Expression of Human CD46 Modulates Inflammation Associated With GalTKO Lung Xenograft Injury
Abstract
Evaluation of lungs from GalTKO.hCD46 pigs, genetically modified to lack the galactose-α(1,3)-galactose epitope (GalTKO) and to express human CD46, a complement regulatory protein, has not previously been described. Physiologic, hematologic and biochemical parameters during perfusion with heparinized fresh human blood were measured for 33 GalTKO.hCD46, GalTKO (n = 16), and WT pig lungs (n = 16), and 12 pig lungs perfused with autologous pig blood. Median GalTKO.hCD46 lung survival was 171 min compared to 120 for GalTKO (p = 0.27) and 10 for WT lungs (p < 0.001). Complement activation, platelet activation and histamine elaboration were significantly reduced during the first 2 h of perfusion in GalTKO.hCD46 lungs compared to GalTKO (ΔC3a at 120′ 812 ± 230 vs. 1412 ± 1047, p = 0.02; ΔCD62P at 120′ 9.8 ± 7.2 vs. 25.4 ± 18.2, p < 0.01; Δhistamine at 60′ 97 ± 62 vs. 189 ± 194, p = 0.03). We conclude that, in addition to significant down-modulation of complement activation, hCD46 expression in GalTKO lungs diminished platelet and coagulation cascade activation, neutrophil sequestration and histamine release. Because GalTKO.hCD46 lung failure kinetics correlated directly with platelet and neutrophil sequestration, coagulation cascade activation and a rise in histamine levels within the first hour of perfusion, further progress will likely depend upon improved control of these pathways, by rationally targeted additional modifications to pigs and pharmacologic interventions.
Abbreviations
-
- βTG
-
- β-thromboglobulin
-
- CD62P
-
- P-Selectin
-
- ELISA
-
- enzyme-linked immunosorbent assay
-
- F1 + 2
-
- prothrombin fragments 1 + 2
-
- GalTKO
-
- α1,3-galactosyl-transferase knockout
-
- HALR
-
- hyperacute lung rejection
-
- hCD46
-
- human membrane cofactor protein, hMCP
-
- hCRP
-
- human complement regulatory protein
-
- hDAF
-
- human decay-accelerating factor, hCD55
-
- hMCP
-
- human membrane cofactor protein, hCD46
-
- PMN
-
- polymorphonuclear leukocyte
-
- PVR
-
- pulmonary vascular resistance
-
- TXB2
-
- thromboxane B2
-
- vWF
-
- von Willebrand factor
Introduction
Major advances have been achieved in survival and function of pig hearts, kidneys and liver xenografts in translational primate models based on genetic modifications to the pig 1-7. The same is true for cell and tissue xenotransplantation 8-10. Pig gene constructs tested to date include removal of the primary carbohydrate target on pig cells, galactose-α(1,3)-galactose, by “knockout” of the α-galactosyl-transferase gene (GalTKO) or introduction of human complement regulatory proteins (hCRPs) such as human membrane cofactor protein (hMCP/hCD46) or human decay-accelerating factor (hDAF/hCD55). With either of these genetic modifications, the incidence of hyperacute rejection and early graft failure of xenogenic hearts, kidneys and livers is significantly reduced 11, 12. In contrast, hCRP or GalTKO-expressing pig lung xenografts remain susceptible to injury (which we term hyperacute lung rejection [HALR]) within minutes to hours after ex vivo perfusion with human blood or and pig-to-baboon models 13-17.
Since GalTKO-transgenic cells are protected from preformed anti-Gal antibodies but can still be recognized by anti-non-Gal antibodies, in vitro experiments have proven that additional expression of hCRP adds further protection from xenogenic cell injury by inhibiting the complement cascade activation, triggered by antibody–antigen binding 18. Recent work from Westall et al 19 demonstrated that GalTKO lungs expressing multiple genetic modifications (hCD55, hCD59) showed improved and sustained pulmonary function in a xenogenic perfusion model.
Here, we test in a large experimental series how the GalTKO.hCD46 phenotype modulates HALR, and begin to reveal the mechanisms underlying GalTKO.hCD46 lung xenograft failure.
