Postanastomotic Transplant Renal Artery Stenosis: Association With De Novo Class II Donor-Specific Antibodies
Abstract
In this study, we analyze the outcomes of transplant renal artery stenosis (TRAS), determine the different anatomical positions of TRAS, and establish cardiovascular and immunological risk factors associated with its development. One hundred thirty-seven of 999 (13.7%) patients had TRAS diagnosed by angiography; 119/137 (86.9%) were treated with angioplasty, of which 113/137 (82.5%) were stented. Allograft survival in the TRAS+ intervention, TRAS+ nonintervention and TRAS− groups was 80.4%, 71.3% and 83.1%, respectively. There was no difference in allograft survival between the TRAS+ intervention and TRAS− groups, p = 0.12; there was a difference in allograft survival between the TRAS− and TRAS+ nonintervention groups, p < 0.001, and between the TRAS+ intervention and TRAS+ nonintervention groups, p = 0.037. TRAS developed at the anastomosis, within a bend/kink or distally. Anastomotic TRAS developed in living donor recipients; postanastomotic TRAS (TRAS-P) developed in diabetic and older patients who received grafts from deceased, older donors. Compared with the TRAS− group, patients with TRAS-P were more likely to have had rejection with arteritis, odds ratio (OR): 4.83 (1.47–15.87), p = 0.0095, and capillaritis, OR: 3.03 (1.10–8.36), p = 0.033. Patients with TRAS-P were more likely to have developed de novo class II DSA compared with TRAS− patients hazard ratio: 4.41 (2.0–9.73), p < 0.001. TRAS is a heterogeneous condition with TRAS-P having both alloimmune and traditional cardiovascular risk factors.
Abbreviations
-
- ACR
-
- acute cellular rejection
-
- AMR
-
- antibody-mediated rejection
-
- BP
-
- blood pressure
-
- CAV
-
- cardiac allograft vasculopathy
-
- CDU
-
- color Doppler ultrasounds
-
- CTA
-
- CT angiogram
-
- DSA
-
- donor-specific antibodies
-
- FK
-
- tacrolimus monotherapy
-
- IADSA
-
- intra-arterial digital subtraction angiography
-
- MFI
-
- mean fluorescence index
-
- MMF
-
- mycophenolate mofetil
-
- MRA
-
- magnetic resonance angiography
-
- PTA
-
- percutaneous transluminal angioplasty alone
-
- PTAS
-
- PTA with intra-arterial stenting
-
- TG
-
- transplant glomerulopathy
-
- TRAS
-
- transplant renal artery stenosis
-
- TRAS−
-
- no TRAS
-
- TRAS-A
-
- anastomotic TRAS
-
- TRAS-B
-
- TRAS in a bend or kink
-
- TRAS-P
-
- postanastomotic TRAS
Introduction
Transplant renal artery stenosis (TRAS) is associated allograft dysfunction, refractory hypertension and inferior allograft survival 1, 2. The reported incidence of TRAS has a large interstudy variability and ranges from 1% to 23%, diagnosis depending upon multiple factors including the modality of imaging, screening thresholds, and baseline recipient and donor characteristics 1-10. While the gold standard of imaging for TRAS remains formal angiography, the optimal management after diagnosis continues to be controversial due to the absence of randomized control trials 1, 2.
Risk factors associated with the development of TRAS include older recipient age, extended criteria donors, delayed graft function, prolonged cold ischemic time, acute rejection and cytomegalovirus infection 1, 10, 11. To our knowledge, there have been no published studies looking at the association between donor-specific antibodies (DSA) and the development of TRAS. In contrast, there have been numerous studies looking at the association of DSA and transplant vasculopathy following cardiac transplantation 12-15. Cardiac allograft vasculopathy (CAV) remains one of the leading causes of patient death following cardiac transplantation 16. Etiological factors shown to be associated with the development of CAV include both traditional cardiovascular and immunological risk factors 16. More recently, using sensitive Luminex methods, DSA and, more specifically, HLA class II DSA have been shown to be associated with accelerated CAV and allograft loss 13-15, 17. In renal transplantation, class II DSA have also been shown to be pathogenic and exhibit a strong correlation with chronic antibody-mediated rejection (AMR) and allograft failure 18, 19.
The purpose of this study is (1) to determine the outcomes of TRAS following intervention in a large series of transplant recipients; (2) to analyze the different subtypes of TRAS defined by anatomical position; and (3) to determine if there is an immunological risk in the development of TRAS and if there is an identifiable association between the presence of HLA, DSA and TRAS.
Materials and Methods
Patients
A retrospective cohort study of prospectively collected data was undertaken in patients transplanted at Imperial College Kidney and Transplant Centre between 2005 and 2012. We included both deceased and live donor renal transplants along with simultaneous pancreas–kidney recipients. All patients had a negative cross match (B and T cell complement-dependent cytotoxicity and T cell flow cytometry) pretransplant. We excluded ABO and HLA incompatible transplants who underwent antibody removal therapy pretransplantation. All patients received monoclonal antibody induction with either an anti-CD52 antibody (alemtuzumab [Campath-1H®; Millennium Pharmaceuticals, Cambridge, MA]) or an anti-CD25 antibody (daclizumab [Zenapax®; Roche, Inc., Nutley, NJ] or basiliximab [Simulect®; Novartis Pharma Corp, East Hanover, NJ]). Maintenance immunosuppression included a steroid-sparing, tacrolimus (FK)-based regimen of FK monotherapy in the alemtuzumab-induced patients and FK with the addition of mycophenolate mofetil (MMF) in the anti-CD25-induced patients. All patients received methylprednisolone at the time of transplantation followed by 1 week of corticosteroids only.
Screening for TRAS
All patients undergo regular color Doppler ultrasounds (CDU) in the perioperative period, at times of allograft dysfunction and routinely at 3 months posttransplant. If there is a clinical suspicion, unexplained allograft dysfunction or suggestion of TRAS on CDU, patients are screened by magnetic resonance angiography (MRA). If there is a contraindication to MRA, patients are screened by CT angiogram (CTA). Patients with a positive screening test or continued clinical suspicion proceed to intra-arterial digital subtraction angiography (IADSA).
