Utility of optical coherence tomography in basal cell naevus syndrome: A case report
Abstract
Optical Coherence Tomography (OCT) is a useful non-invasive diagnostic tool for diagnosing and monitoring treatment of basal cell carcinomas. We describe the use of OCT in a patient with Basal Cell Naevus Syndrome. Through measuring tumour depth on OCT, management of individual tumours was triaged accordingly using 0.4 mm tumour depth as a cut-off for surgical and non-surgical management. OCT has potential to reduce unnecessary excisions and associated morbidity in this population of patients.
INTRODUCTION
Basal cell naevus syndrome (BCNS, OMIM #109400), also known as Gorlin syndrome or Gorlin-Goltz syndrome, is a genodermatosis caused by mutations affecting PTCH1, PTCH2 or SUFU of the sonic hedgehog signalling pathway. It is characterized by numerous early onset basal cell carcinomas (BCCs) and other characteristic cutaneous and skeletal features including odontogenic keratocysts and palmoplantar pits. These younger patients pose a management challenge in balancing adequate treatment of BCCs and treatment-related morbidity from a cosmetic and psychological standpoint. Even the simplest histopathological assessment of BCCs with shave biopsy may eventually feel too invasive considering the number of lesions in these patients. As such, effective and non-invasive diagnostic techniques are welcome.
Optical coherence tomography (OCT) utilizes low-coherence infrared light and interferometry. As different structures of the skin have varying optical properties, their varying refractions are captured and combined to produce an image in vivo. It can penetrate skin to depths of up to 2.5 mm depending on the machine and systems used, and can visualize a 6 × 6 mm field. The software allows the user to measure the thickness of structures within the image. In diagnosing BCC, OCT has a sensitivity and specificity ranging from 79%–94% and 85%–96% respectively.1, 2 We report a case of use of OCT for non-invasive diagnosis and management planning in a patient with BCNS.
CASE HISTORY
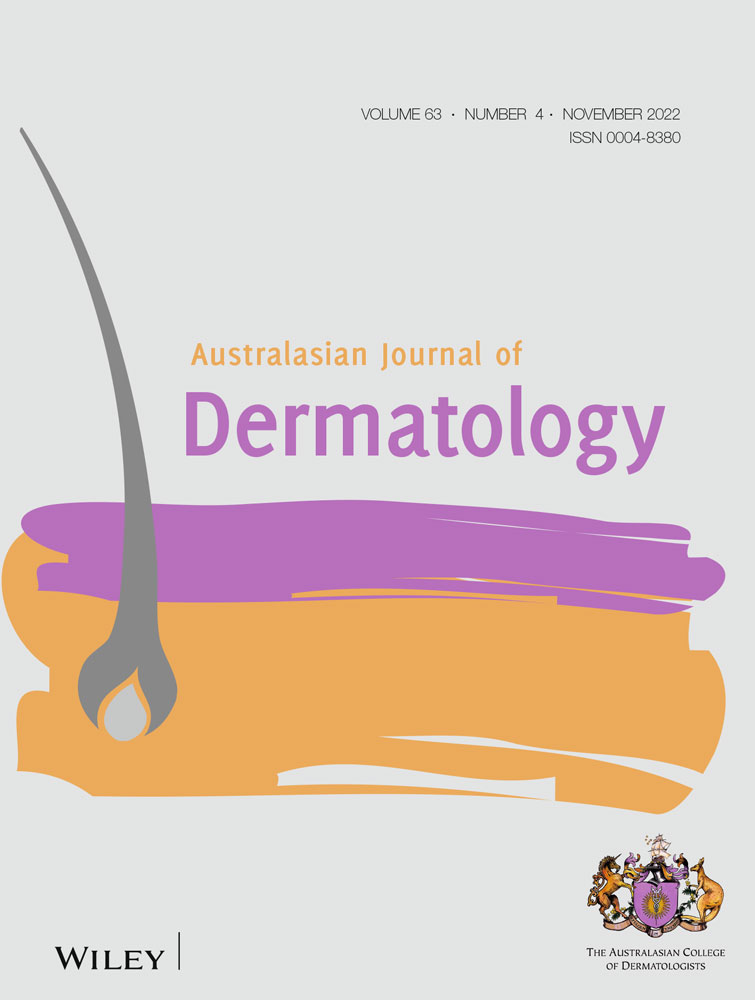
Patient X is a female in her 30s who first developed BCCs at age 25 and who already had 15 BCCs curetted within the preceding 5-year period. She is of Fitzpatrick phototype II, has no history of excessive sun exposure and a family history of a first degree relative with multiple BCCs at a young age. At her first appointment with us, she had 24 lesions suspicious for BCC identified on dermoscopy (Figure 1a). She was noted to have bilateral syndactyly of the second and third toes of each foot. She had a background of papulonodular acne. No other specific features of BCNS were noted. She was confirmed to have a pathogenic variant in the PTCH1 gene (c.3307- 1G>A), thus meeting major criteria for BCNS diagnosis.3
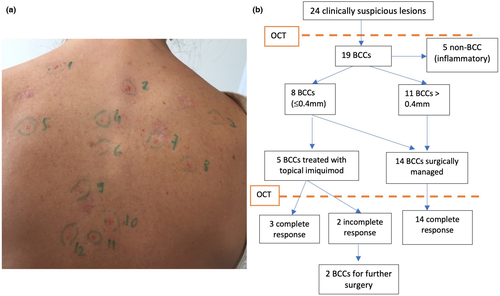
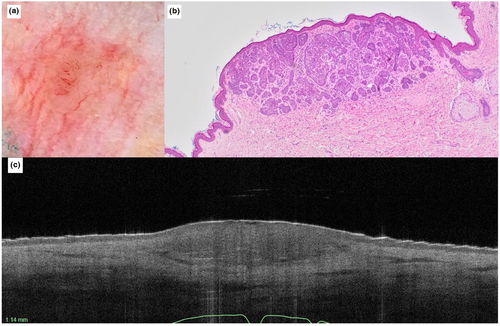
OCT (VivoSight Dx, Michelson Diagnostics Ltd.) was performed on all lesions to guide further management. Diagnostic features of BCC4, 5 were identified in 19/24 lesions, with the remaining five papules presumed to be inflammatory acneiform lesions. The total time taken to scan all 24 lesions was under 30 min. Depth on OCT of BCCs was recorded, and along with anatomical location was used to guide treatment. Tumour depth was measured from the top of the epidermis to the lower margin of the deepest tumour nest. Of the 19 lesions with diagnostic BCC features on OCT, 5/19 lesions were <0.4 mm in depth and were treated as superficial BCCs with topical imiquimod (5 days/week for 6 weeks), excision was performed for 4/19 BCCs >0.4 mm in depth in high risk or cosmetically sensitive areas by a plastic surgeon, and curettage and cautery (C&C) was used to address the remaining lesions due to patient preference (Figure 1b). OCT was used at each subsequent visit to assess response to treatment, and 2/5 BCC's initially treated with imiquimod had incomplete response and were subsequently treated with C&C. OCT was helpful in distinguishing between keloidal scarring at BCC excision sites from recurrent BCC (Figures 2 and 3). At subsequent reviews over the following 9 months, five new BCC's were identified, and again triaged for excisional surgery, topical imiquimod or C&C according to depth of invasion and anatomical location.
