The association between alcohol retail access and health care visits attributable to alcohol for individuals with and without a history of alcohol-related health-care use
Funding information: CIHR Catalyst Grant: Alcohol research to inform health policies and interventions.
Abstract
Background and aims
Alcohol retail access is associated with alcohol use and related harms. This study measured whether this association differs for people with and without heavy and disordered patterns of alcohol use.
Design
The study used a repeated cross-sectional analysis of health administrative databases.
Setting, participants/cases
All residents of Ontario, Canada aged 10–105 years with universal health coverage (n = 10 677 604 in 2013) were included in the analysis.
Measurements
Quarterly rates of emergency department (ED) and outpatient visits attributable to alcohol in 464 geographic regions between 2013 and 2019 were measured. Quarterly off-premises alcohol retail access scores were calculated (average drive to the closest seven stores) for each geographic region. Mixed-effect linear regression models adjusted for area-level socio-demographic covariates were used to examine associations between deciles of alcohol retail access and health-care visits attributable to alcohol. Stratified analyses were run for individuals with and without prior alcohol-attributable health-care use in the past 2 years.
Findings
We included 437 707 ED visits and 505 271 outpatient visits attributable to alcohol. After adjustment, rates of ED visits were 39% higher [rate ratio (RR) = 1.39, 95% confidence interval (CI) = 1.20–1.61] and rates of outpatient visits were 49% higher (RR = 1.49, 95% CI = 1.26–1.75) in the highest versus lowest decile of alcohol access. There was a positive association between alcohol access and outpatient visits attributable to alcohol for individuals without prior health-care attributable to alcohol (RR = 1.65, 95% CI = 1.39–1.95 for the highest to lowest decile of alcohol access) but not for individuals with prior health-care attributable to alcohol (RR = 1.08, 95% CI = 0.90–1.30). There was a positive association between alcohol access and ED visits attributable to alcohol for individuals with and without prior health-care for alcohol for ED visits.
Conclusion
In Ontario, Canada, greater alcohol retail access appears to be associated with higher rates of emergency department (ED) and outpatient health-care visits attributable to alcohol. Individuals without prior health-care for alcohol may be more susceptible to greater alcohol retail access for outpatient but not ED visits attributable to alcohol.
INTRODUCTION
Alcohol use is a leading cause of death and disability in Canada and globally [1]. The burden of alcohol on health systems is increasing in high-income countries, particularly in Canada and the United States [2-5]. In addition, alcohol use and consequent morbidity and mortality have increased in North America during the COVID-19 pandemic [6-10]. A large body of research has investigated the effectiveness of different alcohol control policies for reducing health and social harms from alcohol use [11]. Restricting the physical availability of ‘off-premise’ stores (i.e. stores selling take-away alcohol for off-premise consumption) is considered one of the most effective population-level interventions to reduce alcohol-related harms [11-13]. However, there continue to be knowledge gaps in understanding the relationship between alcohol retail access and harms, limiting these policies’ public health benefits and uptake. One key gap is whether harms from increased alcohol retail access differ across population groups.
Direct and indirect harms from alcohol are well established to occur disproportionately in specific populations [14-20]. Some of these inequities may be created or exacerbated by alcohol control policies. For example, a growing evidence base suggests that alcohol pricing policies may have distinct impacts by sex and gender [21, 22]. Similarly, alcohol outlet access is known to be disproportionately high in low-income neighbourhoods, which may contribute to socio-economic inequities in alcohol-attributable harm [23-26]. Despite the potential for the alcohol retail environment to contribute to inequities in alcohol use and related harms, to our knowledge only a single study examined whether alcohol retail access has a differential impact based on the patterns of alcohol use, including disordered alcohol use [27]. One possibility is that individuals with current or past heavy or disordered patterns of alcohol use may have increased susceptibility to exposure to alcohol retail stores, which may trigger episodes of return to use or make reducing use more difficult [27]. In contrast, individuals with less heavy patterns of drinking may be more influenced by marginal changes in ease of accessing alcohol for consumption and risk of progressing to heavier patterns of drinking. A clearer understanding of potential differences in the association between alcohol availability can guide clinical and policy preventive efforts to reduce disordered drinking and health inequities.