TRAS was defined as a >50% reduction in vessel lumen or >15 mm Hg pressure drop across a stenosed lesion. Our unit protocol is to treat a significant stenosis with intra-arterial stent placement. Balloon-expandable stents used in our patient cohort include the Palmaz® Blue (Cordis Corp, a Johnson & Johnson Company, Miami, FL), Formula™ (Cook Medical, Bloomington, IN), Medtronic Racer (Medtronic, Minneapolis, MN) and ParaMount™ (eV3® Corporate, Minneapolis, MN). If the lesion is not amenable to stenting, patients either undergo angioplasty alone if possible, or in uncommon situations are left for conservative management.
Rejection and DSA detection
All rejection episodes were biopsy proven and classified using the Banff 07 Classification of Renal Allograft Pathology 20. For the histological analysis a v (arteritis), c (capillaritis), g (glomerulitis) and cg (double contour) score ≥1 was taken as positive. Treatment for rejection was as previously described 21. At the time of screening, patients were on FK ± MMF unless they had experienced preceding rejection, when steroids are introduced. Treated subclinical rejection episodes were included in the analysis. Patients are routinely screened for DSA within our H&I Laboratory at 1, 3, 6 and 12 months posttransplant then yearly thereafter and also at times of allograft dysfunction. Patients are screened initially using LABScreen® mixed beads (One Lambda, Inc., Canoga Park, CA) if nonsensitized and subsequently or primarily screened using LABScreen® single antigen beads if sensitized. We include DSA to HLA-A, -B, -Cw, -DR, -DQ and -DP antigens in our study. A mean fluorescence index (MFI) of >300 by single antigen beads on two separate occasions was taken as positive.
Statistical analysis
All analyses were performed using the statistical package Medcalc version 10.4.3 (Medcalc Software, Ostend, Belgium). Comparisons of means and frequencies of normally distributed variables were calculated using t-tests and chi-squared/Fisher's exact tests. The Mann–Whitney test was used for nonnormally distributed variables. Kaplan–Meier survival analysis was used to compare patient, allograft and rejection-free survival following the initial screening test. Odds ratio was used to analyze the association between DSA and TRAS. Repeated measures analysis of variance was used to analyze within TRAS group and between TRAS group allograft function and blood pressure (BP) postangiography using Greenhouse–Geisser estimates. Multivariable analysis was performed using a Cox-proportional hazards regression model.
Results
Eight hundred forty-seven of 999 (84.8%) patients were screened for TRAS. The modality of primary screening was by MRA scan in 828/847 (97.8%) patients, CTA in 14/847 (1.7%) and an IADSA in 5/847 (0.6%). Two hundred thirty-eight of 849 (28.0%) patients had an IADSA, either because screening imaging was positive or inconclusive or clinical suspicion was highly suggestive of TRAS despite a negative screening test. One hundred thirty-seven of 238 (57.6%) patients had TRAS diagnosed following angiography as shown in Figure 1, giving an overall prevalence of TRAS of 137/999 (13.7%). The mean time to TRAS diagnosis posttransplant was 3.2 ± 3.1 months. The mean time to screening posttransplant in the no TRAS (TRAS−) group was significantly longer than the TRAS+ group with a mean time of 6.1 ± 8.87 months posttransplant, p < 0.001.
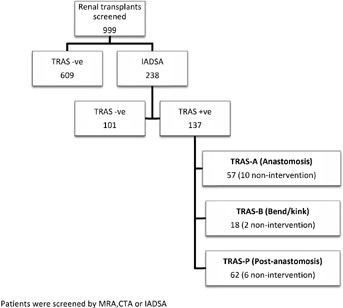
Baseline demographics of our study cohort are shown in Table 1. Of the 137 patients with proven TRAS, 18/137 (13.1%) were unable to undergo intervention due to the complexity of the lesion or the occlusion of the vessel at the time of procedure, 113/137 (82.5%) were treated with an intra-arterial stent and 6 (4.4%) patients underwent angioplasty only. Mean follow-up post-IADSA was 2.7 ± 1.8 years (range 0.05–6.8 years).
| Variable | No TRAS, n = 710 (%) | TRAS, n = 137 (%) | p-Value |
|---|---|---|---|
| Gender (recipient) | |||
| Male | 472 (66.5) | 98 (71.5) | 0.29 |
| Female | 238 (33.5) | 39 (28.5) | |
| Gender (donor) | |||
| Male | 258 (36.3) | 54 (39.4) | 0.98 |
| Female | 402 (56.6) | 83 (60.6) | |
| Age (recipient) | |||
| Years | 47.4 ± 13.0 | 52.5 ± 11.9 | <0.001 |
| Age (donor) | |||
| Years | 46.28 ± 14.1 | 52.6 ± 14.4 | <0.001 |
| Type | |||
| DD | 375 (52.8) | 94 (68.6) | 0.002 |
| LD | 335 (47.2) | 43 (31.4) | |
| Graft | |||
| 1st | 628 (88.5) | 123 (89.8) | 0.76 |
| ≥2 | 82 (11.5) | 14 (10.2) | |
| Time at ESRD | |||
| Pre-emptive | 176 (24.8) | 21 (15.3) | 0.022 |
| Dialysis | 534 (75.2) | 116 (84.7) | |
| Ethnicity | |||
| Caucasian | 356 (50.1) | 47 (34.3) | <0.01 |
| Non-Caucasian | 354 (49.9) | 90 (65.7) | |
| Mismatch | 3.3 ± 1.6 | 3.3 ± 1.6 | 0.99 |
| Sensitization | |||
| NS | 509 (71.7) | 99 (72.3) | 0.99 |
| Sensitized | 135 (19.0) | 25 (18.2) | |
| Preformed | 66 (9.3) | 13 (9.5) | |
| Induction | |||
| Campath | 594 (83.7) | 121 (88.3) | 0.21 |
| IL2RA | 116 (16.3) | 16 (11.7) | |
| Diabetes | |||
| No | 531 (74.8) | 90 (65.7) | 0.036 |
| Yes | 179 (25.2) | 47 (34.3) | |
- DD, deceased donor; ESRD, end-stage renal disease; IL2RA, IL-2 receptor antibodies; LD, living donor; NS, nonsensitized; TRAS, transplant renal artery stenosis.
- Boldface data indicate statistical significance at the p < 0.05 level.
