis of CARVs within the first year after transplantation found an association with death but not BOS in a cohort of nearly 600 pediatric LTRs.26 Moreover, there have been no reports supporting a relationship between T cell responses and the development of DSAs or autoAbs in pediatric LTRs or a relationship between DSAs and/or autoAbs and CLAD in pediatric LTRs.
We conducted a prospective, longitudinal study of pediatric LTRs to test the hypothesis that CARVs increase the risk of meeting a composite endpoint consisting of BOS, obliterative bronchiolitis (OB), death, or retransplant in pediatric LTRs. A companion mechanistic study assessed the relationship between CARVs and immunologic events known to be associated with CLAD development.
2 METHODS
2.1 Study development and oversight
The Clinical Trials in Organ Transplant in Children study (CTOTC-03, NCT00891865) enrolled patients at 6 pediatric institutions in the United States from 2009 to 2013. CTOTC-03 was the first prospective, longitudinal study of pediatric LTRs. This prospective multicenter observational trial had a target accrual of 80 pediatric lung or heart–lung transplant recipients (78 enrolled). The CTOTC-03 protocol development team was led by Drs Sweet and Danziger-Isakov. Clinical and/or laboratory data were contributed by Drs Heeger, Mohanakumar, and Storch. Medical safety oversight was provided by Dr Jonah Odim. Data analysis was the responsibility of Karen Kesler and Hyunsook Chin (with the CTOTC-03 team). Data were collected by the investigators and coordinators at each study site. All authors vouch for data accuracy and completeness. Each site participated under the auspices of its institutional review board. An independent, National Institute of Allergy and Infectious Diseases–appointed Data Safety Monitoring Board was responsible for periodic safety review. The study was registered at ClinicalTirals.gov (NCT00891865).
2.2 Subjects
Candidates for first single or bilateral lung or heart–lung transplant who were 19 years old or younger at enrollment were considered for inclusion pending appropriate informed consent. We excluded multiorgan transplant recipients (aside from heart–lung) and recipients with a condition or characteristic that, in the opinion of the local primary investigator, made the participant unlikely to complete the study.
2.3 Endpoints
We tested the hypothesis that CARVs increase the risk of meeting a composite endpoint consisting of BOS, OB, death, or retransplant in pediatric LTRs. We chose this composite endpoint to increase the power to detect an impact, postulating that CARVs result in direct and indirect allograft injury leading to expanded graft-reactive T and B cell immunity and the development of autoimmunity through the unmasking of cryptic autoantigens. We also evaluated the impact of risk factors associated with outcomes in adults such as primary graft dysfunction (PGD) and ACR.
Subjects were followed for at least 2 years or until they met ≥1 components of the composite endpoint, which included death, retransplant, or meeting criteria for BOS grade 0-p or 127 or the finding of OB on lung biopsy. The endpoint included BOS27 because this study was performed before CLAD becoming accepted terminology,28 but all patients identified through the use of the 2001 BOS criteria would meet current CLAD criteria. Subdivision between those with obstructive and restrictive CLAD was not performed.
2.4 Study design
Clinical data (including pulmonary function testing and imaging studies) were collected at scheduled visits, including pretransplant, at transplant (relevant donor demographics were also collected at transplant), and at posttransplant weeks 2, 4, 6, and 8 and months 3, 6, 9, 12, 18, and 24. Blood, NP, and bronchoalveolar lavage (BAL) specimens were obtained at these visits for viral testing and assessment of immunity. Subjects who developed clinical symptoms consistent with CARV had a nasopharyngeal (NP) swab obtained as well as blood and BAL samples if bronchoscopy was performed as part of clinical care. Standard of care included sending BAL specimens (obtained during bronchoscopies performed for routine surveillance or with symptomatic episodes) to the local laboratory to assess for routine bacterial, fungal, mycobacterial, viral, and opportunistic organisms. When BAL was not performed with a symptomatic episode, standard of care generally included sputum culture.
Subjects underwent routine pretransplant evaluation. Posttransplant management followed International Pediatric Lung Transplant Collaborative guidelines (see Data S1). Use of an induction agent was at the discretion of the transplant center: 2 centers used an interleukin (IL)-2 antagonist (42 subjects), 2 centers used rabbit antithymocyte globulin (10 subjects), 1 center used both an IL-2 antagonist and rabbit antithymocyte globulin (6 subjects), and 1 center administered no induction therapy (3 subjects). All subjects received triple drug maintenance immunosuppressive therapy with tacrolimus, mycophenolate, and steroids, with standardized levels for tacrolimus. Pneumocystis, fungal, and CMV prophylaxis were determined by the local center. Treatment of viral infection detected locally was at the discretion of the treating physician. Viral testing of specimens sent to the central laboratories was performed in batches. Therefore, the clinical sites were not informed of these results.