Materials and Methods
Animals
Genetically engineered pigs (BW 6–15 kg) lacking the alpha-Gal epitope (GalTKO) with or without human membrane cofactor protein (hCD46) were supplied by Revivicor (Blacksburg, VA).
For GalTKO.hCD46 transgenic pigs, a human CD46 minigene construct, containing the endogenous hCD46 promoter and first two introns of genomic DNA fused to hCD46 coding sequence, was used to produce pigs with constitutive high-level expression of the human complement inhibitor transgene 12. This hCD46 transgenic pig line was cross-bred with homozygous GalTKO pigs 20 over more than four generations to produce a stable GalTKO.hCD46 line.
(The GalTKO lung results reported here were obtained using Revivicor pigs, and do not include previously reported results associated with GalTKO lungs evaluated in collaboration with MGH and Immerge Biotherapeutics, Inc. 14, 15).
All procedures were approved by the Institutional Animal Care and Use Committee at the University of Maryland School of Medicine and were conducted in compliance with National Institutes of Health guidelines for the care and use of laboratory animals.
Lung recovery
Induction of anesthesia and surgical organ dissection were performed as previously described 14, 18. Prior to flushing the lungs, 1-benzylimidazole (5 mg/kg BW; a thromboxane synthase inhibitor; Sigma–Aldrich, St. Louis, MO) and synthetic prostaglandin I2 (0.03 mg/kg BW; Flolan; GlaxoSmithKline, Research Triangle Park, NC) were administered intravenously and allowed to circulate for several minutes.
Lung perfusion
The right and left lungs were separately perfused via the pulmonary artery using side-by-side circuits fashioned from silicon tubing and polyurethane connectors as previously described 13, 21. Results associated with a variety of drug interventions to one lung of each pair will be reported separately. Pulmonary artery flow was measured and recorded with a flowmeter (Model T206; Transonic Systems, Inc., Ithaca, NY). The Digimed System Integrator (Micro-Med, Louisville, KY) was used to provide a continuous measurement of both pulmonary artery and airway pressures via transducers integrated into the perfusion and ventilator circuits, respectively. Pulmonary vascular resistance (PVR) calculation and criteria defining “lung failure” prior to elective experimental termination at 4 h have previously been described 14.
Perfusate preparation
Xenogenic perfusions
Approximately 450 mL of type A or O fresh whole blood was collected from two healthy human blood donors into a blood collection bag, containing 64 mL of CPDA-1. Two units (∼240 mL each) of type-compatible thawed plasma were added for each unit of blood to obtain an initial perfusate volume of about 2 L. Heparin (3 IU/mL blood; Heparin Sodium Injection; Sagent, Schaumburg, IL), calcium chloride (1.3–1.6 mg/mL blood; American Regent, Inc., Shirley, NY) to neutralize the CPDA chelating agent and 8.4% sodium bicarbonate (∼0.84 mg/mL blood, target pH of 7.4; Hospira, Inc., Lake Forest, IL) were added to the blood pool. All blood components were pooled and thoroughly mixed before circuit priming. Preperfusion hematocrit values were similar in all experimental groups (GalTKO.hCD46 16.3 ± 0.4%; GalTKO 17.0 ± 0.6%; WT 15.9 ± 1.5%).
Autologous perfusions
One pint of blood was collected from the venous circulation by gravity drainage into a clinical blood collection bag over 5–15 min, with simultaneous peripheral volume replacement with crystalloid solution to minimize hemodynamic perturbations prior to lung recovery. An equal volume (one pint) of saline was added to dilute the blood to a hematocrit of 16.9 ± 1.6%. Finally, heparin, calcium chloride and HCO3 were added to the perfusate at similar dosages as described for the human blood preparation.
Experimental groups
Human blood was perfused through GalTKO lungs (n = 16) and GalTKO.hCD46 lungs (n = 33). Historical and contemporaneous experiments using WT pig lungs perfused with human blood (n = 16, 10 of which were previously reported 14) and pig lungs perfused with autologous pig blood (n = 12, 10 of which were previously reported 14) are reported for contextual analysis.
Sampling regimen
Baseline blood samples were taken after the blood preparation (“pre” sample), and after circulating the blood in the perfusion circuit for at least 3 min (time 0 sample). Further samples were collected 5′, 15′, 30′, 60′, 120′ and 240′ after lung perfusion was initiated. All samples were stored at −70°C.