In this study, we examined the association between alcohol retail access and health-care visits attributable to alcohol [including emergency department (ED) visits and outpatient care] and whether this association differed for individuals with and without a history of health-care attributable to alcohol. This was accomplished by linking population-based health administrative data to longitudinal data on the alcohol retail environment in Ontario, Canada. We hypothesized that the association between increased alcohol-retail access and health service use for alcohol will be stronger for individuals with prior alcohol-attributable health-care use (AAHU) than for the general population.
METHODS
Study design and population
We used a repeated cross-sectional population-level analysis of alcohol-attributable health service use in Ontario, Canada, between 2013 and 2019. The primary unit of analysis was the forward sortation area (FSA), a geographic designation based on the first three digits of the postal code (n = 513 FSAs in Ontario in 2016 and n = 520 in 2021). The exposure (off-premise alcohol availability) and outcomes (rates of alcohol-attributable ED and outpatient visits) were captured quarterly between January 2013 and December 2019. Rural FSAs were excluded from the analysis due to the known differences in the association between alcohol availability and alcohol use between rural and urban areas and privacy requirements [28]. Urban FSAs were defined as those with a statistical area classification of 1 (census metropolitan area), 2 (large census agglomeration) and 3 (smaller census agglomeration), as per the guidelines from Statistics Canada [29]. These represent FSAs in cities with a population larger than 100 000 people. Our study protocol and hypothesis were on the Open Science Framework (OSF, https://osf.io/y23f8).
Data sources
Alcohol retail environment
We obtained and validated the addresses of all off-premise alcohol outlets operating in Ontario for each year between 2013 and 2020. We included government-operated stores which sell beer, spirits and wine [Liquor Control Board of Ontario (LCBO) stores], privately operated beer stores which have a government issue monopoly to sell 12 and 24 packs of beer (the Beer Store), privately operated wine stores (the Wine Rack and the Wine Store) and privately operated grocery stores selling beer, wine and cider. We did not include privately operated LCBO agency stores, which sell beer wine and spirits in rural settings, as our study did not include rural FSAs. The primary source of these data is the Alcohol and Gaming Commission of Ontario, who is the Government regulator which issues licenses to sell off-premise alcohol and data were obtained and validated using previously described methods [23]. We did not have access to longitudinal data on on-premise locations. We obtained data on the location of bars and clubs in Ontario in 2019 from the Enhanced Points of Interest file (DMTI Spatial) for use in a sensitivity analysis.
Alcohol-attributable health service use
We obtained ED and outpatient visits attributable to alcohol for all individuals aged 10–105 years using comprehensive health administrative databases held at ICES (formerly the Institute for Clinical Evaluative Science). We used data from 2011 to 2019 (to allow a 2-year look-back from the first year of the study). ICES databases contain health service use information for all Ontarians with health-care coverage through the Ontario Health Insurance Plan (OHIP), which represents virtually all residents of the province (see Supporting information, Appendix S1 for a detailed list of ICES data sets used in this study). The use of the data in this project is authorized under section 45 of Ontario's Personal Health Information Protection Act (PHIPA) and does not require review by a Research Ethics Board. ICES requires that exported data, which include small cells (one to five events), be suppressed.
Exposure
Alcohol retail access
The primary retail access exposure was the average FSA-level availability of off-premise alcohol outlets, defined using a previously described spatial access index (SAI) [30]. SAI scores measured the average drive time between a population centre and the closest off-premise alcohol outlets on the road network. We calculated SAI scores for all dissemination areas (DAs, ‘neighbourhoods’) in Ontario. DAs are the smallest geographic unit (n = 400–700 individuals) for which census data are available in Canada. We then created a population-weighted average SAI score for all DAs within an FSA using a previously described technique [31, 32]. The population weighted-average SAI score for each FSA was re-calculated for each quarter between January 2013 and December 2019 to capture changes in access over time. Our primary SAI score was for the seven closest alcohol outlets. As a sensitivity analysis, we also recalculated the SAI score using the average drive time to the nearest three and five alcohol outlets, as we have conducted in previous studies using the SAI score [30, 32]. We calculated SAI scores for the seven closest on-premise alcohol outlets in 2019. These SAI scores were only included in a sensitivity analysis for 2019 to examine whether including on-premise access would modify the observed associations for off-premise stores.
Prior alcohol-attributable health-care status
AAHU captures a spectrum of alcohol-related concerns, including individuals with binge drinking, heavy patterns of alcohol use and alcohol use disorders (AUDs).