Allograft outcomes
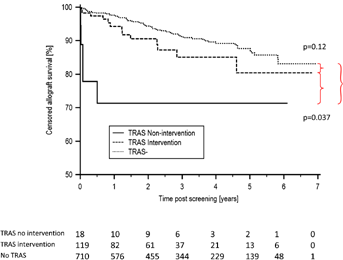
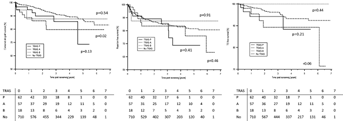
Patients with TRAS had inferior allograft survival. One-, 3- and 5-year censored allograft survival was 91.2%, 83.5% and 79.5% in the TRAS+ group compared with 97.6%, 91.2% and 87.6% in the TRAS− group, p = 0.007. Analyzing allograft survival separately by treatment in the TRAS+ patients (intervention and nonintervention), a disparity was seen between the subgroups. Allograft survival in the TRAS+ intervention, TRAS+ nonintervention and TRAS− groups was 80.4%, 71.3%, and 83.1%, respectively, as shown in Figure 2. Comparing the subgroups, there was no significant difference in allograft survival between the TRAS− and TRAS+ intervention group, p = 0.12. However, there was a significant difference in allograft survival between the TRAS− and TRAS+ nonintervention group, p < 0.001, and also between the TRAS+ intervention and TRAS+ nonintervention groups, p = 0.037.
Association between rejection, DSA and TRAS
There was no difference in the number of acute rejection episodes prescreening in the TRAS− and TRAS+ patients. Seventy-one of 710 (10.0%) TRAS− patients had rejection prescreening compared with 18/137 (13.1%) TRAS+ patients, p = 0.34. Overall rejection-free survival postscreening was no different between the TRAS+ and TRAS− groups at 64.7% and 80.9%, respectively, p = 0.33; with an acute cellular rejection (ACR)-free survival of 87.0% and 83.3%, p = 0.61; and an AMR-free survival of 84.2% and 95.8%, p = 0.59, respectively. There was a trend toward inferior transplant glomerulopathy (TG)-free survival in the TRAS+ patients compared with the TRAS− group, with a TG-free survival of 77.4% and 92.4%, respectively, p = 0.087.
Thirteen of 137 (9.5%) TRAS+ patients and 66/710 (9.3%) TRAS− patients had low-level preformed DSA at the time of transplantation, p = 0.81. Of the patients without preformed DSA, 15/124 (12.1%) TRAS+ patients had developed de novo DSA prescreening, compared with 55/644 (8.5%) TRAS− patients, p = 0.28. Of these, 12/124 (9.7%) TRAS+ patients had developed de novo class II DSA compared with 31/644 (4.8%) TRAS− patients, p = 0.052; 6/124 (4.8%) TRAS+ patients had developed de novo class I DSA prescreening compared with 35/644 (5.4%) TRAS− patients, p = 0.96. A list of the DSA detected by specificity and MFI is shown in Table 2. Following screening, a further 7/109 (6.4%) TRAS+ and 51/615 (8.3%) TRAS− patients developed de novo DSA, p = 0.64, during follow-up.
| Group | CI specificity | CII MFI | CII specificity | CII MFI | CI and CII specificities | CI and CII MFI |
|---|---|---|---|---|---|---|
| No TRAS (n = 710) | A2 | 1262 | DQ2 | 400 | B8, B44, Cw16, DQ5, DQ7, DR4 | 4100, 1800, 500, 1300, 900, 300 |
| A2, A25, B50 | 4500, 4600, 2300 | DQ7 | 6176 | B50, DQ7 | 1700, 2200 | |
| Cw7 | 400 | DQ7 | 759 | B44, DR7, DR53, DQ7 | 4453, 4098, 2212, 1809 | |
| Cw7 | 938 | DQ2, DQ7 | 640, 360 | B8, DQ2 | 724, 2600 | |
| A30, A66 | 1300, 700 | DQ6 | 900 | B58, B44, DR53 | 3318, 1817, 495 | |
| B41 | 6300 | DR1 | 379 | A11, DQ6 | 3477, 820 | |
| B41 | 405 | DQ6 | 1200 | A2, DQ7 | 1710, 730 | |
| B57 | 1050 | DQ7 | 3300 | B8, DR7 | 412, 700 | |
| A1 | 1200 | DR4 | 330 | A32, DR7 | 960, 2700 | |
| B49 | 500 | DQ7 | 2140 | Cw8, A33, DR1 | 5600, 1200, 1560 | |
| A1, B8 | 550, 400 | DR52 | 700 | A32, Cw16, DR12 | 2800, 2380, 9500 | |
| Cw16 | 400 | DR4 | 6550 | |||
| Cw10 | 3956 | DR1, DQ5 | 1560, 970 | |||
| B27 | 528 | DQ7 | 6600 | |||
| A2, Cw5 | 6088, 745 | DQ7, DR53 | 1600, 3200 | |||
| Cw10 | 1060 | DR7 | 3000 | |||
| B55, B62 | 400, 325 | DQ6 | 3050 | |||
| B55 | 3420 | DQ8 | 3800 | |||
| B13 | 2730 | DQ5 | 330 | |||
| B7 | 1170 | DR4 | 1950 | |||
| A2 | 470 | |||||
| A32, Cw8 | 2450, 1350 | |||||
| B38, A24, Cw12 | 1430, 2000, 2550 | |||||
| A25 | 1200 | |||||
| TRAS-P (n = 62) | A25 | 400 | DQ2 | 650 | Cw6, DQ5 | 7640, 5800 |
| DR1 | 600 | A1, B44, Cw5, DQ6, DR13 | 1140, 3050, 2000, 3100, 560 | |||
| DQ2 | 500 | A29, Cw16, DQ8, DQ4 | 550, 520, 1380, 420 | |||
| DQ7 | 686 | |||||
| DR7 | 1000 | |||||
| TRAS-A (n = 57) | A24, Cw15 | 2400, 1000 | DQ6 | 786 | ||
| DR13 | 500 | |||||
| TRAS-B (n = 18) | Cw1 | 623 | DQ7, DR4 | 4747, 362 | ||
| Cw2 | 470 |
- CI, class I; CII, class II; DSA, donor-specific antibodies; MFI, mean fluorescence index; TRAS, transplant renal artery stenosis; TRAS-A, anastomotic TRAS; TRAS-B, TRAS in a bend or kink; TRAS-P, postanastomotic TRAS.
