Age–period–cohort analysis of trends in tobacco smoking, cannabis use, and their co-use in the Australian population
Funding information: None.
Abstract
Background and aim
The prevalence of tobacco smoking has declined in most high-income countries, while cannabis use has been rising. Moreover, cannabis use has been found to have increased among cigarette smokers in recent years in jurisdictions where it has been either decriminalized or legalized. This study measured trends in cannabis, tobacco and the co-use of cannabis and tobacco in Australia.
Design
Age–period–cohort analysis.
Setting and participants
Participants were n = 143 344 individuals aged 18–80 years who participated in Australia's National Drug Strategy Household Surveys (NDSHS) between 2001 and 2019.
Measurements
Regular (weekly/more frequently): (1) tobacco smoking only, (2) cannabis use only and (3) the co-use of cannabis and tobacco.
Findings
Prevalence of only smoking tobacco decreased in all age groups (P < 0.001) and birth cohorts between 2001 and 2019, but the co-use of cannabis and tobacco did not. Younger cohorts were much less likely to co-use tobacco and cannabis (P = 0.02). Period trends showed that both cannabis use only and the co-use of cannabis and tobacco have increased since 2013.
Conclusion
There has been a consistent decrease in exclusive tobacco smoking across age, period and birth cohorts between 2001 and 2019 in Australia, although there is a recent increasing period trend in cannabis use with or without tobacco. The non-decreasing trend of co-use may reflect the strong tobacco control policies introduced over the period and changing attitudes towards cannabis use in Australia.
INTRODUCTION
Tobacco use is a leading risk factor for burden of diseases and is responsible for 8.7 million deaths globally [1]. More than 85% of the disease burden caused by tobacco use is from smoking. In Australia, 12.2% of people aged 14 years or above smoke tobacco daily [2]. In 2018, 8.6% of the disease burden in Australia was due to tobacco use, making it the leading risk factor that contributed to disease burden and deaths [3].
Cigarette smoking has declined in developed countries during the last several decades [4]. By contrast, the global number of past-year cannabis users increased by 18% between 2010 and 2019, partly owing to the liberalization of cannabis policies and public attitudes in many countries, including the legalization of recreational use in Canada, 18 US states and Uruguay. Many other countries have legalized medical use of cannabis [5].
Tobacco and cannabis are often used concurrently [6]. Some evidence suggests that co-use of both tobacco and cannabis has increased among cigarette smokers in recent years in jurisdictions where it has been legalized [7-10]. There is evidence of increased toxicant exposure among people who co-use cannabis and tobacco [11, 12]. Tobacco and cannabis are often smoked and one could serve as a cue for the other substance, so cannabis smoking could reduce the success of tobacco cessation [13-17]. Further, nicotine and delta-9-tetrahydrocannabinol (the key psychoactive ingredient of cannabis) may produce synergistically rewarding effects (e.g. greater than the effects of using each substance alone) [18].
In the last two decades there have been radical divergences in cannabis and tobacco policies [19]. On one hand, more than 180 countries are now signatories of the World Health Organization Framework Convention on Tobacco Control (WHO FCTC), the first global treaty that aims to end the tobacco epidemic [20]. On the other hand, there had been a strong movement towards liberalizing cannabis use in various forms, predominantly smoking. Despite being banned globally under the United Nations (UN) Convention of Narcotic Drugs, several nations have legalized recreational cannabis (e.g. Uruguay and Canada) and other countries (e.g. the Netherlands) have decriminalized it [21].
Australia has implemented several of the recommended policies of the WHO FCTC and has one of the lowest smoking rates in the world [1]. In the case of cannabis, Australian policy has become more liberal with the legalization of medical cannabis use in 2016 [22]. The Australian Capital Territory (one of the eight states/territories of Australia) has removed all penalties for private recreational cannabis use in 2020 [23].
The 2019 Australian National Drug Strategy Household Survey (NDSHS) showed that 11.6% of the population aged 14 years and older had used cannabis in the past 12 months [2]. There is some evidence that the co-use of cannabis is higher in some countries that have liberalized cannabis [24]; less is known about trends in Australia.