Clinical data were collected from each site using standardized forms. Primary graft dysfunction was determined based on published criteria.29 Bacterial, fungal, viral, and mycobacterial systemic and respiratory tract infections meeting International Society for Heart and Lung Transplantation (ISHLT) working formulation criteria30 were captured based on local clinical data interpretation and intervention as determined by the clinical site primary investigator. After verification of adequate correlation of local biopsy readings with readings made by 2 core pathologists, local pathology readings were used for histologic determination of acute, humoral, and chronic rejection. Centers submitted all pulmonary function data to the data coordinating center (including those obtained during scheduled visits and with acute events). Based on all PFT data, a tentative BOS grade was assigned using an algorithm based on published criteria.27 The local site principal investigator was asked to verify that no concomitant conditions excluding BOS were present before finalizing the BOS grade.
2.5 Laboratory studies
2.5.1 Virology polymerase chain reaction
BAL and NP swab samples obtained at the time points specified here were analyzed in the CTOTC-03 virology core laboratory using the xTAG Respiratory Virus Panel manufactured by Luminex Corp. (Austin, TX) following the manufacturer's instructions. A research use–only panel was used, which included assays for the following viruses: influenza A, influenza A H1, influenza A H3, influenza B, respiratory syncytial viruses A and B, parainfluenza 1–4, enterovirus/rhinovirus, metapneumovirus, adenovirus, and coronaviruses OK43, 229E, NL63, and 229E. Samples with a mean fluorescence index (MFI) ≥1000 were considered positive. Samples with MFI 300 to 999 were retested and considered positive if the repeat MFI was ≥300. If the MFI of the repeat test was <300, the test was repeated a second time, and the sample was considered positive if the MFI of the second repeat test was ≥300. CMV and Epstein-Barr virus in whole blood and BAL were also assessed using polymerase chain reaction (PCR)31 for inclusion in the assessment of the relationship between immunosuppression and viral infection.
2.5.2 Assessment of humoral immunity
Anti-HLA alloantibody testing was performed using Luminex assays.32 DSA were determined by comparing HLA antibody specificities to the donor HLA. Detection of autoantibodies to type V collagen (colV) and K-alpha 1 tubulin (Kα1T) were performed by ELISA methodology using vimentin and myosin as controls.8
2.5.3 Assessment of cellular immunity
Cellular alloreactivity was assessed by cytokine (interferon [IFN]γ) enzyme-linked immunosorbent spot assays (ELISPOT) using donor B cell lines expanded with CD40L-transfected fibroblasts and IL-4 as described previously.33 Specimens with >25 positive cells per 300,000 PBL were considered positive. For T cell autoreactivity, peripheral blood mononuclear cells were tested against recombinant colV (Chemicon/Millipore, Billerica, MA) and Kα1T (recombinant protein expressed in the Mohanakumar laboratory as published)34 using cytokine ELISPOT as well.35
2.5.4 Statistical analyses
Continuous variables were summarized with mean and standard deviation values, and categorical variables were summarized with counts and percentages. Subject characteristics were compared by using χ2, Fisher exact, or Cochran-Mantel-Haenszel tests for categorical variables and t-tests for continuous variables. Time-dependent Cox proportional hazard models were used to examine the associations between viral infections and the composite endpoint as well as between viral infections and the selected mechanistic endpoints. Hazard ratios (HRs) and corresponding 95% confidence intervals (CIs) were reported. Survival curves were estimated by using the Kaplan-Meier method. Because subjects’ infection status could transition between positive and negative, and because of the presence of the endogenous time-varying aspect of viral infection, a sensitivity analysis was performed using multistate and joint survival models.36 Log10 transformations were applied as necessary to satisfy normal distribution assumptions. All statistical analyses were performed using SAS Version 9.4 (SAS Institute, Inc., Cary, NC).
3 RESULTS
3.1 Subject population
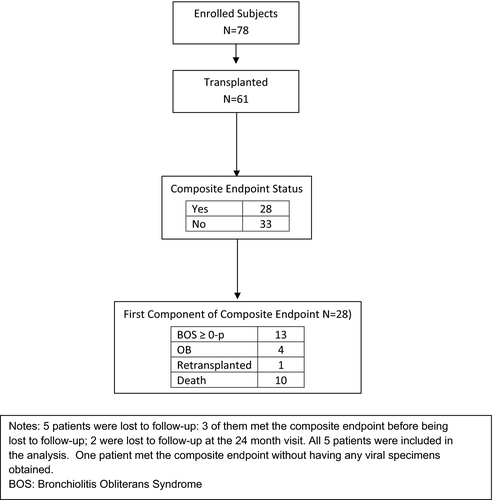
Seventy-eight subjects were enrolled in the study, from which 61 underwent transplant (Figure 1). Twenty-nine (48%) subjects had cystic fibrosis, 11 (18%) had pulmonary hypertension, 9 (15%) had OB, 6 (10%) had interstitial lung disease, 4 (7%) had congenital disorders of surfactant metabolism, and 2 (3%) had other diseases leading to transplant. Mean age at transplant was 11.3 years, ranging from 9 months to 18 years (Table 1). Patients were followed for an average of 20 (±8) months after transplant.