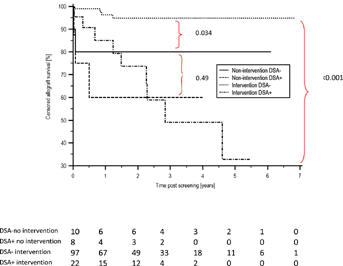
Six of 18 (33.3%) TRAS+ nonintervention group had DSA compared with 22/119 (18.5%) TRAS+ intervention group by the time of diagnosis, p = 0.25. There was no difference in allograft survival between the DSA+ nonintervention group and DSA+ intervention group, with an allograft survival of 66.7% and 32.7%, respectively, p = 0.88. However, in the DSA− patients, TRAS+ allograft survival was significantly higher in the intervention compared with the nonintervention groups at 94.8% and 75.0%, respectively, p = 0.0029, as shown in Figure 3.
Allograft function and BP
There was a significant difference in allograft function between the TRAS− and TRAS+ intervention group at the time of IADSA, with a mean serum creatinine of 153.9 ± 58.7 and 190.6 ± 86.4 µmol/L, respectively, p = 0.043. There was a significant improvement in function from 2 months following intervention in the TRAS+ group, with the mean serum creatinine falling from 190.6 ± 86.1 to 161.4 ± 55.9 µmol/L, p < 0.01. There was no change in allograft function within the TRAS− group, p = 0.20. Further details on allograft function are shown in Table S1.
The TRAS+ intervention group had a significantly higher systolic BP pre-IADSA than the TRAS− group with a mean systolic BP of 151.6 ± 18.4 and 142.1 ± 15.9 mm Hg, respectively, p < 0.01. There was no difference in the number of antihypertensive agents prescribed per patient in the TRAS− and TRAS+ intervention group, with a median number of two (range 0–5) agents per patient in each group, p = 0.77. In the TRAS+ intervention group there was a significant improvement in systolic BP postprocedure, p < 0.01, with no difference in the mean number of antihypertensive agents used, p = 0.11; further BP details are shown in Tables S2 and S3.
Complications and outcomes following IADSA
The overall complication rate following IADSA was highest in the TRAS intervention group with 18/119 (15.1%) having a reported complication compared with 3/101 (3.0%) TRAS− group and 2/18 (11.1%) TRAS nonintervention group, p = 0.0096. There were only 6/238 (2.5%) major complications, five in the intervention group and one in the TRAS+ nonintervention group. These included the use of localized thrombolysis, which required repeat angiogram in three patients, two with large dissection flaps and one with an occluded stent. One patient with a bleeding tendency required vascular oversewing of the arterial puncture site. Two patients lost their grafts following IADSA; one patient had a stent inserted, the other patient had TRAS but the artery was difficult to cannulate and therefore procedure was abandoned. Both patients had subsequent IADSA which documented no flow to the allograft. Both of these patients had developed de novo DSA at the time of initial procedure. Specific complications are summarized in Table 3.
| Complication | No TRAS, n = 101 (%) | TRASi, n = 119 (%) | TRASn, n = 18 (%) |
|---|---|---|---|
| Local hematoma | 1 (0.99) | 3 (2.5) | 0 |
| Pseudoaneurysm | 2 (1.98) | 0 | 0 |
| Dissection (minor—nonflow limiting) | 0 | 5 (4.2) | 1 (5.6) |
| Dissection (major—requiring intervention1) | 0 | 2 (1.68) | 0 |
| Stent malposition2 | 0 | 5 (4.2) | 0 |
| Occluded stent | 0 | 1 (0.84) | 0 |
| Vascular repair | 0 | 1 (0.84) | 0 |
| Allograft loss | 0 | 1 (0.84) | 1 (5.6) |
| Total | 3 (3.0%) | 18 (15.1%) | 2 (11.1%) |
- IADSA, intra-arterial digital subtraction angiography; TRAS, transplant renal artery stenosis; TRASi, TRAS intervention; TRASn, TRAS nonintervention.
- 1 Includes: need for local thrombolysis, stent insertion.
- 2 Includes: stent not covering stenosis, malposition on deployment, occlusion of branch vessel as a consequence of stent position.
Seventy-two of 119 (60.5%) TRAS intervention patients had a further IADSA. Of the 9/119 (7.6%) patients who had angioplasty only at the time of initial procedure, 3/9 (33.3%) of these patients had recurrent stenosis and subsequently underwent stent placement. Twelve of 113 (10.6%) patients with stents developed an in-stent or peri-stent stenosis, which required further angioplasty with or without stent. There was a tendency of increased intervention failure in the angioplasty only group only, although this failed to reach statistical significance, p = 0.08. Seventeen of 119 (14.3%) patients developed a further isolated stenosis away from the initial lesion.
Subanalyses of the different types of TRAS
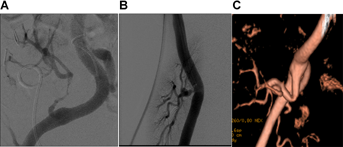
Anatomical position of the stenoses was considered in the 137 patients with TRAS. For analysis purposes, patients were categorized into three different groups, pictorial examples of which are shown in Figure 4. Stenoses occurred either at the anastomosis TRAS (TRAS-A), within a bend or kink in the artery (TRAS-B) or postanastomosis TRAS (TRAS-P), which included those with both discrete and diffuse disease. Fifty-seven of 137 (41.6%) patients had TRAS-A, 18/137 (13.1%) patients had TRAS-B and 62/137 (45.3%) patients had TRAS-P. There was no difference in the time to diagnosis between the groups, with a mean time posttransplant of 3.1 ± 2.7, 2.5 ± 1.5 and 3.7 ± 3.8 months in the TRAS-A, TRAS-B and TRAS-P groups, respectively, p = 0.28.
