Liver surface nodularity and ascites are associated with mortality risk in acute alcohol-associated hepatitis
Abstract
Background
Acute alcohol-associated hepatitis (AH) is associated with high mortality. CT-derived liver surface nodularity (LSN) is a robust prognostic biomarker in other chronic liver diseases. The aim of this study was to determine relationships between LSN, disease severity, and mortality in AH.
Methods
Adults hospitalized with AH from January 2016 to March 2020 were included if an abdominal CT was performed between 8 weeks prior to 72 h after hospitalization. LSN was measured using quantitative methods (Liver Surface Nodularity Software version 0.88, Birmingham, AL, USA). Cox proportional hazards models, logistic regression and AUROC analysis were used to examine relationships between LSN and 180-day transplant-free survival.
Results
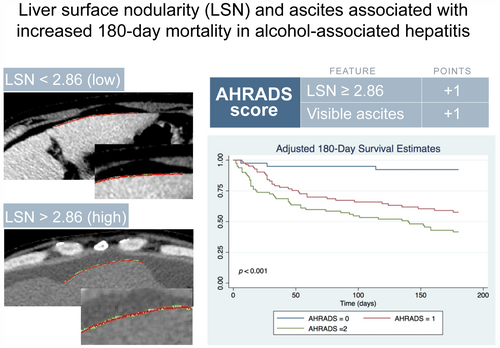
Of 386 patients hospitalized with AH during the study period, 230 had CT scans performed, and 205 met inclusion criteria. Mean transplant-free survival was 127 days (95% CI 118–137). Within each cohort, patients were grouped into low [LSN-LOW, N = 109 (53.2%)] and high [LSN-HIGH, N = 96 (46.8%)] LSN strata based on an optimal cutoff of 2.86 derived from unadjusted ROC curves. Patients with high LSN had features of portal hypertension, which included encephalopathy [53 (55.2%) vs. 43 (39.4%), p = 0.017], ascites on CT [81 (84.4%) vs. 69 (63.3%), p = 0.001] and portosystemic shunts [78 (81.2%) vs. 69 (63.3%), p = 0.003]. High LSN, ascites and MELD were independently associated with lower likelihood of 180-day transplant-free survival, and inclusion of a score assigning 1 point each for high LSN or ascites on CT (AHRADS score) to MELD enhanced diagnostic accuracy of AUROC for 180-day survival compared to MELD alone [AUROC 0.782 (95% CI 0.719–0.845) vs. 0.735 (0.667–0.802), p = 0.023].
Conclusions
CT-derived factors that include LSN and ascites are radiographic biomarkers associated with 180-day transplant-free survival in alcohol-associated hepatitis.
Graphical Abstract
This study assesses the utility of CT-derived biomarkers for outcome prediction in alcohol-associated hepatitis (AH). A radiographic score (AHRADS) including 1) semi-automated assessment of liver surface nodularity (LSN) from CT scans and 2) visible ascites on imaging were associated with increased risk of death at 180 days in patients with AH. Addition of AHRADS to the well-validated laboratory MELD Score improves model performance. This study highlights the utility of imaging-based biomarkers for both survival prediction and treatment responses in AH.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no conflict of interest.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.