Lung tissue samples were collected preperfusion and 10′, 30′, 60′, 120′ and 240′ after perfusion was begun.
Hematologic analysis
Blood cell counts were enumerated by standard automated techniques (Antech Diagnostics, Rockville, MD) in blood samples collected in ethylenediaminetetraacetic acid (EDTA).
Beta-thromboglobulin, thrombin, thromboxane B2, histamine and complement enzyme-linked immunosorbent assays
Beta-thromboglobulin (βTG) and prothrombin fragments 1 + 2 (F1 + 2) were measured by commercial enzyme-linked immunosorbent assay (ELISA) in plasma samples collected in CTAD tubes as previously described 14. EDTA plasma was used to measure histamine (ELISA kit; Li StarFish, Cernusco, Italy) and C3a levels 14. Blood, collected at three time points (0′, 15′ and 60′) in EDTA tubes containing 100 µL (at 10 µg/mL) of meclofenamate (Sigma–Aldrich), was analyzed to measure plasma levels of thromboxane (Thromboxane B2 [TXB2] EIA Kit; Cayman Chemical Company, Ann Arbor, MI; Catalog No. 519031).
Measurement of platelet activation by flow cytometry
Blood samples were stained by mAbs specific for CD41 (as a marker for platelets) (AbD Serotec, Raleigh, NC) and P-Selectin (CD62P) (expressed by activated platelets) (BD Pharmingen, San Diego, CA) and acquired on a FACSCalibur (BD Biosciences, San Jose, CA). Platelets and platelet aggregates, identified by size and by presence of CD41 staining, were analyzed for expression of CD62P by fluorescence-activated cell sorting analysis. Results were expressed as the percentage of CD62P-positive cells among CD41-positive cells.
Measurement of anti-non-Gal antibody levels by flow cytometry
IgM antibody levels were measured in plasma samples collected before lung perfusion (“pre” sample) as previously described 14 with modifications.
Histology and immunochemistry
Lung biopsy specimens obtained during the perfusion and terminally samples were trisected and processed as previously described 14. Frozen tissue sections from optimal cutting temperature-infused biopsy specimens (10′ biopsies) were assessed by immunohistochemistry with mAbs against CD41 (Immunotech, Marseilles, France) at 1:100, C4d (Quidel Corporation, San Diego, CA) at 1:50, human C5b-9 at 1:50 and rabbit anti-von Willebrand factor (vWF) antibody (both Dako, Carpinteria, CA). The deposition of platelets and complement in lung tissue was quantified by staining intensity (from 0 to 3), taking into account both the extent (proportion of endothelial surface with detectable staining) and intensity of staining, relative to standard positive and negative “control” sections.
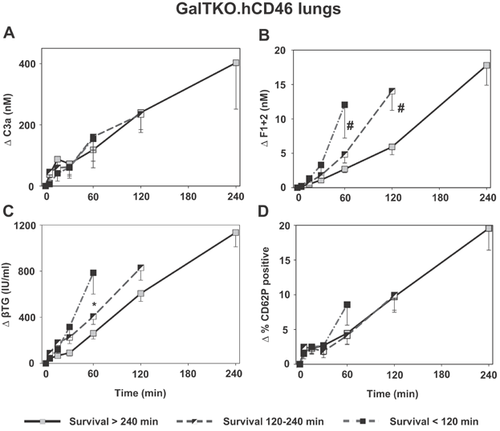
GalTKO.hCD46 group analysis
The GalTKO.hCD46 lung cohorts was arbitrarily divided into three groups according to whether the lungs failed within 120 min (“early”), after 120 but before 240 min (“intermediate”) or did not meet failure criteria at 4 h (“surviving” >240 min). The experimental groups were analyzed for complement cascade activation (C3a), thrombin generation (F1 + 2) and platelet activation (βTG, CD62P).
Statistical analysis
Statistical analysis was performed as previously described 14 using a personal computer with the statistical package SigmaPlot for Windows (Version 11.0; Systat Software, Inc., San Jose, CA).