Risk factors in the baseline demographics for the different type of stenoses are shown in Table 4. Patients with TRAS-A were more likely to have received a transplant from a living donor. Twenty-eight of 57 (49.1%) TRAS-A patients compared with 1/18 (5.6%) TRAS-B and 13/62 (21.0%) TRAS-P patients had received a transplant from a living donor, p < 0.001. Patients with TRAS-B or TRAS-P were older at the time of transplant and were more likely to receive a kidney from an older donor than TRAS-A patients. The mean age at transplantation in the TRAS-B, TRAS-P and TRAS-A patients was 53.7 ± 11.1, 54.9 ± 11.6 and 49.4 ± 12.0 years, respectively, p = 0.038, while the mean age of the respective donors in these patients was 58.4 ± 8.5, 54.9 ± 13.0 and 48.0 ± 16.2 years, respectively, p = 0.0052. Patients with TRAS-B and TRAS-P were also more likely to be diabetic at the time of transplantation than TRAS-A patients, with 7/18 (38.9%), 28/62 (45.2%) and 12/57 (21.1%) patients, respectively, being diabetic, p = 0.02.
| Variable | TRAS-A (anastomotic), n = 57 | TRAS-P (postanastomotic), n = 62 | TRAS-B (bend/kink), n = 18 | p-Value |
|---|---|---|---|---|
| Gender (recipient) | ||||
| Male | 41 (71.9) | 47 (75.8) | 10 (55.6) | 0.24 |
| Female | 16 (28.1) | 15 (24.2) | 8 (44.4) | |
| Gender (donor) | ||||
| Male | 24 (42.1) | 24 (38.7) | 6 (33.3) | 0.79 |
| Female | 33 (57.9) | 38 (61.3) | 12 (66.7) | |
| Age (recipient) | ||||
| Years | 49.4 ± 12.0 | 54.9 ± 11.6 | 53.7 ± 11.1 | 0.038 |
| Age (donor) | ||||
| Years | 48.0 ± 16.2 | 54.9 ± 13.0 | 58.4 ± 8.5 | 0.0052 |
| Type | ||||
| DD | 29 (50.9) | 49 (79.0) | 17 (94.4) | <0.001 |
| LD | 28 (49.1) | 13 (21.0) | 1 (5.6) | |
| Graft | ||||
| 1st | 49 (86.0) | 56 (90.3) | 17 (94.4) | 0.55 |
| ≥2 | 8 (14.0) | 6 (9.7) | 1 (5.6) | |
| Time at ESRD | ||||
| Pre-emptive | 13 (22.8) | 5 (8.1) | 2 (11.1) | 0.068 |
| Dialysis | 44 (77.2) | 57 (91.9) | 16 (88.9) | |
| Ethnicity | ||||
| Caucasian | 25 (43.9) | 16 (25.8) | 6 (33.3) | 0.12 |
| Non-Caucasian | 32 (56.1) | 46 (74.2) | 12 (66.7) | |
| Mismatch | 3.3 ± 1.6 | 3.4 ± 1.6 | 3.3 ± 1.6 | 0.95 |
| Sensitization | ||||
| NS | 38 (66.7) | 47 (75.8) | 13 (72.2) | 0.35 |
| Sensitized | 11 (19.3) | 10 (16.1) | 5 (27.8) | |
| Preformed | 8 (14.0) | 5 (8.1) | 0 (0) | |
| Induction | ||||
| Campath | 48 (84.2) | 58 (93.5) | 14 (77.8) | 0.12 |
| IL2RA | 9 (15.8) | 4 (6.5) | 4 (22.2) | |
| Diabetes | ||||
| No | 45 (78.9) | 34 (54.8) | 11 (61.1) | 0.02 |
| Yes | 12 (21.1) | 28 (45.2) | 7 (38.9) | |
| Arteries | ||||
| 1 | 36 (63.2) | 46 (74.2) | 16 (88.9) | 0.089 |
| ≥2 | 21 (36.8) | 16 (25.8) | 2 (11.1) | |
- DD, deceased donor; ESRD, end-stage renal disease; IL2RA, IL-2 receptor antibodies; LD, living donor; NS, nonsensitized; TRAS, transplant renal artery stenosis.
Allograft outcomes and association with DSA by TRAS type
There was no difference in the number of rejection episodes between the TRAS groups pre-IADSA, 10/57 (17.5%) TRAS-A, 0/18 (0%) TRAS-B and 10/62 (16.1%) TRAS-P patients had rejection preangiography, p = 0.17. The histological findings of the prescreening rejection episodes in the TRAS-A, TRAS-P and TRAS− patients are shown in Table 5. Compared with the TRAS− group, patients with TRAS-P were more likely to have a rejection episode with arteritis, OR: 4.83 (1.47–15.87), p = 0.0095, and capillaritis, OR: 3.03 (1.10–8.36), p = 0.033. There was no statistical difference in the detection of glomerulitis between the TRAS− and TRAS-P group, OR: 2.07 (0.59–7.28), p = 0.26. Only one patient had a rejection episode with a cg score >1 prescreening. There was no statistical significance between the histological findings with regard to v, c and g lesions between the TRAS− and TRAS-A groups (Table 6).