There are currently no published and recent data on the prevalence of cannabis use and co-use with tobacco in Australia. This study examined the age, period and cohort trends of cannabis, tobacco and co-use in Australia using data from a series of large, nationally representative adult samples. Age–period–cohort analysis can provide a better understanding of how age groups, birth cohorts and periods distinctly contribute to trends [25]. Age effects refer to the variation associated with chronological age, which reflects changes due to biological and social processes of ageing. Cohort effects refer to the variations among individuals from different birth cohorts, who move through life and have experienced the same historical events at similar ages. Period effects refer to variations between periods across time that affect all age groups. Delineating cohort and period effects has paramount policy implications. If a trend is largely driven by a cohort effect, policies that target the affected cohorts might be more effective to interrupt a trend, whereas a trend underpinned by a period effect may be better targeted using a population approach.
METHODS
Data source, study design and procedure
Data for this age–period–cohort study were from the National Drug Strategy Household Surveys (NDSHS) [26] conducted in 2001, 2004, 2007, 2010, 2013, 2016 and 2019. The NDSHS is the largest nationally representative drug use cross-sectional survey in Australia that is conducted every 3 years under the governance of the Australian Institute of Health and Welfare. The NDSHS is conducted in all Australian states and territories, with a sampling frame designed to be representative of the Australian population aged 14 years and above living in a household setting. Detailed descriptions of the sample characteristics and collection procedures can be found elsewhere [26]. Access to the survey data by the National Centre for Youth Substance Use Research was approved by the Australian Data Archive and by The University of Queensland Human Research Ethics Committee.
Study sample
This study focused on individuals who were aged between 18 and 80 years. Participants aged 14–17 years were excluded because of the small sample sizes in each survey and because the legal age for tobacco purchase is 18 years in Australia. There were approximately 20 000 participants in each survey year (range = 19 228–22 952). The total sample size for this study was 143 344 (mean age = 45.8, SD = 15.5; 56% female; 2.4% Indigenous). The average response rates were approximately 50% (range = 46–51%), which is comparable to other Australian and international surveys of alcohol and drug use [27, 28].
Measures
The outcome variables were regular tobacco use only, cannabis use only and the co-use of cannabis and tobacco. In each case, the response was coded as yes/no based on whether the person reported weekly use or more frequent use in the past year. Reports of at least weekly use of both cannabis and tobacco were classified as co-use. At least weekly use of cannabis was the focus because health harms are associated with frequent use.
The predictor variables were age (continuous), period (survey year) and cohort (birth cohort). Participants were grouped into six birth cohorts: 1936–50, 1951–60, 1961–70, 1971–80, 1981–90 and 1991–2001. There were seven periods: 2001, 2004, 2007, 2010, 2013, 2016 and 2019.
Gender, remoteness (living in a major city, inner regional area or outer regional area), education (finished high school: yes/no) and states were used as covariates.
Analysis
Mixed-effect logistic regressions were used to model the effect of age, period and cohort on regular tobacco only, cannabis only and their co-use. To break the linear dependency between these three variables, age and its quadratic term were entered as fixed effects and the cohort and period terms were entered as random effects [25]. To test the cohort and period effect, likelihood ratio tests were used to compare models with and without these effects. We calculated model-based predicted probabilities of tobacco and cannabis use to facilitate the interpretation of the cohort and period effects. For the age effect, the probability was calculated for an ‘average’ cohort and ‘average’ period. The predicted probability for the period and cohort effects were calculated at 20 years of age. The patterns of period and cohort effects for other ages were the same on a logit scale. This method assumed that the long-term trends of variables entered as random-effects were zero.
To evaluate the robustness of the results, we conducted a sensitivity analysis by entering all age, period and cohort effects as fixed effects. In this analysis, the linear dependency between age, period and cohort was broken because age was modelled as a continuous variable, and cohort and period were grouped into 10- and 3-year intervals, respectively.