Outcomes
Alcohol-attributable ED visits were identified in the National Ambulatory Care Reporting System (NACRS) database using the International Classification of Disease—10th edition (ICD-10) codes outlined in the previously described Canadian Institute for Health Information (CIHI) [33]; see Supporting information, Appendix S2 for detailed codes. Alcohol-attributable outpatient visits were identified in the OHIP Claims Database using the ICD-9 codes ‘alcohol psychosis (291)’ or ‘alcoholism (303)’, as this database uses the ICD-9 coding system. The primary outcomes were (a) the rate of alcohol-attributable ED visits and (b) the rate of outpatient visits for residents of each FSA by quarter between January 2013 and December 2019. We obtained overall and stratum-specific rates for our pre-specified subpopulations (e.g. those with and without AAHU).
Covariates
The following area-level covariates were included in the statistical models a priori, as they were identified as potential confounders based on our previous work on alcohol availability and alcohol-attributable health service use in Ontario [7, 15, 16, 23, 30, 34]. We used area-level variables, as individual-level data on income, education and ethnicity are not available at ICES. Covariates were neighbourhood median income, the proportion of individuals with post-secondary education (defined as more than a high school diploma), the proportion of individuals between the ages of 20–29 years, the proportion of females, the proportion of visible minorities and the proportion of immigrants.
Statistical analysis
We calculated and presented descriptive statistics of alcohol availability (SAI score) and alcohol-attributable health service use over the study time-frame (Q1, 2013–Q4, 2019). We reported mean alcohol-attributable outpatient and ED visit rates across deciles of the SAI score. We used a quintile-based imputation approach for suppressed cells [35]. Briefly, we ranked the mean outcome rate for each FSA-year combination with at least one suppressed quarter cell count. The FSA-year combinations were grouped into quintiles and assigned an integer value of 1 to 5. Any quarter with a suppressed cell count had their cell count imputed with a value equal to the assigned quintile integer value of the respective FSA year. Suppressed quarter cell counts that fell in FSA-years in the top 20% were assigned an imputed cell count of 5, those in the bottom 20% were assigned a cell count of 1, and so on. Crude rates were then re-calculated using the imputed cell counts and populations at risk.
The associations between FSA-level SAI score deciles rates of alcohol-attributable outpatient and ED visits were modelled using mixed effects linear regression models. We included an indicator for each FSA as a random intercept term and a quarterly indicator for time as a random linear slope within each FSA. This model allowed each FSA to have its own FSA-specific deviation from the overall intercept and its own FSA-specific deviation from the overall linear outcome slope. We log-transformed the rates of our outcomes and exponentiated coefficients, which allowed the interpretation of the coefficients as relative changes. We completed separate models using two specifications for the SAI score deciles: (1) a continuous variable (assuming a linear relationship across deciles) and (2) a categorical decile-based approach where the first decile was the referent. The models were additionally adjusted for all mean-centred covariates listed in the Covariates section above as well as a linear trend in time (year–quarter) as an overall fixed effect. The population at risk in each FSA (during each quarter) was used as the denominator for the FSA-level rates of alcohol-attributable outpatient and ED visits. We completed analyses overall and stratified into those with AAHU and those with no history of AAHU to investigate potential effect modification.
RESULTS
Our study included 464 unique FSAs followed over 28 quarters. In each year, there were more than 10 million individuals included (n = 10 677 604 in 2013). The socio-demographic characteristics of FSAs by level of alcohol access in the first and last year of the study are presented in Table 1. Relative to FSAs in the lowest decile of alcohol access, FSAs in the highest decile of alcohol access were more likely to be in urban centres, have a higher proportion of immigrants, have a higher median income and have a higher proportion of individuals aged 20–29 years. The proportion of the population with prior AAHU remained consistent throughout the study period at 1.8%. During the study period there was a 16% overall increase in SAI scores (0.25 in 2013 to 0.29 in 2019).