|
All subjects (n = 61), n (%) |
Composite endpoint yes (n = 28), n (%) |
Composite endpoint no (n = 33), n (%) |
P-value | |
|---|---|---|---|---|
| Recipient characteristics | ||||
| Lung allocation score diagnosis group | ||||
| Group A | 1 (1.6) | 1 (3.6) | 0 | .758 |
| Group B | 11 (18.0) | 5 (17.9) | 6 (18.2) | |
| Group C | 29 (47.5) | 13 (46.4) | 16 (48.5) | |
| Group D | 20 (32.8) | 9 (32.1) | 11 (33.3) | |
| Age | ||||
| No. | 61 | 28 | 33 | .859 |
| Mean (SD) | 11.3 (5.46) | 11.5 (5.56) | 11.2 (5.46) | |
| Median | 13 | 13 | 13 | |
| Min, max | <1, 18 | <1, 18 | <1, 18 | |
| Sex | ||||
| Male | 25 (41.0) | 14 (50.0) | 11 (33.3) | .187 |
| Female | 36 (59.0) | 14 (50.0) | 22 (66.7) | |
| Race | ||||
| White | 50 (82.0) | 21 (75.0) | 29 (87.9) | .734 |
| Black or African American | 5 (8.2) | 3 (10.7) | 2 (6.1) | |
| Asian | 2 (3.3) | 1 (3.6) | 1 (3.0) | |
| >1 race | 1 (1.6) | 1 (3.6) | 0 | NA |
| Unknown or not reported | 3 (4.9) | 2 (7.1) | 1 (3.0) | NA |
| Ethnicity | ||||
| Hispanic or Latino | 5 (8.2) | 2 (7.1) | 3 (9.1) | >.999 |
| Not Hispanic or Latino | 42 (68.9) | 19 (67.9) | 23 (69.7) | |
| Unknown or not reported | 14 (23.0) | 7 (25.0) | 7 (21.2) | NA |
| Type of transplant | ||||
| Double lung | 56 (91.8) | 25 (89.3) | 31 (93.9) | .653 |
| Heart–lung | 5 (8.2) | 3 (10.7) | 2 (6.1) | |
| Donor and recipient sex | ||||
| Donor female, recipient female | 18 (29.5) | 3 (10.7) | 15 (45.5) | .028 |
| Donor female, recipient male | 13 (21.3) | 6 (21.4) | 7 (21.2) | |
| Donor male, recipient female | 18 (29.5) | 11 (39.3) | 7 (21.2) | |
| Donor male, recipient male | 11 (18.0) | 7 (25.0) | 4 (12.1) | |
| Induction | ||||
| Anti–interleukin-2 antibody | 44 (72.1) | 22 (78.6) | 22 (66.7) | .241 |
| Thymoglobulin | 14 (23.0) | 6 (21.4) | 8 (24.2) | |
| None | 3 (4.9) | 0 | 3 (9.1) | |
| Donor sex | ||||
| Male | 29 (47.5) | 18 (64.3) | 11 (33.3) | .010 |
| Female | 31 (50.8) | 9 (32.1) | 22 (66.7) | |
| Clinical events | ||||
| Acute cellular rejection | ||||
| Yes | 16 (26.2) | 8 (28.6) | 8 (24.2) | .513 |
| No | 42 (68.9) | 17 (60.7) | 25 (75.8) | |
| Highest acute cellular rejection grade | ||||
| A2 – mild | 14 (23.0) | 7 (25.0) | 7 (21.2) | >.999 |
| A3 – moderate | 2 (3.3) | 1 (3.6) | 1 (3.0) | |
| Antibody-mediated rejection | ||||
| Yes | 11 (18.0) | 6 (21.4) | 5 (15.2) | .504 |
| No | 47 (77.0) | 19 (67.9) | 28 (84.8) | |
- Bold indicates P ≤ .05.
Primary graft dysfunction was common among subjects in this cohort: 33% of the 55 subjects with PGD data available met criteria for grade 2 or 3 PGD within 72 hours.
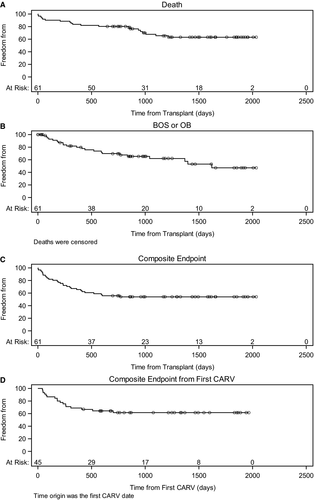
Twenty of the 61 subjects died before the end of the study period. Survival probability was 84% at 1 year and 68% at 3 years (Figure 2A). Chronic rejection (40%) was the most common cause of death, followed by infection (20%). Death from primary graft dysfunction (10%) or posttransplant lymphoproliferative disease (5%) was uncommon in this population. Other causes of death (1 each) included renal failure, liver failure, heart failure, drug overdose, and multisystem organ failure of unknown etiology.