Results
Graft survival and function
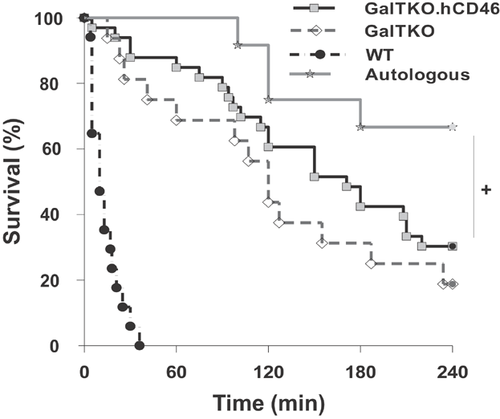
Kaplan–Meier survival analysis (Figure 1) shows that 8 of 12 pig lungs perfused with autologous blood reached elective termination after 240 min of perfusion. In contrast, as previously reported, all xenogenic-perfused lungs of WT pigs failed within 36 min, in association with markedly elevated PVR. GalTKO lungs perfused with human blood survived for a median of 120 min (range 15–240 min) whereas organs from GalTKO.hCD46 animals had a median survival time of 171 min (range 5–240 min; p = 0.27 vs. GalTKO). Three (of 16; 19%) of the GalTKO and 10 (of 33; 30%) of the GalTKO.hCD46 transgenic lungs survived to an elective termination. Although 33% of the autologously perfused lungs failed before reaching the elective termination time point, survival in this cohort was significantly prolonged compared to xenogenetically perfused groups (p = 0.04 vs. GalTKO.hCD46). Gradual loss of pulmonary vascular barrier function, with tracheal edema, was the prevalent lung failure mode in this group. The lung failure modes associated with different lung phenotypes are listed in Table 1.
| Rejection reason | Experimental group n/% of failed lungs | |||
|---|---|---|---|---|
| GalTKO.hCD46 | GalTKO | WT | Autologous | |
| Trachea edema | 7/30% | 2/15% | 2/12% | 3/75% |
| Loss of perfusate | 2/9% | 2/15% | – | 1/25% |
| Loss of blood flow | 12/52% | 7/55% | 15/88% | – |
| Oxygenation failure | 2/9% | 2/15% | – | – |
- Lungs from WT pigs failed almost all due to a loss of blood flow through the lungs (elevated pulmonary vascular resistance) whereas this mechanism is only responsible for about 50% of GalTKO.hCD46 lung failures. The development of trachea edema could be identified as the predominant reason for organ failure within the autologously perfused group.
Pulmonary vascular resistance
Autologously perfused pig lungs maintained very stable and low values over the time of perfusion whereas xenogenetic perfusion of WT pig lungs led to a rapid extreme rise in PVR (284 ± 50 mmHg min/L at 5′) (Figure 2A). Both GalTKO (±hCRP) groups showed an identical moderate rise in PVR to ∼110–140 mmHg min/L within the initial 30 min. At the subsequent measurement intervals, GalTKO.hCD46 transgenic lungs exhibited higher PVR values than with GalTKO organs, reaching statistical significance at 90 min of perfusion (p = 0.04).
Complement activation
In contrast to the prolific elaboration of complement noted with WT xenograft perfusion (ΔC3a at 5′ 2019 ± 377 ng/mL), both GalTKO (63 ± 29, p < 0.001) and GalTKO.hCD46 (33 ± 10, p < 0.001) experimental groups exhibited statistically significantly reduced complement activation. C3a elaboration was not fully inhibited by the additional expression of hCD46, but was significantly reduced at 30′, 60′ and 120′ time points when compared to the GalTKO group (Figure 2B).
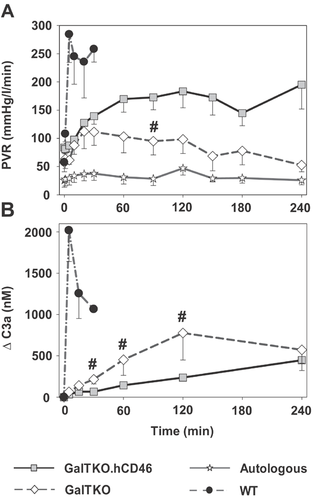
Platelet sequestration and activation
Platelet sequestration by GalTKO.hCD46 lungs was only significantly reduced at 5′ when compared to GalTKO pig lung perfusions (% of initial platelets at 5′ 46 ± 6 vs. 26 ± 4, p = 0.02) (Figure 3A). At later time points (1–4 h of perfusion), there was no statistical significant difference in platelet counts between GalTKO.hCD46 and GalTKO experiments. Activation of platelets measured by CD62P-expression on platelets was significantly decreased between 30 min and 2 h in the GalTKO.hCD46 group when compared to the GalTKO group (ΔCD62 at 120′ 10.2 ± 1.6 vs. 25.4 ± 7.4, p < 0.01). In WT experiments, CD62P-expression was significantly higher when compared to values of GalTKO.hCD46 lungs (Figure 3B).