| 2013 | 2019 | |||||
|---|---|---|---|---|---|---|
| FSAs lowest decile SAI access | FSAs highest SAI decile access | Whole population | FSAs lowest SAI decile access | FSAs highest SAI decile access | Whole population | |
| Total population | 615 819 | 958 278 | 10 677 604 | 615 926 | 1 096 226 | 11 500 314 |
| History of prior alcohol-attributable health-care use (AAHU)a | ||||||
| Proportion of people prior AAHU | 1.7 | 2.5 | 1.8 | 1.9 | 2.5 | 1.8 |
| Proportion of people no prior AAHU | 98.3 | 97.5 | 98.2 | 98.1 | 97.5 | 98.2 |
| Socio-demographic characteristics | ||||||
| % Female | 50.1 | 50.9 | 51.2 | 50.1 | 51.1 | 51.2 |
| % Aged 20–29 years | 10.4 | 20.2 | 13.3 | 10.4 | 20.2 | 13.3 |
| % Immigrant | 8.1 | 31.2 | 26.6 | 7.7 | 32.1 | 26.6 |
| % With less than high school education | 50.0 | 30.3 | 44.3 | 50.0 | 30.1 | 44.3 |
| % Visible minority | 2.9 | 32.4 | 25.5 | 2.5 | 36.6 | 25.5 |
| % Living in large urban centre (SAC 1) | 52.2 | 100 | 86.4 | 50 | 100 | 86.4 |
| % Living in mid-sized urban centre (SAC 2) | 6.5 | 0 | 3.0 | 6.5 | 0 | 3.0 |
| % Living in small urban centre (SAC 3) | 41.3 | 0 | 10.6 | 43.5 | 0 | 10.6 |
| Median income ($CAD) | 36 362 | 42 861 | 36 813 | 35 726 | 42 598 | 36 813 |
| Population density | 35.32 | 7007.29 | 1902.02 | 29.57 | 7886.34 | 2072.63 |
| Alcohol access variables (SAI score) | ||||||
| All stores selling alcohol | 0.07 | 0.67 | 0.25 | 0.08 | 0.73 | 0.29 |
| % of alcohol stores that sell Wine only | 0.07 | 0.33 | 0.23 | 0.04 | 0.32 | 0.16 |
- AAHU = alcoho-attributable health-care use; SAI = spatial access index.
- a Alcohol-attributable health-care use: individuals with one or more alcohol-attributable health service encounters (outpatient visits, ED visits or hospitalizations) in the 2 years before the quarter being evaluated. individuals with one or more alcohol-related acute health service encounters [emergency department (ED) visits or hospitalizations] in the 2 years prior to the quarter being evaluated.
Overall effect
Between 2013 and 2019, there were a total of 437 707 alcohol-attributable ED visits and 505 271 alcohol-attributable outpatient visits (Table 2). Observed ED visits and outpatient visits attributable to alcohol increased by 25.0 and 12.4%, respectively, between 2013 and 2019. Individuals with AAHU incurred 290 880 (66.5%) of ED visits attributable to alcohol and 369 006 (73.0%) of outpatient visits attributable to alcohol. FSAs in the highest decile of alcohol retail access (D10) had a higher absolute number and rate of both ED visits and outpatient compared to those in the lowest level of access (D1); see Table 2 for crude rates and Table 3 for adjusted relative differences. The rate of ED visits per 100 000 individuals aged 10 years and above in D1 was 111.84, while in D10 it was 273.48. After adjustment, each 10% increase in alcohol retail access was associated with a 4% relative increase in ED visits attributable to alcohol, with a relative difference in D10 relative to D1 of 1.39 (95% CI = 1.20–1.61). See Supporting information, Appendix S3 for models with alcohol retail access deciles treated as a linear variable. The crude rate of outpatient attributable to alcohol per 100 000 individuals in D1 was 124.31, while in D10 it was 322.29. After adjustment each 10% increase in alcohol retail access was associated with a 3% relative increase in outpatient visits attributable to alcohol, with a relative difference in D10 relative to D1 of 1.49 (95% CI = 1.26–1.75). A sensitivity analysis using alternative SAI scores based on the closest three and five alcohol retail stores showed a consistent direction of association (see Supporting information, Appendix S4). Similarly, a sensitivity analysis including a SAI score for the closest seven on-premise stores showed consistent associations between off-premise store access and harms (see Supporting information, Appendix S5).