| TRAS− (n = 710), number | TRAS-A (n = 57) | TRAS-P (n = 62) | |||||
|---|---|---|---|---|---|---|---|
| Number | OR (95% CI) | p-Value | Number | OR (95% CI) | p-Value | ||
| Rejection | |||||||
| All | 74 | 10 | 1.83 (0.89–3.77) | 0.10 | 10 | 1.65 (0.81–3.39) | 0.17 |
| AMR | |||||||
| All AMR | 28 | 4 | 2.60 (0.86–7.90) | 0.09 | 4 | 2.38 (0.79–7.19) | 0.12 |
| Full AMR criteria1 | 20 | 2 | 0.89 (0.21–3.82) | 0.87 | 2 | 0.81 (0.19–3.49) | 0.78 |
| Suspicious AMR2 | 8 | 2 | 3.19 (0.66–15.39) | 0.15 | 2 | 2.93 (0.61–14.08) | 0.18 |
| ACR | |||||||
| Banff BL/I | 40 | 5 | 1.61 (0.61–4.26) | 0.34 | 4 | 1.16 (0.40–3.34) | 0.79 |
| Banff II/III | 6 | 1 | 2.10 (0.25–17.71) | 0.50 | 2 | 3.91 (0.77–19.80) | 0.099 |
| C4d+ rejection | |||||||
| All C4d+ | 29 | 5 | 2.26 (0.84–6.08) | 0.11 | 4 | 1.62 (0.55–4.77) | 0.38 |
| Focal | 13 | 0 | 5.16 (1.77–15.02) | 0.003 | 3 | 2.73 (0.76–9.84) | 0.13 |
| Diffuse | 16 | 5 | 0.37 (0.02–6.18) | 0.49 | 1 | 0.71 (0.09–5.45) | 0.74 |
| DSA + rejection | |||||||
| Preformed | 17 | 3 | 2.26 (0.64–7.97) | 0.20 | 1 | 0.67 (0.09–5.11) | 0.70 |
| Overall de novo | 16 | 1 | 0.80 (0.10–6.14) | 0.83 | 3 | 2.19 (0.62–7.74) | 0.22 |
| CI de novo | 10 | 1 | 1.29 (0.17–10.26) | 0.81 | 2 | 2.32 (0.50–10.81) | 0.29 |
| CII de novo | 9 | 0 | 0.66 (0.04–11.52) | 0.78 | 3 | 3.93 (1.04–14.92) | 0.044 |
| Rejection with arteritis | |||||||
| v ≥ 1 | 10 | 2 | 2.55 (0.54–11.91) | 0.24 | 4 | 4.83 (1.47–15.87) | 0.0095 |
| Rejection with capillaritis | |||||||
| c ≥ 1 | 20 | 2 | 1.25 (0.29–5.51) | 0.76 | 5 | 3.03 (1.10–8.36) | 0.033 |
| Rejection with glomerulitis | |||||||
| g ≥ 1 | 17 | 1 | 0.73 (0.10–5.57) | 0.76 | 3 | 2.07 (0.59–7.28) | 0.26 |
| Rejection with DC3 | |||||||
| cg ≥ 1 | 1 | 0 | – | – | 0 | – | – |
| Rejection with scarring | |||||||
| IFTA > 25% | 3 | 3 | 13.09 (2.58–66.43) | 0.002 | 2 | 7.86 (1.29–47.93) | 0.026 |
- ACR, acute cellular rejection; AMR, antibody mediated rejection; CI, class I, CII, class II; DSA, donor-specific antibodies; IFTA, interstitial fibrous and tubular atrophy; TRAS, transplant renal artery stenosis; TRAS−, no TRAS; TRAS-A, anastomotic TRAS; TRAS-P, postanastomotic TRAS.
- 1 Morphological AMR and C4d+ and DSA+.
- 2 Morphological AMR and C4d or DSA.
- 3 DC, double contours.
| No TRAS, n = 710 (%) | TRAS-A | TRAS-B | TRAS-P | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n = 57 (%) | OR (95% CI) | p-Value | n = 18 (%) | OR (95% CI) | p-Value | n = 62 (%) | OR (95% CI) | p-Value | ||
| Preformed DSA | 66 (9.3) | 8 (14.0) | 1.59 (0.72–3.51) | 0.25 | 0 | 0.26 (0.02–4.40) | 0.35 | 5 (8.1) | 0.86 (0.33–2.21) | 0.75 |
| CI | 38 (5.4) | 4 (7.0) | 1.27 (0.48–3.31) | 0.63 | 0 | 0.39 (0.03–6.52) | 0.51 | 3 (4.8) | 0.73 (0.22–2.43) | 0.61 |
| CII | 20 (2.8) | 3 (5.3) | 1.68 (0.57–4.95) | 0.35 | 0 | 0.65 (0.04–11.0) | 0.76 | 2 (3.2) | 0.81 (0.19–3.49) | 0.78 |
| CI + CII | 8 (11.3) | 1 (1.8) | 0 | 0 | ||||||
| De novo DSA prescreening | 55 (7.7) | 3 (6.1) | 0.70 (0.21–2.32) | 0.56 | 3 (16.7) | 2.14 (0.60–7.63) | 0.24 | 9 (15.8) | 1.86 (0.87–3.98) | 0.11 |
| CI | 24 (3.3) | 1 (2.0) | 0.36 (0.05–2.70) | 0.32 | 1 (5.6) | 1.02 (0.13–7.91) | 0.98 | 1 (1.8) | 1.27 (0.44–3.72) | 0.66 |
| CII | 20 (2.8) | 2 (4.1) | 0.84 (0.20–3.62) | 0.82 | 2 (11.1) | 2.47 (0.54–11.2) | 0.24 | 5 (8.8) | 3.23 (1.41–7.40) | 0.0056 |
| CI + CII | 11 (1.7) | 0 | – | – | 0 | – | – | 3 (5.3) | – | – |
| De novo DSA postscreening | 51 (7.2) | 1 (2.2) | 0.22 (0.03–1.66) | 0.14 | 0 | 0.34 (0.02–5.72) | 0.45 | 5 (10.4) | 1.23 (0.47–3.23) | 0.68 |
| CI | 20 (3.4) | 0 | 0.40 (0.05–3.00) | 0.37 | 0 | 0.57 (0.03–9.78) | 0.70 | 1 (2.1) | 0.78 (0.18–3.37) | 0.74 |
| CII | 20 (2.8) | 0 | 0.40 (0.05–3.00) | 0.37 | 0 | 0.57 (0.03–9.78) | 0.70 | 3 (6.3) | 1.64 (0.52–4.49) | 0.37 |
| CI + CII | 11 (1.9) | 1 (2.2) | – | 0 | 1 (2.1) | |||||
| Overall de novo DSA | 106 (14.9) | 4 (8.2) | 0.45 (0.16–1.28) | 0.14 | 3 (16.7) | 1.02 (0.29–3.57) | 0.98 | 14 (24.6) | 1.65 (0.87–3.13) | 0.12 |
| CI | 44 (6.2) | 1 (2.0) | 0.37 (0.09–1.57) | 0.18 | 1 (5.6) | 0.52 (0.07–3.93) | 0.52 | 2 (3.5) | 1.03 (0.43–2.49) | 0.95 |
| CII | 40 (5.6) | 2 (4.1) | 0.61 (0.19–2.02) | 0.42 | 2 (11.1) | 1.17 (0.26–5.22) | 0.83 | 8 (14.0) | 2.50 (1.26–4.98) | 0.009 |
| CI + CII | 22 (3.4) | 1 (2.0) | – | – | 0 | – | – | 4 (7.0) | – | – |
| Overall DSA | 172 (24.2) | 12 (21.1) | 0.83 (0.43–1.61) | 0.59 | 3 (16.7) | 0.63 (0.18–2.19) | 0.46 | 19 (30.6) | 1.38 (0.78–2.44) | 0.26 |
| CI | 82 (11.5) | 5 (8.8) | 0.75 (0.33–1.69) | 0.48 | 1 (5.6) | 0.31 (0.04–2.34) | 0.26 | 5 (8.1) | 0.91 (0.43–1.89) | 0.79 |
| CII | 60 (8.5) | 5 (8.8) | 0.98 (0.43–2.23) | 0.96 | 2 (11.1) | 0.86 (0.19–3.81) | 0.84 | 10 (16.1) | 2.01 (1.06–3.79) | 0.03 |
| CI + CII | 30 (4.2) | 2 (3.5) | – | – | 0 | – | – | 4 (6.5) | – | – |
- CI, class I; CII, class II; DSA, donor-specific antibodies; TRAS, transplant renal artery stenosis; TRAS-A, anastomotic TRAS; TRAS-B, TRAS in a bend or kink; TRAS-P, postanastomotic TRAS.