Plasma TXB2 levels remained lower in the GalTKO.hCD46 than in GalTKO group without reaching statistical significance (ΔTXB2 at 15′ 1.92 ± 0.48 vs. 4.99 ± 1.74 ng/mL, p = 0.17) (Figure 3C).
Plasma βTG rose significantly within 5 min of perfusion in WT lungs (ΔβTG 1286 ± 554 vs. GalTKO 144 ± 36, p = 0.01; vs. GalTKO.hCD46 62 ± 15 IU/mL, p < 0.001). Although the initial rise of βTG level tended to be lower in GalTKO.hCD46 compared to GalTKO lungs during the subsequent hour (at 60′: 440 ± 66 vs. 784 ± 288, p = 0.11), βTG levels after 4 h of perfusion were significantly lower in the three survivors among the GalTKO group when compared to 10 survivors in the GalTKO.hCD46 group (483 ± 54 vs. 1350 ± 133, p < 0.02) (Figure 3D).
Thrombin formation
Relative to prolific, rapid thrombin generation with WT lungs at 30′ (ΔF1 + 2 20.5 ± 9 nM), thrombin generation was significantly reduced in association with GalTKO (2.6 ± 1.3, p < 0.01) or GalTKO.hCD46 lungs (2.1 ± 0.4, p < 0.001) (Figure 4A). Later in the experiment, GalTKO.hCD46 transgenic lungs showed reduced thrombin formation when compared to GalTKO lungs without reaching statistical significance (ΔF1 + 2 at 240′: 13.6 ± 3.6 vs. 25.1 ± 14.1, p = 0.26).
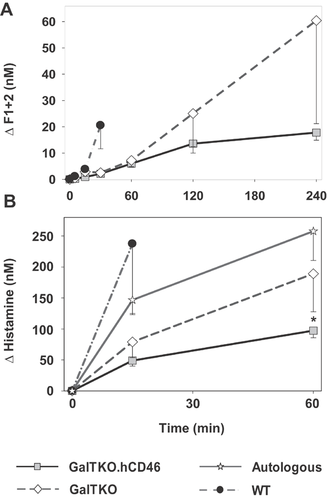
Histamine levels
Histamine, as a marker for mast-cell-driven innate immunologic response, showed a rapid increase in WT lungs at the 15′ time point, significantly higher than in GalTKO.hCD46 lung perfusions (237 ± 113 vs. 49 ± 9 nM, p < 0.01). Levels in GalTKO experiments were higher than with GalTKO.hCD46, reaching statistical significance after 1 h of perfusion (189 ± 61 vs. 97 ± 11, p < 0.03) (Figure 4B). Interestingly, the porcine blood, collected for the autologous perfusions, showed high histamine levels prior to the start of the perfusions whereas the human blood for the xenogenic perfusions had approximately 10-fold lower levels (96 ± 13 vs. 10 ± 1 nM for GalTKO.hCD46).
Leukocyte sequestration
WT, autologously perfused and GalTKO lungs all exhibited immediate neutrophils (polymorphonuclear leukocyte [PMN]) sequestration with 28 ± 13, 54 ± 22 and 45 ± 5 percent of initial neutrophils remaining in the blood after 5′ of perfusion, respectively. During the first half hour of perfusion, neutrophil counts in GalTKO.hCD46 lung perfusions showed significantly higher values when compared to control groups (% remaining at 30′: 59 ± 7 vs. GalTKO 26 ± 4, p < 0.01; vs. WT 7 ± 3, p < 0.01) (Figure 5A). At later time points, there was no statistical difference in PMN sequestration between the groups.