3.1.1 Infection
Lower respiratory tract infections (LRTIs) were reported in nearly all subjects (Table 2). For bacterial LRTI, 22 of the 38 subjects had cystic fibrosis and accounted for 68% of the infections. None of the bacterial LRTIs were the primary cause of death. Thirteen episodes of bacteremia were identified in 10 subjects (16%); 5 of the subjects had bacteremia within the first 90 days after transplant. Bacteremia contributed to 2 of the 4 deaths attributable to infection.
| Infection type | No. of episodes | No. of subjects |
|---|---|---|
| Any infection including CARV, bacterial, viral, fungal, mycobacterial, and protozoan | 416 | 57 |
| At least 1 infection of CARV, bacterial, or fungal LRT and respiratory (unspecified) infection | 268 | 56 |
| No infection at all | — | 4a |
| CARV | 156 | 50 |
| Bacterial (LRT and respiratory [unspecified] infection) | 117 (103 with LRT infection only) | 41 (38 with LRT infection only) |
| Fungal (LRT and respiratory [unspecified] infection) | 39 | 25 |
| Bacterial or fungal (LRT and respiratory [unspecified] infection) | 140 | 46 |
| CARV and either bacterial or fungal (LRT and respiratory [unspecified] infection) at the same time | 37 | 25b |
| CARV and bacterial but no fungal (LRT and respiratory [unspecified] infection) at the same time | 27 | 21b |
| CARV and fungal but no bacterial (LRT and respiratory [unspecified] infection) at the same time | 8 | 8b |
| 3 infections at the same time | 2 | 2b |
| CARV and neither bacterial nor fungal (LRT and respiratory [unspecified] infection) at the same time | 119 | 46c |
| Bacterialaor fungal (LRT and respiratory [unspecified] infection) but no CARV at the same time | 112 | 42c |
| Bacterial and fungal (LRT and respiratory [unspecified] infection) but no CARV at the same time | 8 | 5c |
- a Three subjects who did not have any infection died early between 1 and 27 d posttransplant due to the primary graft failures and cardiac failure. One subject completed the study without any infection and not meeting composite endpoint.
- b The count reflects the number of unique subjects with community-acquired respiratory virus infection (CARV) or lower respiratory tract (LRT) bacterial or fungal infections, regardless of type.
- c Subjects may be counted in >1 row if the subject experienced multiple types of infection.
Of the locally identified viral LRTIs, adenovirus (7) was the most common virus reported followed by parainfluenza (5). CMV pneumonitis was reported in 4 patients. Adenovirus infection contributed to 2 of the 4 deaths attributable to infection. In 20 of 22 (91%) of the locally identified viral infections for which a matching specimen was sent to the CTOTC-03 virology core laboratory, the same virus was identified. Approximately 40% of the locally identified viral LRTIs did not have a central specimen submitted to the core lab.
Consistent with what was previously reported,37none of the fungal LRTIs were contributors to death.
3.1.2 Rejection
A Kaplan-Meier analysis showed the probability of having at least 1 ACR of grade A2 or greater was 21% at 1 year and 30% at 2 years. There were 19 ACRs of grade A2 or greater in 12 subjects within 1 year and 6 ACR episodes in 6 subjects between 1 and 2 years. Thirteen episodes of antibody-mediated rejection were identified in 11 subjects (18%) during the 2-year follow-up period.
The probability of developing either BOS of grade greater than 0-p or a histologic diagnosis of OB was 20% at 1 year and 38% at 3 years (Figure 2B).
3.2 Composite endpoint
Twenty-eight subjects (46%) met ≥1 of the components of the composite endpoint: death, retransplant, or development of BOS or OB (Figure 1). Recipient diagnosis, age, sex, and race/ethnicity were not associated with the composite endpoint (Table 1), nor was type of transplant, transplant time, ischemic time, the use of induction immunosuppressant medications, or the development of PGD, ACR, or antibody-mediated rejection. Univariate analyses showed that recipients receiving organs from a female donor were less likely to meet the composite endpoint, particularly when the recipient was female as well (P = .028). No other donor factors were associated with the composite endpoint. No relationship was found among demographic factors and the separate components of the composite outcome (Tables S1 and S2).
3.3 Mechanistic markers and the composite endpoint
We analyzed serum DSAs and autoAbs in this cohort because the presence of these antibodies has been associated with poor lung transplant outcomes in adults.8, 38-40 Twenty-eight subjects in the cohort developed de novo DSAs. Twenty-one subjects without detectable serum autoAbs pretransplant developed posttransplant autoAbs to ColV, and 26 subjects developed de novo posttransplant autoAbs to Kα1T. We did not detect relationships among any of the antibodies and the composite endpoint. We also quantified pretransplant and posttransplant, donor-reactive and Kα1T-reactive immunity in peripheral blood mononuclear cells by IFNγ ELISPOT. Whereas 10 subjects developed de novo posttransplant donor-reactive cellular responses and 20 subjects developed de novo Kα1T-reactive cellular immunity, we did not observe relationships between either of these parameters and the composite endpoint (Table 3). Nor did we observe significant correlations between the composite endpoint (or its components) and the presence of posttransplant humoral or cellular reactivity to either alloantigens or autoantigens whether or not de novo (Table 3).