- Boldface data indicate statistical significance at the p < 0.05 level.
There was no difference in the number of patients with preformed DSA in the TRAS groups, with 8/57 (14.0%) TRAS-A, 0/18 (0%) TRAS-B and 5/62 (8.1%) TRAS-P having low-level preformed DSA at the time of transplant, p = 0.45, as shown in Table 2. Compared with the TRAS− patients, TRAS-P patients were significantly more likely to have developed a de novo class II DSA by the time of TRAS diagnosis, OR: 3.02 (1.32–6.90), p = 0.0056. No association was seen between TRAS-A and TRAS-B types and the development of de novo DSA.
Allograft survival in the DSA+ TRAS-A and TRAS-P groups was inferior to the DSA− TRAS-A and TRAS-P groups. Allograft survival in the DSA+ and DSA− TRAS-A patients was 28.9% and 92.5%, p < 0.001, and 31.7% and 95.1% in the DSA+ and DSA− TRAS-P patients, respectively, p = 0.0081. There was no difference in allograft survival in the DSA+ and DSA− TRAS-B patients, with a survival of 100.0% and 84.8%, respectively, p = 0.49.
Figure 5 shows a comparison of allograft outcomes following screening between the TRAS− and TRAS groups. Overall allograft survival in the TRAS−, TRAS-P, TRAS-A and TRAS-B patients was 83.1%, 68.6%, 79.7% and 87.7%, respectively, p = 0.087. Compared with TRAS− patients, TRAS-A patients had inferior allograft survival, p = 0.02, and there was a trend toward inferior survival in the TRAS-P patients, p = 0.13. There was no difference in allograft survival between the TRAS− and TRAS-B groups, p = 0.41. Overall ACR-free survival postscreening was 83.3%, 71.4%, 80.6% and 87.4% in the TRAS−, TRAS-P, TRAS-A and TRAS-B patients, respectively, p = 0.94. There was no difference in ACR-free survival between the TRAS− group when individually compared with the TRAS-P group, p = 0.53; TRAS-A group, p = 0.94; or the TRAS-B group, p = 0.89. AMR-free survival in the TRAS−, TRAS-P, TRAS-A and TRAS-B patients was 95.8%, 96.4%, 79.1% and 100.0%, respectively, p = 0.66. There was no difference in AMR-free survival postscreening between the TRAS− group compared with the TRAS-P group, p = 0.87; TRAS-A group, p = 0.30; or the TRAS-B group, p = 0.48. TG-free survival postscreening in the TRAS−, TRAS-P, TRAS-A and TRAS-B patients was 92.4%, 88.3%, 71.4% and 100.0%, respectively, p = 0.14. There was no significance difference in TG-free survival between the TRAS− group compared with the TRAS-P group, p = 0.21; TRAS-A group, p = 0.059; or the TRAS-B group, p = 0.44.
Multivariate analysis
To determine risk factors associated with the development of TRAS-P, donor and recipient age, non-Caucasian ethnicity of recipient, dialysis dependence at the time of transplantation, diabetes in the recipient, and de novo CII DSA were incorporated in a multivariable model. Results are shown in Table 7. Factors found to be associated with enhanced risk of TRAS-P were donor age (hazard ratio [HR]: 1.03 [1.00–1.05], p = 0.019), recipient age (HR: 1.03 [1.00–1.06], p = 0.023), diabetes (HR: 3.20 [1.80–5.72], p < 0.001) and de novo CII DSA (HR: 4.41 [2.00–9.73], p < 0.001). The recipient being of Caucasian ethnicity was protective (HR: 0.50 [0.27–0.93], p = 0.029). No factors were retained in a multivariable analysis of risk factors for TRAS-A. Increasing donor age was associated with the development of TRAS-B (HR: 1.07 [1.02–1.12], p = 0.0048), while receiving a living donor transplant was protective (HR: 0.05 [0.01–0.47], p = 0.01).
| Exp (b) | 95% CI | p-Value | |
|---|---|---|---|
| Live donor | 0.52 | 0.26–1.03 | 0.06 |
| Donor age (years) | 1.03 | 1.00–1.05 | 0.019 |
| Diabetes | 3.20 | 1.80–5.72 | <0.001 |
| Caucasian recipient | 0.50 | 0.27–0.93 | 0.029 |
| De novo CII DSA | 4.41 | 2.00–9.73 | <0.001 |
| Pre-emptive transplant | 0.71 | 0.26–1.97 | 0.51 |
| Recipient age (years) | 1.03 | 1.00–1.06 | 0.023 |
- CII, class II; DSA, donor-specific antibodies; TRAS, transplant renal artery stenosis.
Patients with TRAS-A were less likely to develop a further stenosis than patients in the TRAS-B or TRAS-P group. Three of 18 (16.7%) TRAS-B and 12/62 (19.4%) TRAS-P patients developed a further stenosis compared with 2/57 (3.5%) TRAS-A patients, p = 0.027. A comparison of the histological rejection episodes postprimary IADSA in the patients who developed further stenosis is shown in Table S4. There was no difference in the incidence of in-stent stenosis between the TRAS-A, TRAS-B and TRAS-P groups, being 6/57 (10.5%), 2/18 (11.1%) and 4/62 (6.5%), respectively, p = 0.68.