Monocyte counts in GalTKO and WT experiments showed an immediate cell sequestration after perfusion initiation, whereas GalTKO.hCD46 lung perfusions demonstrated a cell number increase at 5′ of perfusion (145 ± 31% of initial monocyte counts) (Figure 5B). Monocyte numbers showed no difference between the groups after 150′ with about 50% of initial monocytes remaining in the perfusate; the relative contribution of pig and human monocytes was not enumerated in the course of the current work.
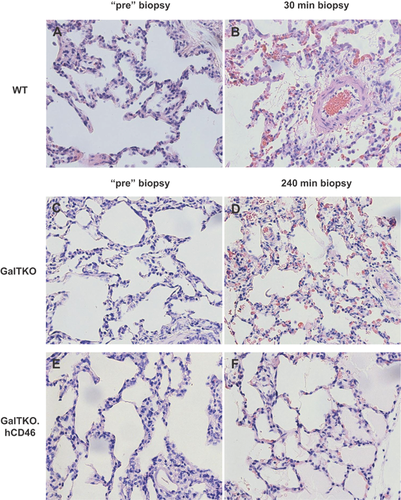
Histology and immunohistochemistry
WT lungs exhibited severe interstitial and alveolar hemorrhage that extended to the airway at failure, along with cellular infiltration and prevalent intravascular thrombosis (Figure 6B). GalTKO lungs showed relatively preserved histology at 60′, but infiltration by polymorphonuclear granulocytes, intravascular thrombosis and hemorrhage were prominent at lung failure (Figure 6D). Only autologously perfused and GalTKO.hCD46 lungs that had not met lung failure criteria showed normal microscopic anatomy with air-filled alveoli and thin inter-alveolar septae at an elective termination after 240′ of perfusion (Figure 6F).
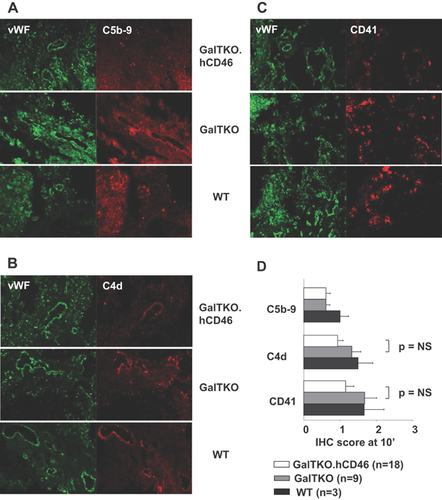
Classical pathway complement activation fragment C4d deposition in 10′ biopsy samples showed the lowest scores in GalTKO.hCD46 tissue (0.94 ± 0.15 vs. GalTKO 1.3 ± 0.25, p = 0.15). C5b-9 membrane attack complex scores were very similar in GalTKO.hCD46 and GalTKO lungs but showed slightly lower values than measured in WT lungs (GalTKO.hCD46 0.61 ± 0.11 vs. WT 1.0 ± 0.24, p = 0.25). CD41 staining, as a marker for platelet deposition, tended toward reduced intensity in GalTKO.hCD46 tissue (1.16 ± 0.23 vs. GalTKO 1.68 ± 0.32, p = 0.19) (Figure 7A–D).
Anti-non-Gal antibody levels
Preperfusion anti-non-Gal IgM antibody levels were comparable in the perfusate used for GalTKO and GalTKO.hCD46 lung perfusions (GalTKO 17.3 ± 6.3 vs. GalTKO.hCD46 15.6 ± 6.9, p = 0.39). Blood used for WT lung perfusions showed significantly lower anti-non-Gal antibody levels (9.2 ± 2.1, vs. GalTKO.hCD46 p < 0.01). In neither group did the individual preformed antibody level correlate to survival time. C3a levels at 15′ and 30′ correlated in the GalTKO group to the level of anti-non-Gal antibody (at 15′ r = 0.62, p < 0.02). This correlation was not significant in the GalTKO.hCD46 group (at 15′ r = 0.28, p = 0.16).