| Overall | No prior AAHUa | Prior AAHU | ||||
|---|---|---|---|---|---|---|
| Count of events | Rate per 100 000 person-years | Count of events | Rate per 100 000 person-years | Count of events | Rate per 100 000 person-years | |
| Entire study (2013–19) | ||||||
| ED visits | 437 707 | 140.67 | 142 717 | 46.69 | 290 880 | 5276.69 |
| Outpatient visits | 505 271 | 162.39 | 132 853 | 43.47 | 369 006 | 6693.93 |
| ED annual visits | ||||||
| D1 study average | 2782 | 111.84 | 1077 | 43.62 | 1591 | 3639.01 |
| D10 study average | 11 077 | 273.48 | 2373 | 60.13 | 8658 | 8429.76 |
| Outpatient annual visits | ||||||
| D1 study average | 3103 | 124.31 | 991 | 40.72 | 2031 | 4580.30 |
| D10 study average | 13 078 | 322.29 | 2599 | 65.46 | 10 456 | 10 174.85 |
- D1 is the lowest decile of alcohol access. D10 is the highest decile of alcohol.
- AAHU = alcohol-attributable health-care use.
- a Alcohol-attributable health-care use: individuals with one or more alcohol-attributable health service encounters (ED visits or hospitalizations) in the 2 years prior to the quarter being evaluated.
| Outpatient visits | ED visits | |||||
|---|---|---|---|---|---|---|
| Overall | Prior AAHUa | No prior AAHU | Overall | Prior AAHU | No prior AAHU | |
| Relative change (95% CI) | ||||||
| Alcohol retail access | ||||||
| SAI off-premise decileb | ||||||
| 1 | Ref | Ref | Ref | Ref | Ref | Ref |
| 2 | 1.06 (0.97–1.15) | 0.96 (0.88–1.06) | 1.18 (1.08–1.29) | 1.04 (0.97–1.12) | 1.09 (0.99–1.19) | 1.06 (0.99–1.14) |
| 3 | 1.11 (1.00–1.22) | 1.00 (0.90–1.11) | 1.22 (1.10–1.35) | 1.07 (0.98–1.17) | 1.10 (0.99–1.22) | 1.06 (0.98–1.15) |
| 4 | 1.15 (1.03–1.28) | 0.97 (0.86–1.09) | 1.26 (1.12–1.41) | 1.10 (1.00–1.22) | 1.11 (0.98–1.24) | 1.10 (1.01–1.20) |
| 5 | 1.21 (1.08–1.36) | 1.01 (0.89–1.14) | 1.24 (1.10–1.39) | 1.18 (1.07–1.30) | 1.16 (1.03–1.30) | 1.16 (1.06–1.27) |
| 6 | 1.26 (1.12–1.41) | 1.01 (0.89–1.15) | 1.31 (1.17–1.48) | 1.19 (1.07–1.32) | 1.16 (1.03–1.32) | 1.20 (1.09–1.32) |
| 7 | 1.29 (1.15–1.46) | 1.04 (0.91–1.18) | 1.33 (1.18–1.50) | 1.24 (1.11–1.38) | 1.24 (1.09–1.41) | 1.21 (1.10–1.33) |
| 8 | 1.29 (1.14–1.46) | 1.02 (0.89–1.17) | 1.33 (1.17–1.50) | 1.25 (1.12–1.40) | 1.26 (1.10–1.43) | 1.22 (1.10–1.34) |
| 9 | 1.35 (1.19–1.54) | 1.04 (0.90–1.20) | 1.42 (1.25–1.62) | 1.30 (1.15–1.46) | 1.32 (1.15–1.52) | 1.26 (1.13–1.39) |
| 10 | 1.49 (1.26–1.75) | 1.08 (0.90–1.30) | 1.65 (1.39–1.95) | 1.39 (1.20–1.61) | 1.47 (1.23–1.75) | 1.30 (1.14–1.48) |
| Covariatesc | ||||||
| Proportion wine store | 1.02 (1.01–1.03) | 1.02 (1.01–1.03) | 1.02 (1.01–1.03) | 1.01 (1.01–1.02) | 1.00 (0.99–1.01) | 1.02 (1.01–1.03) |
| Year (linear) | 1.00 (1.00–1.01) | 1.00 (1.00–1.00) | 1.01 (1.00–1.01) | 1.01 (1.01–1.01) | 1.01 (1.01–1.01) | 1.00 (1.00–1.00) |
| Median incomed | 1.00 (0.99–1.01) | 1.00 (1.00–1.01) | 1.00 (0.99–1.01) | 0.98 (0.97–0.99) | 0.99 (0.98–1.00) | 0.98 (0.98–0.99) |
| % Immigrant | 1.02 (0.98–1.06) | 1.05 (1.01–1.09) | 1.01 (0.97–1.04) | 0.99 (0.95–1.03) | 1.02 (0.98–1.06) | 0.98 (0.95–1.01) |
| % less than high school diploma | 0.95 (0.91–0.99) | 0.90 (0.87–0.94) | 1.00 (0.96–1.03) | 1.02 (0.98–1.07) | 1.01 (0.96–1.05) | 1.00 (0.97–1.03) |
| % Visible minority | 0.94 (0.91–0.97) | 0.98 (0.96–1.01) | 0.94 (0.92–0.96) | 0.94 (0.92–0.97) | 0.98 (0.95–1.01) | 0.95 (0.93–0.97) |