Analyses adjusted for, but did not stratify by gender, because the cell sizes were small (e.g. co-use among older cohort), leading to unstable estimates with large confidence intervals. In both sets of analyses, the effects of gender, remoteness (living in a major city, inner regional or outer regional area), education (finished high school: yes/no) and states were adjusted for in all models. The analysis was not pre-registered and the results should be considered exploratory. Main analyses were conducted using StatsNotebook [29] for R (version 4.0.3) [30]. The lme4 package [31] was used for mixed effect modelling and the emmeans package was used to calculate conditional predicted probabilities of tobacco, cannabis and co-use of the two substances. Sensitivity analyses were conducted in Stata version 14 [32].
RESULTS
Figure 1 shows the model-based predicted probabilities of exclusive tobacco smoking, exclusive cannabis use and co-use by age, period and birth cohort. Model parameters are shown in Supporting information, Table S1.
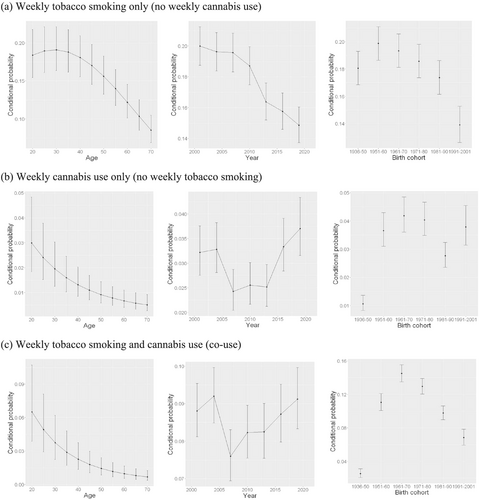
The age effect on exclusive tobacco smoking was non-linear [linear term: b = 0.08, standard error (SE) = 0.04, P = 0.021; quadratic term: b = −0.05, SE = 0.005, P < 0.001]. The probabilities remained stable for those between 20- and 30-year-olds and decreased afterwards. There was a significant period and birth cohort effect (P < 0.001). Probabilities of exclusive smoking decreased substantially between 2001 and 2019. The 1951–60 birth cohort has the highest probability of exclusive tobacco smoking, and this probability decreased in subsequent birth cohorts.
The age effect on exclusive cannabis use and co-use showed a similar pattern. Both peaked at early 20 and then decreased with age (P < 0.05; see Supporting information, Table S1 for model parameters). The period and cohort effects were highly statistically significant for both exclusive cannabis use and co-use. The period effects on exclusive cannabis use and co-use were similar—the conditional probability of exclusive cannabis use and co-use dipped in 2007, increased thereafter and peaked in 2019.
The cohort effects were qualitatively different. The 1936–50 birth cohort had the lowest probability of exclusive cannabis use and co-use. The probabilities increased substantially in the next birth cohort (1951–60). Probabilities of exclusive cannabis use remained high in most of the subsequent birth cohorts (except for the 1981–90 cohort). Probabilities of co-use were highest among the 1961–70 cohort and then decreased substantially among the younger cohorts. Findings from the sensitivity analyses were consistent, supporting the robustness of our results (see Supporting information, S2).
DISCUSSION
This study examined the age, period and cohort (APC) trends in cannabis, tobacco and the co-use of cannabis and tobacco in Australia between 2001 and 2019. We found that the prevalence of exclusive cigarette smoking decreased across age groups and birth cohort. Such a comprehensive decrease most probably reflects the implementation of strong tobacco control policies (e.g. increased taxes and price; smoke-free policies; health warnings and plain packaging; advertising bans; and public health educational campaigns), implemented during the period that increased prices and awareness of the harms of smoking cigarettes in Australia as has been experienced elsewhere, such as in New Zealand and Canada [33-35].