Discussion
This study has several important findings. First, in the largest series of TRAS treated with intervention we have shown that allograft outcomes are comparable with TRAS− patients in the absence of DSA. Second, TRAS cannot be considered as a single entity, and different anatomical subtypes of TRAS have multifarious associations. Whether management should be tailored to subtype is not answered in this study. Third, TRAS-P is associated with both nonimmunological and immunological factors. Whether the nonimmunological risk factors are attenuated by alloimmune injury will best be answered in a prospective dedicated study. Finally, the novel finding of this study is that the development of de novo class II DSA is associated with TRAS. This potentially has important management implications and patients with class II DSA should be monitored for clinical signs of TRAS and screened accordingly.
With the expanding use of marginal and extended criteria donors the incidence of TRAS may increase in the current era of transplantation, yet how to best manage patients is still unknown and evidence is currently extrapolated from small case–control studies 1, 3-10, 22, 23. Treatment options include conservative management, percutaneous transluminal angioplasty alone (PTA), PTA with intra-arterial stenting (PTAS) or surgical intervention. From published series percutaneous intervention with PTA or PTAS appears to be superior to conservative or surgical treatment 4. Unlike native renal artery stenosis where the benefit of intervention remains controversial, left untreated TRAS is associated with allograft failure 2, 4, 24. Surgical management is associated with a high complication rate and is best reserved for TRAS-A where percutaneous intervention has failed or is not possible 2, 4, 25. Which choice of percutaneous intervention, angioplasty alone or stent insertion should be the first-line treatment is not known. Both procedures have reported good clinical outcomes in terms of improvement of allograft function and BP control 3-5, 8, 9. In the largest reported series to date of intra-arterial stenting of TRAS, Valpreda et al 8 described 30 cases in which technical success was 100%; there was only one complication and restenosis rate was 15.6%. The use of drug-eluting stents may be considered advancement in this technique and might help to reduce the restenosis rate further 3. In comparison, in studies where PTA is undertaken, technical success is reported in up to 93.1% of cases, complication rate is as high as 25.5% and restenosis rates vary between 6.3% and 36% 6, 7, 9, 10. In the studies where PTA is primary treatment, PTAS is often reserved for patients with recurrent stenoses as restenosis rate tends to be higher in patients who undergo PTA 9. A randomized controlled trial is needed to formally answer whether there is a difference in outcomes between the two techniques. However, optimal management of TRAS may be confounded by anatomical subtype and etiological factors.
Postanastomotic stenoses are the predominant anatomical subtype that has been reported in the literature and we found an immunological association in the risk of developing TRAS-P 5. A few other series have suggested a correlation between rejection and the subsequent development of TRAS but only two studies have specifically analyzed the relationship. Wong et al 10 reported 77 cases of TRAS over a long period and demonstrated an association between acute rejection and TRAS. Fernandez-Najera et al 26 described a smaller series in which there were an increased number of vascular rejection episodes in patients with TRAS. No previous study has described a relationship between DSA and TRAS despite the expanding evidence of the role of DSA in renal transplantation. However, in a recent notable study Hill et al 27 demonstrated an association between DSA and accelerated arteriosclerosis in protocol biopsies that was independent of traditional cardiovascular factors. Traditionally mild to moderate arteritis has been considered to be a lesion of ACR; however, there is increasing evidence that v lesions may be associated with AMR 27-29. Conversely, chronic arteriopathy is a diagnostic criterion for chronic AMR and traditionally alloimmune arteriopathy in histological samples has been differentiated from traditional arteriosclerosis by the absence of duplication of the elastica 30. However, the Hill et al 27 study demonstrates that early transplant arteriopathy associated with DSA can be indistinguishable from traditional arteriopathy by as little as 1 year after transplantation. Extrapolation of the correlation between microvasculature transplant vasculopathy and DSA to macroscopic vasculopathy in the form of TRAS was an intuitive hypothesis that has precedence in cardiac transplantation.
In contrast to renal transplantation, the association between macroscopic transplant vasculopathy and DSA has been extensively studied following cardiac transplantation 12-15, 17. CAV is a major cause of patient death following cardiac transplantation and has been shown to be associated with DSA 13-17. According to registry data, 10% of patients have CAV by 1 year and >50% by 10 years 16. Topilsky et al 15 showed that patients with preformed class II DSA developed an accelerated form of CAV within the first year posttransplant detected by both intravascular ultrasound and coronary angiography. Smith et al 14 showed that de novo class II DSA was associated with poor patient survival, and although no direct correlation between DSA and CAV was shown, significantly more patients with DSA died of CAV than patients without DSA. Non-HLA antibodies such as anti-MICA, antivimentin and anticardiac myosin have also been shown to be associated with CAV, AMR and allograft loss following cardiac transplant 17, 31, 32. Non-HLA antibodies including antiendothelial and anti-MICA antibodies have been implicated in renal allograft rejection but there is no documented studies looking specifically at arteriosclerosis, whether microscopic or macroscopic 33-35.
To conclude, this is the largest reported series of TRAS. We have described the favorable outcomes following intervention in DSA− patients, predominantly through the placement of intra-arterial stents. More importantly, we have shown that TRAS is a heterogeneous condition with specific risk factors and have shown that both alloimmune and traditional cardiovascular risk factors are associated with postanastomosis TRAS. This is the first report showing an association between the development of de novo class II DSA and TRAS. Screening for TRAS may be beneficial in patients who develop de novo class II DSA as it offers a potential reversible cause of allograft dysfunction. Further prospective studies will be needed to determine whether DSA are a causative factor of TRAS rather than an association.
Acknowledgments
The authors would like to thank work contributed by the transplant clinic staff, histocompatibility and immunogenetics laboratory, planned investigation unit staff, Dawn Chaquico, and the interventional radiology department at Hammersmith Hospital.
Disclosure
The authors of this manuscript have conflicts of interest to disclose as described by the American Journal of Transplantation. Dr. Adam McLean has received research support from Astellas Pharma. Professor David Taube has received consultation fees from Sandoz.