| % Aged 20–29 years | 1.08 (1.01–1.15) | 0.94 (0.88–1.01) | 1.03 (0.97–1.09) | 1.25 (1.17–1.34) | 1.11 (1.03–1.19) | 1.16 (1.10–1.21) |
| % Female | 1.12 (0.96–1.29) | 1.05 (0.91–1.22) | 0.75 (0.66–0.85) | 1.00 (0.86–1.16) | 0.85 (0.72–1.00) | 0.78 (0.70–0.87) |
| Population density | 1.05 (1.03–1.07) | 1.02 (1.00–1.04) | 1.02 (1.01–1.04) | 1.05 (1.03–1.07) | 1.03 (1.01–1.05) | 0.99 (0.98–1.01) |
| % In large urban centre | 1.12 (0.97–1.29) | 1.13 (0.98–1.30) | 1.10 (0.97–1.24) | 1.05 (0.90–1.23) | 0.98 (0.84–1.15) | 1.01 (0.90–1.12) |
| % In mid-sized urban centre | 0.93 (0.72–1.20) | 1.04 (0.81–1.33) | 1.00 (0.81–1.24) | 1.05 (0.80–1.38) | 1.14 (0.86–1.50) | 1.05 (0.87–1.27) |
| % In small urban centre | Ref | Ref | Ref | Ref | Ref | Ref |
- AAHU = alcohol-attributable health-care use. SAI = spatial access index.
- a Alcohol-attributable health-care use: individuals with one or morealcohol-attributable health service encounters (ED visits or hospitalizations) in the 2 years prior to the quarter being evaluated.
- b Spatial access index: the population weighted average of the drive time between the centroid of each neighbourhood in a forward sortation area (FSA) and its seven closest off-premises alcohol outlets.
- c Effect estimate per 5% change in covariates that are a proportion.
- d Effect estimate per $1000 change in median income.
Figure 1 illustrates the relative differences in rates of alcohol-attributable ED visits and outpatient visits, categorized across deciles of alcohol retail store access. There was a dose–response relationship between increasing deciles of SAI scores and increases in both ED visits and outpatient visits attributable to alcohol in the overall population. When examining the data by AAHU status, a similar trend was observed for ED visits among the AHHU and non-AAHU groups. However, different trends emerged for outpatient visits. As SAI access increased there was an increase in outpatient visits among those without a history of AAHU, but not among those with a history of AAHU.
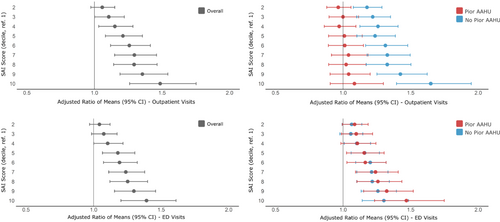
Effect by AAHU status
Throughout the entire study and for all levels of alcohol access the crude rates of alcohol-attributable health service use between those with AAHU versus those without were 112.94-fold higher for ED visits (5276.69 versus 46.69) and 154.01-fold higher for outpatient visits (6693.93 versus 43.47). For individuals with AAHU the adjusted relative difference in rates of ED visits attributable to alcohol per 100 000 individuals between D1 (3638.01) and D10 (8429.76) was 1.47 (95% CI = 1.23–1.75). For individuals without AAHU the adjusted relative difference in rates per 100 000 individuals between D1 (43.62) and D10 (60.13) was 1.30 (95% CI = 1.14–1.48). There was no difference in the association between alcohol access and rates of ED visits attributable to alcohol for individuals with and without an AAHU. For individuals with AAHU the adjusted relative difference in rates of outpatient visits attributable to alcohol per 100 000 individuals between D1 (4580.30) and D10 (10174.85) was 1.08 (95% CI = 0.90–1.30). For individuals without AAHU the adjusted relative difference in rates per 100 000 individuals between D1 (40.72) and D10 (65.46) was 1.65 (95% CI = 1.39–1.95).