DISCUSSION
OCT was a useful tool in triaging and guiding management in this case of BCNS, particularly for dermoscopically equivocal or difficult lesions. When added to dermoscopy, it may increase sensitivity from 90.6% to 95.7%, and specificity from 54.3% to 75.3% (p < 0.001).4 In our case, OCT was also useful in distinguishing BCC from acneiform lesions, and recurrence from scar.
Histopathological correlation with OCT findings has been previously described.4, 5 The main OCT diagnostic features seen in this case were epidermal protrusions into the upper dermis with a dark rim, dark oval structures at varying depths, some with peripheral rimming and disruption of the epidermis.
We relied on tumour depth to guide management. The use of ≤0.4 mm as a cut-off for non-surgical management is based on previous studies where tumour thickness >0.4 mm was predictive of topical imiquimod treatment failure6 and because OCT/histopathological correlation is best when tumour depth is ≤0.4 mm.7 Depth correlation of OCT becomes less accurate with deeper tumours.1, 7 Morphological features on OCT have recently been proposed to better discriminate superficial from non-superficial BCC subtypes, as is done histopathologically.8 Ideally, all BCCs > 0.4 mm should be excised for depth correlation and to confirm subtype and margins. In vivo reflectance confocal microscopy may also assist in confirming diagnosis of BCCs with cellular resolution of tumour morphology, although has a depth limitation of 0.2 mm and is less helpful in guiding treatment option.
In the setting of innumerable BCCs, use of OCT to triage and select tumours for non-surgical management may reduce the cumulative surgical burden in BCNS patients and optimize effective use of non-invasive therapies. OCT is helpful for monitoring treatment response and detecting recurrence, in a time-saving manner (15 s per structural scan). Given that 85% of BCNS patients require some form of annual surgical excision, reported to be the most disliked treatment modality as well as one associated with the highest psychosocial burden,9 non-invasive technologies have an important role in this patient cohort. Larger studies of standardized methodology would be helpful to further define the use of OCT in this population.
AUTHOR CONTRIBUTIONS
GH, RS, BMG and LM contributed to conception and design; GH, RS, PG, NAS, VC, SC and LM contributed to acquisition and interpretation of data; all authors were involved in drafting and revising the manuscript. All authors have given final approval of the version to be published and agree to be accountable for all aspects of the work.
FUNDING INFORMATION
GH is supported by NHMRC CRE funding (#1135285). RJS is supported by the Goodridge Foundation MIA Dermatology Fellowship. LKM is supported by the Warwick L Morison Professorship of Dermatology, UNSW. Sunpharma donated the VivoSightDx device used in this report as a third party sponsored investigator-initiated research grant.
Acknowledgement
Open access publishing facilitated by The University of Sydney, as part of the Wiley - The University of Sydney agreement via the Council of Australian University Librarians.
CONFLICT OF INTEREST
The authors have no conflicts of interest to declare.
INFORMED CONSENT
The patient in this manuscript has given written informed consent to the publication of their case details.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analysed in this study.