| Mechanistic assays |
All subjects (n = 61), n (%) |
Composite endpoint yes (n = 28), n (%) |
Composite endpoint no (n = 33), n (%) |
P-value |
|---|---|---|---|---|
| Pretransplant to posttransplant antibody status | ||||
| Collagen V | ||||
| Negative to negative | 10 (16.4) | 7 (25.0) | 3 (9.1) | .135 |
| Negative to positive | 21 (34.4) | 8 (28.6) | 13 (39.4) | |
| Ka1T | ||||
| Negative to negative | 3 (4.9) | 2 (7.1) | 1 (3.0) | .553 |
| Negative to positive | 26 (42.6) | 10 (35.7) | 16 (48.5) | |
| Donor-specific antibody | ||||
| Negative to negative | 28 (45.9) | 11 (39.3) | 17 (51.5) | .420 |
| Negative to positive | 28 (45.9) | 14 (50.0) | 14 (42.4) | |
| Posttransplant antibody status | ||||
| ELISA: autoantibodies | ||||
| Collagen V | ||||
| Positive | 46 (75.4) | 17 (60.7) | 29 (87.9) | .038 |
| Negative | 13 (21.3) | 9 (32.1) | 4 (12.1) | |
| Missing | 2 (3.3) | 2 (7.1) | 0 | NA |
| Ka1T | ||||
| Positive | 56 (91.8) | 24 (85.7) | 32 (97.0) | .578 |
| Negative | 3 (4.9) | 2 (7.1) | 1 (3.0) | |
| Missing | 2 (3.3) | 2 (7.1) | 0 | NA |
| Anti-HLA antibodies | ||||
| Class I | ||||
| Positive | 33 (54.1) | 12 (42.9) | 21 (63.6) | .179 |
| Negative | 26 (42.6) | 14 (50.0) | 12 (36.4) | |
| Missing | 2 (3.3) | 2 (7.1) | 0 | NA |
| Class II | ||||
| Positive | 31 (50.8) | 13 (46.4) | 18 (54.5) | .728 |
| Negative | 28 (45.9) | 13 (46.4) | 15 (45.5) | |
| Missing | 2 (3.3) | 2 (7.1) | 0 | NA |
| Donor-specific antibody | ||||
| Yes | 30 (49.2) | 14 (50.0) | 16 (48.5) | .795 |
| No | 30 (49.2) | 13 (46.4) | 17 (51.5) | |
| ELISPOT | ||||
| Pretransplant to posttransplant ELISPOT status | ||||
| Donor-specific ELISPOT (≥25) | ||||
| Negative to negative | 19 (31.1) | 10 (35.7) | 9 (27.3) | .433 |
| Negative to positive | 10 (16.4) | 3 (10.7) | 7 (21.2) | |
| Kα1T specific ELISPOT (≥5) | ||||
| Negative to negative | 3 (4.9) | 1 (3.6) | 2 (6.1) | >.999 |
| Negative to positive | 20 (32.8) | 9 (32.1) | 11 (33.3) | |
| Posttransplant donor-specific ELISPOT (≥25) | ||||
| Positive | 16 (26.2) | 6 (21.4) | 10 (30.3) | .368 |
| Negative | 21 (34.4) | 11 (39.3) | 10 (30.3) | |
| Posttransplant Kα1T specific ELISPOT (≥5) | ||||
| Positive | 52 (85.2) | 22 (78.6) | 30 (90.9) | >.999 |
| Negative | 6 (9.8) | 3 (10.7) | 3 (9.1) | |
3.4 Viral infection and the composite endpoint
The virology core laboratory evaluated 397 BAL and 480 NP specimens for viral pathogens. Of these, CARVs were detected in 156 subject visits. In 40 of these, both BAL and NP specimens were positive. In 26, the BAL alone was positive, whereas 90 had only a positive NP sample (this includes symptomatic episodes where no BAL was obtained). Of the CARVs identified in positive specimens, in 116 (74%) of the visits the specimen was positive for enterovirus/rhinovirus. Eight subjects had successive samples positive for enterovirus/rhinovirus, suggestive of persistent infection.
To investigate the association between CARVs and composite endpoint, we considered only CARVs that occurred on or before the subject's known endpoint status. Of subjects who had at least 1 BAL or NP specimen positive for CARVs, 38% (17/45) met the composite endpoint (11 BOS/OB, 5 death, 1 retransplant). In contrast, two-thirds of subjects who did not test positive for CARV (10/15) met the composite endpoint (6 BOS/OB, 4 death). When CARV with symptoms was evaluated, this difference was more pronounced. Only 20% of subjects with symptomatic CARVs (4/20) met the composite endpoint (Table 4).
| Met composite endpoint (death, retransplant, or bronchiolitis obliterans syndome/obliterative bronchiolitis) within 24 mo | |||
|---|---|---|---|
| CARV: (rhinovirus + other) |
Total (n = 60),a n (%) |
Yes (n = 27), n (%) |
No (n = 33), n (%) |
| BAL or NP | |||
| Yes | 45 (73.8) | 17 (63.0 | 28 (84.8) |
| No | 15 (24.6) | 10 (37.0) | 5 (15.2) |
| Symptomatic CARV | |||
| Yes | 20 (32.8) | 4 (14.8) | 16 (48.5) |
| No | 40 (65.6) | 23 (85.2) | 17 (51.5) |
- Abbreviations: CARV, community-acquired respiratory virus; BAL, bronchoalveolar lavage; NP, nasopharyngeal swab.