DISCUSSION
In this population-based analysis of alcohol-attributable health service use in Ontario, Canada, we found that greater off-premise alcohol retail access was associated with higher rates of alcohol-attributable outpatient and ED visits. Each 10% increase in alcohol retail access was associated with a 4% higher rate of outpatient and a 3% higher rate of ED visits attributable to alcohol. Individuals with alcohol-attributable health-care visits in the past 2 years accounted for almost two-thirds of total alcohol-attributable outpatient and ED visits, despite representing fewer than 2% of the overall population. There was no difference in the positive association between alcohol availability and rates of alcohol-attributable ED visits between individuals with and without previous alcohol-attributable health-care. However, increasing alcohol availability was only associated with higher rates of alcohol-attributable outpatient visits among those without previous alcohol-attributable health-care.
Our results showing a positive association between greater alcohol availability and increased alcohol-attributable health-care visits are consistent with a large body of evidence finding that off-premise alcohol store density is associated with increased alcohol consumption and related harms. Multiple reviews have supported this association [36-38] and the causal nature of the relationship continues to be uncertain (i.e. whether opening more alcohol outlets encourages heavier drinking in the local population or vice versa) [31, 32, 39]. The association between alcohol availability and alcohol-attributable ED visits was similar between groups with and without prior alcohol-attributable health-care visits, while the association between alcohol availability and rates of alcohol-attributable outpatient visits only existed in the general population, and not among individuals with prior alcohol-attributable health-care visits. These findings are consistent with the one prior study in the literature, which found that greater off-premise retail access was associated with an increased risk of developing an AUD but not for the risk of recurrence for individuals with past AUD histories [27]. Collectively, the findings suggest that individuals without disordered drinking patterns may be more likely to be harmed by increases in local alcohol availability. One reason for this finding could be that, due to motivations such as craving and withdrawal avoidance, individuals with current disordered patterns of drinking may have alcohol purchase patterns that are less influenced by retail availability (e.g. stockpiling, greater willingness to travel to obtain alcohol). In contrast, individuals without disordered drinking patterns may display a greater susceptibility to alcohol availability through cues to purchase and reduced barriers to obtaining alcohol. This is consistent with studies finding that physical alcohol advertising and point-of-sale promotions in retail stores can induce alcohol purchasing and consumption [40, 41].
There are alternative explanations for the observed null association between alcohol availability and alcohol-attributable outpatient visits among individuals with prior alcohol visits. Outpatient alcohol-attributable visits in individuals with a history of health-care attributable to alcohol capture a wide variety of alcohol-related presentations, ranging from the therapeutic management of an existing alcohol-related problem in remission to a return to a new disorder due to alcohol use. Consequently, our findings do not rule out the possibility that increased alcohol availability may increase the risk of some types of harms (e.g. a return to use in someone with a past history of disordered patterns of alcohol use) while not increasing the risk of others (e.g. frequency of outpatient care for someone with current heavy daily drinking, or preventive visits for prescription of anticraving medications).
Overall, these results demonstrate an association between increasing alcohol availability and higher rates of alcohol-attributable harms in populations with and without a history of alcohol-attributable health-care visits. This supports that reducing alcohol availability would be an effective public health strategy for reducing population-level rates of alcohol-attributable harm. Differences in the association between alcohol availability and rates of alcohol-attributable outpatient visits between those with and without prior alcohol-attributable health care may be capturing an important causal effect of alcohol environments. Additional research is indicated to understand these complexities and potentially target policies more effectively to minimize the risk of alcohol-attributable harm.