GalTKO.hCD46 group analysis
No difference in the kinetics of complement cascade activation (as ΔC3a) was seen in association with early lung failure relative to longer-surviving lungs (Figure 8A). Thrombin generation (F1 + 2 at 60′ 2.7 ± 0.5 vs. 12.1 ± 4.8, p < 0.02; at 120′ 5.9 ± 1.1 vs. 14.0 ± 1.8 nM, p < 0.02) (Figure 8B) as well as platelet activation (βTG at 60′ 261 ± 50 vs. 786 ± 85 IU/mL, p < 0.02) (Figure 8C) was significantly lower in association with “surviving” lungs when compared to lungs with short- or intermediate-survival times. CD62P-expression on platelets did not differ between groups (Figure 8D).
Discussion
Previously published studies have demonstrated that WT, hCRP and GalTKO xenograft injury can be triggered or accelerated by anti-pig antibody 13, 14, 22, 23, and implicate a combination of complement activation, coagulation cascade activation and cellular adhesion and activation 24-26. The genetic modifications of adding a human complement pathway regulatory protein on the WT pig background or GalTKO alone led to a reduction of complement cascade activation and “survival” prolongation 14. Residual lung injury was attributed in part to binding of classical pathway complement activation triggered by anti-pig antibody 27, 28 or anti-non-Gal antibody 14.
Membrane cofactor protein (CD46) catalyzes the degradation of C3b and C4b by Factor I, thereby inhibiting downstream complement pathway constituents 29, 30 and should thus reduce GalTKO organ injury caused by the complement system. In support of this hypothesis, we find in our study that GalTKO lungs that additionally express human CD46 induced lower C3a generation in the first 2 h of perfusion relative to GalTKO lungs.
We infer that the binding of preformed non-Gal antibodies to GalTKO xenograft, activating leukocytes and endothelial cells as well as the complement cascade, is presumably responsible for acute organ injury. The correlation between preformed non-GalT-antibody levels and lung survival in the GalTKO, but not in the GalTKO.hCD46 group, suggests that the additional complement regulation by overexpression of hCD46 is effective to inhibit, if not prevent, lung injury caused by this mechanism.
Expression of hCD46 on GalTKO lungs modulates platelet activation, as CD41 deposition in the lung and CD62 expression on circulating platelets, and tends to lower thrombin generation. Since expression of hCRPs is not thought to directly inhibit clotting cascade amplification or the adhesion and activation of platelets, we infer that these are indirect effects through reduced complement-driven tissue and cell injury. For example, reduced complement activation may result in less vWF expression on endothelium and diminished vWF secretion into the blood and on circulating human platelets. Although the precise mechanism(s) is not defined by our studies to date, here we show that expression of hCRP on GalTKO organs confers anti-inflammatory, anti-coagulant and anti-thrombotic effects that extend beyond the targeted pathway.
White blood cell and platelet sequestration is observable in all groups, but is greatly accelerated during pig lung perfusion by human blood. Platelet counts in autologous perfusions showed low-level sequestration with about 80% of initial platelets remaining in the perfusate after 2 h of perfusion, illustrating the artifactual effects associated with the ex vivo lung perfusion model. In contrast, more than 50% of initial thrombocytes are sequestered within the first 15 min in xenogenic perfusions, demonstrating a drastic reaction to xenogenic stimuli. Neutrophil sequestration is associated with ischemia-reperfusion injury of allografts 31, 32. We find a neutrophil sequestration in our autologously perfused lungs that is quantitatively similar to that observed in the GalTKO or WT lung perfusions. Interestingly, hCD46 expression on GalTKO led to a significant delay in neutrophil (and monocyte) sequestration when compared to other xenogenetically and autologously perfused experimental groups. We provisionally infer that complement activation plays an important role in cell sequestration in this early perfusion phase, as previously reported 33, and that it can be partly controlled by reduced complement activation seen in the context of genetic “overexpression” of complement regulatory molecules.
The significant rise in PVR in WT perfusions reflects one clinically important physiological consequence of the xenogenic immunologic reaction and the associated rapidly progressive lung injury. GalTKO and GalTKO.hCD46 lung perfusions generally do not exhibit as extreme PVR elevation. Although average PVR values among “survivors” in the GalTKO group remained lower than in surviving GalTKO.hCD46 lungs, this result is biased by the relatively low PVRs in three GalTKO lungs that survived to 4 h. PVR data analysis of the GalTKO lungs revealed that several lungs were censored that just reached the PVR rejection criteria, reducing the average PVR for that group at subsequent time points. In contrast, a higher proportion of GalTKO.hCD46 organs remained in the “still-functioning” group by PVR (and all other) survival criteria, albeit with persistently high PVR, leading to the relatively elevated PVR values for the group.