- a One subject met the composite endpoint without having any viral specimens obtained.
However, recognizing that the subject's CARV status could change over time, we utilized a time-dependent Cox analysis. First, we focused on the transitions from positive to negative or negative to positive. We found no relationship between the presence of CARV by PCR and the composite endpoint (Table 5). Second, when the presence of CARV was treated as an absorbent state (ie, a subject is considered permanently positive for CARV after the initial exposure), the HR was 0.8 with a 95% CI of 0.3 to 2.5 and P = .73. These findings, which were contrary to the primary hypothesis, led us to suspect competing risk bias in the simpler χ2and Kaplan-Meier analyses, so to support the Cox model we added a sensitivity analysis of multistate and joint survival models. As with the Cox model, no relationship between the presence of CARVs and the composite endpoint was found (data not shown).
| Variable | Hazard ratio (95% lower CL, upper CL) | P-value |
|---|---|---|
| Any virus | 0.57 (0.26, 1.25) | .161 |
| Any virus with symptoms | 0.66 (0.2, 2.2) | .497 |
| CARV | 0.64 (0.25, 1.59) | .335 |
| CARV with symptoms | 0.94 (0.22, 4.03) | .937 |
- Abbreviations: CARV, community-acquired respiratory virus; CI, confidence interval.
No relationship was found when we limited the analysis to paramyxovirus, influenza, and adenovirus episodes when we looked for relationships between the timing of the viral episode (occurring within the first 3 months or the first 6 months) or the number of independent viral episodes and the composite endpoint. We also observed no relationship between presence of CARVs by PCR and the individual components of death (HR = 0.8, CI = 0.2-3.2, P = .80) and the development of BOS (HR = 0.4, CI = 0.1-1.7, P = .20).
In addition, we did not observe statistically significant relationships when we repeated these analyses including viral infection data as reported by the local clinical laboratories (HR = 0.5, CI = 0.2-1.4, P = .21).
3.5 Viral infection and mechanistic endpoints (alloimmunity and autoimmunity)
We subsequently tested for relationships between viral presence and the development of markers of humoral and cellular alloimmunity and autoimmunity. Recovery of CARVs from airway specimens was not related to the development of DSAs, autoAbs (CoIV and Kα1T), and Kα1T specific ELISPOT (Table 6). The presence of a CARV was associated with an increased risk for subsequent development of ColV autoAbs. Because there were multiple CARVs at different times, the time-dependent Cox model was used (HR = 3.1, CI = 1.2-8.1, P = .02).
| Mechanistic assays |
All subjects (n = 60),a n (%) |
CARVs (n = 45), n (%) |
No CARVs (n = 15), n (%) |
P-value |
|---|---|---|---|---|
| Antibody status posttransplant | ||||
| ELISA: autoantibodies | ||||
| Collagen V | ||||
| Positive | 46 (76.7) | 37 (82.2) | 9 (60.0) | .157 |
| Negative | 13 (21.7) | 8 (17.8) | 5 (33.3) | |
| Missing | 1 (1.7) | 0 | 1 (6.7) | NA |
| Ka1T | ||||
| Positive | 56 (93.3) | 42 (93.3) | 14 (93.3) | >.999 |
| Negative | 3 (5.0) | 3 (6.7) | 0 | |
| Missing | 1 (1.7) | 0 | 1 (6.7) | NA |
| Anti-HLA antibodies | ||||
| Class I | ||||
| Positive | 33 (55.0) | 28 (62.2) | 5 (33.3) | .081 |
| Negative | 26 (43.3) | 17 (37.8) | 9 (60.0) | |
| Missing | 1 (1.7) | 0 | 1 (6.7) | NA |
| Class II | ||||
| Positive | 31 (51.7) | 25 (55.6) | 6 (40.0) | .406 |
| Negative | 28 (46.7) | 20 (44.4) | 8 (53.3) | |
| Missing | 1 (1.7) | 0 | 1 (6.7) | NA |
| Donor-specific antibodies | ||||
| Yes | 30 (50.0) | 24 (53.3) | 6 (40.0) | .493 |
| No | 29 (48.3) | 21 (46.7) | 8 (53.3) | |
| ELISPOT | ||||
| Posttransplant donor-specific ELISPOT (≥25) | ||||
| Positive | 16 (26.2) | 11 (24.4) | 5 (33.3) | .614 |
| Negative | 21 (34.4) | 16 (35.6) | 5 (33.3) | |
| Posttransplant Kα1T specific ELISPOT (≥5) | ||||
| Positive | 52 (85.2) | 41 (91.1) | 11 (73.3) | .149 |
| Negative | 6 (9.8) | 3 (6.7) | 3 (20.0) | |
- Abbreviation: CARV, community-acquired respiratory virus.