Limitations
Our study has important limitations. First, while the use of health administrative data allowed us to examine objective population-level outcomes, it does not provide data on patterns of drinking and whether or not individuals have an AUD. While prior research has found that the majority of individuals with a previous alcohol-attributable health-care visit have heavy or disordered drinking, we did not directly capture AUD [42]. In addition, individuals with disordered drinking but have not had a recent alcohol-attributable health service encounter are considered part of the general population. Secondly, our study cannot distinguish individuals with former disordered drinking from those with more active conditions. It is plausible that individuals in the early stages of recovery may exhibit a higher susceptibility to changes in alcohol access, while such variations may be less influential in those with more active drinking. Further research is necessary to explore these distinctions and more clearly understand the relationship between drinking level, recovery stages and responsiveness to changes in alcohol availability. Thirdly, our study captured visits wholly attributable to alcohol, which only represent an estimated 25–40% of total health-care visits which may be caused by alcohol (e.g. cardiovascular and respiratory conditions or cancers partially attributable to alcohol use) [43]. Further research examining the effect of alcohol access for individuals with differing patterns of alcohol use is indicated.
CONCLUSION
Consistent with the literature, this study showed that greater off-premise retail alcohol access is associated with greater rates of ED and outpatient visits attributable to alcohol. This study highlights potential differences in this association for individuals with and without prior care attributable to alcohol. Further research utilizing diverse study designs should be conducted to more clearly understand these observations.
AUTHOR CONTRIBUTIONS
Daniel T. Myran: Conceptualization (equal); data curation (equal); funding acquisition (equal); investigation (equal); methodology (equal); project administration (equal); supervision (lead); validation (equal); visualization (supporting); writing—original draft (equal); writing—review and editing (equal). Erik Friesen: Conceptualization (equal); data curation (equal); funding acquisition (equal); investigation (equal); methodology (equal); project administration (equal); writing—original draft (equal); writing—review and editing (equal). Robert Talarico: Conceptualization (equal); data curation (equal); formal analysis (lead); funding acquisition (equal); investigation (equal); methodology (equal); software (lead); validation (equal); visualization (lead); writing—original draft (equal); writing—review and editing (equal). Adrienne Gaudreault: Conceptualization (equal); data curation (equal); investigation (equal); methodology (equal); project administration (equal); writing—original draft; writing—review and editing (equal). Monica Taljaard: Conceptualization (equal); data curation (equal); funding acquisition (equal); investigation (equal); methodology (equal); writing—review and editing (equal). Erin Hobin: Conceptualization (equal); data curation (equal); funding acquisition (equal); investigation (equal); methodology (equal); writing—review and editing (equal). Brendan Smith: Conceptualization (equal); data curation (equal); investigation (equal); methodology (equal); writing—review and editing (equal). Naomi Schwartz: Conceptualization (equal); data curation (equal); funding acquisition (equal); investigation (equal); methodology (equal); writing—review and editing (equal). Norman Giesbrecht: Conceptualization (equal); data curation (equal); funding acquisition (equal); investigation (equal); methodology (equal); writing—review and editing (equal). Jean-François Crépault: Conceptualization (equal); data curation (equal); funding acquisition (equal); investigation; methodology (equal); writing—review and editing (equal). Peter Tanuseputro: Conceptualization (equal); data curation (equal); funding acquisition (equal); investigation (equal); methodology (equal); writing—review and editing (equal). Douglas Manuel: Conceptualization (equal); data curation (equal); funding acquisition (equal); investigation (equal); methodology (equal); writing—review and editing (equal).
ACKNOWLEDGEMENTS
Parts of this material are based on data and/or information compiled and provided by CIHI, and the Ontario Ministry of Health. The analyses, conclusions, opinions and statements expressed herein are solely those of the authors and do not reflect those of the funding or data sources; no endorsement is intended or should be inferred. The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and the decision to submit the manuscript for publication.
DECLARATION OF INTERESTS
None to disclose.
Open Research
DATA AVAILABILITY STATEMENT
The dataset from this study is held securely in coded form at ICES. While legal data sharing agreements between ICES and data providers (e.g. healthcare organizations and government) prohibit ICES from making the dataset publicly available, access may be granted to those who meet pre-specified criteria for confidential access, available at www.ices.on.ca/DAS (email: [email protected]). The full dataset creation plan and underlying analytic code are available from the authors upon request, understanding that the computer programs may rely upon coding templates or macros that are unique to ICES and are therefore either inaccessible or may require modification.