By contrast, there has not been any decline in the co-use of tobacco and cannabis between 2001 and 2019, despite a strong birth cohort effect showing that younger cohorts were much less likely to co-use. The co-use period trend is similar to the exclusive cannabis use period trend, which has shown an upward trajectory since 2013. A potential explanation could be that the co-use trend may be driven by cannabis use, regardless of tobacco use. Consistently, in the United Kingdom and United States, repeated cross-sectional data on tobacco and cannabis use had shown that cannabis use increased between 2013 and 2019, while tobacco smoking decreased, and that those who used cannabis were more likely to also smoke tobacco [9, 36].
Since 2013, Australians have become more accepting of cannabis use, with a sharp drop in the proportion of Australians who associate cannabis use as a ‘drug problem’ [22]. Previous analyses of the 2016 NDSHS survey have shown that 77% of Australians supported the legalization of cannabis for medical use and 40% supported its legalization for recreational use [22]. In 2017, Australia legalized medical cannabis use, and in 2020 the Australian Capital Territory was the first Australian jurisdiction to remove all penalties for recreational cannabis use [23]. These attitudinal trends have been accompanied by an increase in cannabis use, as evident in the exclusive cannabis use period trend.
The stable trend of co-use may reflect the combined effects of strong tobacco control policies and the liberalization of cannabis attitudes in Australia. There are potential synergistic effects of nicotine and cannabis, and co-use may reduce successful quitting of tobacco smoking. A recent systematic review and meta-analyses of 11 randomized clinical trials delivered to participants who co-used showed overall weak effectiveness on both cannabis [relative risk (RR) = 14.48, 0.92–2.49] and tobacco cessation (RR = 1.10, 0.68–1.87) [37]. Subgroup analyses of a smaller number of studies suggested some effectiveness of interventions that targeted the use of both substances, but only on cannabis cessation and reduction. Future research is warranted on effective cessation interventions that simultaneously addresses the quitting of both tobacco and cannabis use [7, 38].
Our findings are to be interpreted with some limitations. Cannabis use may be under-reported due to hesitancies in reporting the use of illicit substances. We used a national general household sample, but findings may differ in specific subpopulations. For example, there are health disparities by Indigenous status [39], but we did not have an adequate sample to analyse trends in this subgroup. Tobacco and cannabis are typically first used during adolescence, but our study excluded people aged under 18 years due to small sample sizes. Future research that draws upon youth-specific studies [e.g. Australian Secondary School Students Alcohol and Drug (ASSAD) survey], to provide an understanding of trends in co-use among adolescents, is warranted.
We had not examined results by route of administration because in Australia tobacco is predominantly smoked in cigarettes and the use of smokeless, chewing or vaping tobacco is extremely rare because policies limit their availability. Similarly, cannabis has been predominately smoked in Australia compared to Canada, where it is more common to also use vapes [24]. Future studies are warranted to monitor the use of tobacco and cannabis via vaping devices and the health impacts of their use by these more novel methods [40].
CONCLUSION
There has been a consistent decrease in exclusive tobacco smoking among age, period and birth cohorts between 2001 and 2019 in Australia. By contrast, there was an increasing period trend in exclusive cannabis use, and the probabilities of exclusive cannabis use among the birth cohorts as 1950 were similar, except for the 1981–90 cohort. The period trend of co-use was similar to that of exclusive cannabis use, despite a decreasing cohort trend since the 1961–70 cohort.
ACKNOWLEDGEMENTS
Open access publishing facilitated by The University of Queensland, as part of the Wiley - The University of Queensland agreement via the Council of Australian University Librarians. Open access publishing facilitated by The University of Queensland, as part of the Wiley - The University of Queensland agreement via the Council of Australian University Librarians.
DECLARATION OF INTERESTS
None.
AUTHOR CONTRIBUTIONS
Janni Leung: Conceptualization-Equal; Data curation-Equal; Project administration-Lead; Writing – original draft-Equal. Shannon Gravely: Conceptualization, Methodology; Investigation. Carmen Lim: Data curation-Equal; Formal analysis-Equal; Investigation-Equal; Writing – review & editing-Equal. Wayne Hall: Conceptualization; Methodology; Investigation. Gary Chan: Conceptualization-Equal; Data curation-Equal; Methodology-Equal; Writing – original draft-Equal.