- a One subject met the composite endpoint without having any viral specimens obtained.
3.6 Viral infection as a potential surrogate for degree of immunosuppression
Finally, we considered the hypothesis that viral infection might be a surrogate marker for the overall level of immunosuppression. We found no relationship between mean or coefficient of variation of tacrolimus trough levels and the composite endpoint (Table S3). Although decreased frequencies of IFNγ ELISPOTs to polyclonal stimulus with phytohemagglutinin were associated with viral infection (Table 7), we did not detect a relationship between IFNγ producers and the composite endpoint (Table 8).
| Mechanistic assays |
All subjects (n = 60),a n (%) |
Any viral infection (n = 52), n (%) |
No viral infection (n = 8), n (%) |
P-value |
|---|---|---|---|---|
| High immunosuppression per ELISPOT (at least 1 positiveb sample) | ||||
| Yes | 43 (71.7) | 41 (78.8) | 2 (25.0) | .003 |
| No | 16 (26.7) | 10 (19.2) | 6 (75.0) | |
| No. of high immunosuppression samplesb per subject | ||||
| 0 | 16 (26.7) | 10 (19.2) | 6 (75.0) | .055 |
| 1 | 9 (15.0) | 9 (17.3) | 0 | |
| 2 | 7 (11.7) | 6 (11.5) | 1 (12.5) | |
| 3 | 7 (11.7) | 7 (13.5) | 0 | |
| 4 | 11 (18.3) | 11 (21.2) | 0 | |
| 5 | 5 (8.3) | 5 (9.6) | 0 | |
| 6 | 3 (5.0) | 2 (3.8) | 1 (12.5) | |
| 10 | 1 (1.7) | 1 (1.9) | 0 | |
- a One subject met the composite endpoint without having any viral specimens obtained.
- b Samples were considered positive for high immunosuppression if the response to positive control (phytohemagglutinin) was <100 spots and cell viability was >50%.
- Bold indicates P ≤ .05.
|
All subjects (n = 61), n (%) |
Composite endpoint yes (n = 28), n (%) |
Composite endpoint no (n = 33), n (%) |
P-value | |
|---|---|---|---|---|
| High immunosuppression per ELISPOT (at least 1 positivea sample) | ||||
| Yes | 44 (72.1) | 18 (64.3) | 26 (78.8) | .291 |
| No | 16 (26.2) | 9 (32.1) | 7 (21.2) | |
| No. of high immunosuppression samplesa per subject | ||||
| 0 | 16 (26.2) | 9 (32.1) | 7 (21.2) | .473 |
| 1 | 10 (16.4) | 3 (10.7) | 7 (21.2) | |
| 2 | 7 (11.5) | 2 (7.1) | 5 (15.2) | |
| 3 | 7 (11.5) | 3 (10.7) | 4 (12.1) | |
| 4 | 11 (18.0) | 7 (25.0) | 4 (12.1) | |
| 5 | 5 (8.2) | 1 (3.6) | 4 (12.1) | |
| 6 | 3 (4.9) | 2 (7.1) | 1 (3.0) | |
| 10 | 1 (1.6) | 0 | 1 (3.0) | |
- a Samples were considered positive for high immunosuppression if the response to positive control (phytohemagglutinin) was <100 spots and cell viability was >50%.
4 DISCUSSION
In this first prospective, observational, multicenter study of pediatric LTRs, we obtained clinical and mechanistic data on 61 subjects from 6 pediatric lung transplant centers followed for a minimum of 2 years and found comparable outcomes to the most recent ISHLT registry report.3 However, in contrast to studies using adult subjects, we did not find relationships among primary graft dysfunction, ACR, or CARV exposure and BOS/OB or graft loss. Based on the hypothesis that the common link between these different forms of graft injury and chronic allograft dysfunction is stimulation of a cellular and humoral responses directed at the allograft, these observations raise the possibility that the immunologic environment in pediatric lung transplant recipients is different than that of adults.
The indications for lung transplant, incidence of PGD, acute rejection, BOS, and overall survival in this population are comparable to those reported in the most recent ISHLT registry report.3 In contrast to adult LTRs, ACR and PGD were not related to the development of BOS/OB or the composite endpoint.41-43
We found that identification of common respiratory viruses in NP or BAL specimens was not predictive of poor outcome as measured by a composite endpoint of death, retransplant, or development of CLAD based on OB and BOS criteria. Although subjects with a CARV identified in NP or BAL were less likely to meet the composite endpoint, particularly when the CARV was associated with symptoms, this could be due to a competing risk bias in that subjects with good outcomes had more follow-up time to develop more viral infections. The time-dependent Cox analysis partially controls for this bias, and when we did not find a statistically significant difference between the groups, we concluded that the competing risk bias was driving these nonintuitive results.