Preliminary analysis suggests that “failure” of 4 out of 12 autologously perfused lungs prior to elective termination was associated with surprisingly elevated preperfusion histamine levels, which may adversely affect vascular barrier function.
GalTKO lungs expressing hCD46 exhibited better control of the complement cascade activation, as expected, but did not exhibit significantly prolonged survival compared to GalTKO lungs that do not express additional hCRP. As a hypothesis-generating strategy to begin to explain this observation, we compared biochemical indices of inflammation between three groups of GalTKO.hCD46 lungs cohorted according to “survival time” of the lung. The thrombin generation and platelet activation (βTG), but not complement activation, were significantly lower in association with longer-surviving lungs. We infer that the activation of platelets and the coagulation cascade in “nonsurviving” lungs contributed importantly to the organ injury and determined outcome and survival time. In contrast, increased early complement activation (as C3a) was directly correlated with earlier graft failure for GalTKO lungs (Figure S1A). GalTKO lungs that survived until the elective termination also showed a strong trend to reduced βTG levels when compared to earlier failing lungs (Figure S1C), suggesting to us that platelet activation is an important factor contributing to GalTKO lung injury, as for GalTKO.hCD46 lungs in our current report. Thus, this post hoc analysis of intra-group variability in outcome, comparing groups cohorted by arbitrarily selected survival duration intervals, and putative mechanistic indices of specific pathways associated with lung xenograft injury revealed expected (GalTKO) and hypothesis-generating (GalTKO.hCD46) data regarding what pathways remain important to progress toward clinically useful lung xenograft performance.
One limitation to our study is that we did not also study CD46 modification by itself. Thus, we have not formally excluded the possibility that the hCD46 construct used here might alone account for the observed effects. Previous work shows that hCD46 (hMCP) or hCD55 (hDAF) 17, 18, 34, 35 exhibit incomplete protection, similar to the GalTKO results reported here. Based on two decades of work by us and many others, the GalTKO modification is widely viewed by scientists and regulators as an essential component of the pig genetic background needed for proceeding to clinical application most safely, while minimizing recipient immunosuppressive requirements. Repeating the extensive prior work by us and others with hCRP transgenic pig lungs was judged scientifically unnecessary to address our primary objectives: to determine whether hCD46 protects GalTKO lung from complement-driven injury; and to describe its influence on other HALR mechanisms.
In conclusion, GalTKO.hCD46 lungs exhibit biochemically significant and physiologically important protection from antibody- and complement-mediated HALR. Our data and analysis support our working hypothesis that coagulation- and platelet-driven mechanisms are the principal mediators of PVR elevation and injury of GalTKO.hCD46 lungs in our model, although additional roles for residual complement activation, pulmonary intravascular macrophage activation and human leukocytes (neutrophils, monocytes, natural killer cells) remain to be formally evaluated. We predict that efficient control of one or more among several known molecular incompatibilities regulating coagulation and platelet and leukocyte adhesion 36-43 will prove necessary and sufficient to prevent these well-described HALR phenomena, and yield consistent “survival” to 4 h in this model, as well as life-supporting function of pig lungs in baboons and, eventually, in man.
Disclosure
The authors of this manuscript have conflicts of interest to disclose as described by the American Journal of Transplantation. Dr. Pierson serves on the Scientific Advisory Board of Revivicor.
Author Contributions
LB: concept/design, data analysis/interpretation, statistics, drafting article; TS: concept/design, data analysis/interpretation, approval of article; TZ: concept/design, approval of article; ER: concept/design, approval of article; AR: data analysis/interpretation, approval of article; CA: concept/design, approval of article; AL: concept/design, approval of article; XC: concept/design, approval of article; ES: concept/design, approval of article; GB: concept/design, approval of article; AN: concept/design, approval of article; CJP: providing of genetically modified pigs, approval of article; DA: providing of genetically modified pigs, critical revision of article; AMA: concept/design, data analysis/interpretation, statistics, critical revision of article; RNP: concept/design, data analysis/interpretation, statistics, critical revision of article.