These findings contrast with previous retrospective studies performed in adult populations. Both prospective21, 44, 45 and retrospective studies46 support a link between CARVs and chronic rejection, particularly when the infection involves the lower respiratory tract and/or is associated with clinical symptoms.46, 47 Specifically, community-acquired respiratory viruses including paramyxoviruses, influenza, and adenovirus have been implicated in OB/BOS.44, 45 Most viral infections in our cohort were asymptomatic, perhaps a reflection of the fact that 75% of the CARVs identified in our population were rhinovirus/enterovirus (which was not a risk factor in adult populations). No relationship was found when we limited the analysis to paramyxovirus, influenza, and adenovirus episodes, but the small number of these episodes limits our power to detect an effect.
Also, in contrast to adult populations, the development of donor-specific humoral alloimmunity and autoimmunity to self-antigens was not correlated to meeting the composite endpoint or any of its components. Single-center analyses of adult LTRs have identified anti-donor HLA antibodies,39, 40 as well as ColV and Kα1T autoantibodies as risk factors for CLAD.8, 48 Similarly, we did not find a correlation between donor-specific alloreactive T cells responsiveness (as assessed by cytokine ELISPOT) in contrast to studies in kidney transplant recipients where ELISPOT reactivity strongly correlates with long-term renal graft function.49-55
Taken together, the absence of a relationship between among CARVs, ACR, and outcome as well as the absence of a relationship between donor and/or self-antigen specific immunity and outcome suggests that these events occurring in the context of the developing immune system of a pediatric patient56 impact transplant outcome differently than they do in adults.
The finding that female subjects, particularly females receiving organs from female donors, were less likely to meet the composite endpoint is difficult to reconcile with the other findings. Although one could hypothesize that females receiving male organs would have increased potential to develop immunity to Y chromosome gene products from the donor, our study population was not adequately powered to evaluate this hypothesis. The impact of gender combinations is not fully studied among LTRs. Indeed, some studies have shown that gender combinations appeared to have a significant impact,57, 58 and others, no effects, on survival of LTRs.59, 60 One single-center, retrospective study of adult LTRs reported a trend toward improved survival in female recipients.61 Our study was not sufficiently powered to dissect this further.
Although the study population was composed of nearly 40% of pediatric lung transplants performed in the United States during the accrual period, it is underpowered. A posthoc power calculation using the observed frequencies in this cohort would require enrollment of 100 subjects to provide 80% power to detect an HR of 2.5. Nonetheless, given that we saw no relationship between infection and the composite endpoint (including an absence of statistical trends), we believe this study provides strong evidence rejecting the original hypothesis. The absence of a relationship between alloimmune and autoimmune responses and the composite endpoint may also reflect inadequate power. The relatively short 2-year follow-up period may have also limited our ability to identify the development of BOS, which is often diagnosed beyond 2 years posttransplant. We plan to obtain 5-year clinical follow-up data to assess this possibility. Because we did not collect data about patients who met exclusion criteria, we cannot rule out a recruitment bias in that regard. A final limitation to our study is that it was performed using BOS rather than CLAD criteria. It is possible that our findings would have been different had we collected sufficient data to characterize patients using current CLAD criteria and chosen a composite endpoint based on 1 of the CLAD subtypes.
Nonetheless, in contrast to the adult population,21, 44-46 respiratory viral infections in pediatric LTRs do not appear to be a predictor for poor outcome. Coupled with the observation that high immunosuppression based on ELISPOT reactivity was associated with viral infection and the observation that a subset of our subjects had persistent rhinovirus infection,62 it is possible that viral infection was a surrogate for immunosuppression in this population. The finding, in a companion study using samples from this population, that low betatorquevirus levels at 6 weeks and 6 months after transplant were associated with death and the composite outcome supports this hypothesis.63
In summary, this comprehensive prospective analysis of pediatric LTRs found comparable outcomes to the most recent ISHLT registry report3 but did not identify relationships among primary graft dysfunction, ACR, or CARVs and graft loss/CLAD. These observations raise the possibility that the immunologic environment in pediatric lung transplant recipients is different than that observed in adults. Further research is needed to determine whether these observations can be correlated with specific immunologic markers and/or warrant changes in screening or immunosuppression therapy in pediatric LTRs.
ACKNOWLEDGMENTS
This research was performed as a project of the Clinical Trials in Organ Transplantation in Children, a collaborative clinical research project headquartered at the National Institute of Allergy and Infectious Diseases. The work was supported by Grant U01 AI077810 “Viral Triggers of Alloimmunity and Autoimmunity in Pediatric Lung Transplantation” from the Division of Allergy, Immunology and Transplantation of the National Institutes of Health.
DISCLOSURE
The authors of this manuscript have no conflicts of interest to disclose as described by the American Journal of Transplantation.
Open Research
DATA AVAILABILITY STATEMENT
The data supporting this publication will be available at ImmPort (immport.org) under study accession SDY960-Viral Triggers of Alloimmunity and Autoimmunity in Pediatric Lung Transplantation.64