Who gets the ventilator? A multicentre survey of intensivists' opinions of triage during the first wave of the COVID-19 pandemic
Abstract
Background
The COVID-19 pandemic has caused a shortage of intensive care resources. Intensivists' opinion of triage and ventilator allocation during the COVID-19 pandemic is not well described.
Methods
This was a survey concerning patient numbers, bed capacity, triage guidelines, and three virtual cases involving ventilator allocations. Physicians from 400 ICUs in a research network were invited to participate. Preferences were assessed with a five-point Likert scale. Additionally, age, gender, work experience, geography, and religion were recorded.
Results
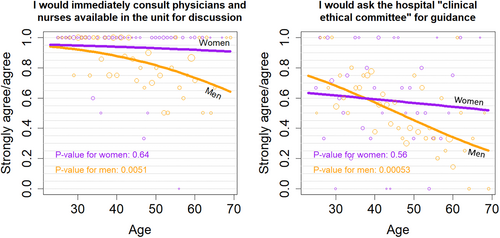
Of 437 responders 31% were female. The mean age was 44.4 (SD 11.1) with a mean ICU experience of 13.7 (SD 10.5) years. Respondents were mostly European (88%). Sixty-six percent had triage guidelines available. Younger patients and caretakers of children were favoured for ventilator allocation although this was less clear if this involved withdrawal of the ventilator from another patient. Decisions did not differ with ICU experience, gender, religion, or guideline availability. Consultation of colleagues or an ethical committee decreased with age and male gender.
Conclusion
Intensivists appeared to prioritise younger patients for ventilator allocation. The tendency to consult colleagues about triage decreased with age and male gender. Many found such tasks to be not purely medical and that authorities should assume responsibility for triage during resource scarcity.
Editorial Comment
This study reports the views of a large international cohort of front line intensivists about their approach to hypothetical triage scenarios in the setting of the COVID pandemic. Three out of four intensivists chose to allocate the last free ventilator to the youngest patient. This decision was similar across respondents' age, experience level religion, and triage guideline availability.
1 INTRODUCTION
The COVID-19 pandemic led to a surge in demand for intensive care in many countries. Initial reports from hospitals in Northern Italy spurred concerns of shortness of critical resources and the need to triage patients to criteria not usually utilised.1, 2 The following pandemic waves affected numerous countries, where extreme allocation and rationing of scarce resources was an unusual experience. Only few guidelines existed to assist clinicians in prioritising intensive care resources in a severe pandemic scenario and while some resource scarcity is not unusual most ICU physicians had neither experienced such extreme dilemmas nor received any training to deal with them.
Outside of pandemics, the primary factor in deciding whether ICU care is offered is the probability of survival with a good functional outcome. However, when beds, ventilators and qualified personnel become increasingly scarce, physicians need to make different allocation decisions. During the maximum surge in a pandemic, when ICU resources approach depletion, clinicians could be confronted with the task of refusing patients they probably would have offered treatment under normal circumstances.
Thus, a number of ethical and legal dilemmas can arise when demand exceeds supply.3 Triage guidelines for pandemic crises are designed to assist physicians to apply scarce resources in an optimum way. The underlying ethical principles include utilitarianism (‘greatest good for the greatest number’) egalitarianism (‘allocation based upon equal access to resources’) and life cycle consideration (‘fair-innings’ or ‘years of life saved’) or social benefit consideration (prioritising instrumental value such as front-line health care personnel and other essential workers).4-6
Furthermore, the question arises whether ventilator allocation during extreme scarcity is the responsibility of the authoritative body or the individual physician.7 Leaving allocation choices solely to the individual front-line physician creates risks of variations in triage, potential injustice, discrimination and moral harm for the clinicians.8, 9 There may also be a conflict between what is required and what is legally allowed.3 Therefore, governmental or medical bodies should assume responsibility for developing pandemic triage guidelines to be used by physicians to solve these issues.10
Given the many uncertainties about triage decisions, it is of interest to elicit the perception of frontline physicians at a time when many countries had issued triage guidelines.11 In the present study, we aimed to investigate the opinions of intensivists who treated intensive care COVID-19 patients during the first wave of the COVID-19 pandemic about allocation decisions using virtual case scenarios.
2 METHODS
An online survey was created during July 2020. It was made available to intensivists involved in the Very Old ICU Patient (VIP, vipstudy.org) research network consisting of more than 400 ICUs. Data collection was anonymous. Participation implied consent and agreement to use data for analysis. Ethical approval was not required for this study. Information about aim of the study was provided in an invitation email. The case record form was constructed with the REDCap-software12 hosted on a secure server at Aarhus University, Denmark.
Part 1 of the survey collected baseline data from each intensivist including country of residence, age, gender, ICU experience and religious belief (optional: Muslim, Jewish, Hindu, Catholic, Christian, other, no, no comment). In addition, there were questions about the availability of ICU triage guidelines relevant to the pandemic, the respondent's opinion of such guidelines (Table S1) and who issued them (institution, government, scientific society). Lastly, there were questions about the baseline ICU capacity and increased capacity in the respondent's ICU and hospital.
Part 2 of the survey included three clinical case vignettes concerning virtual triage scenarios regarding the setting of scarce ventilator capacity.
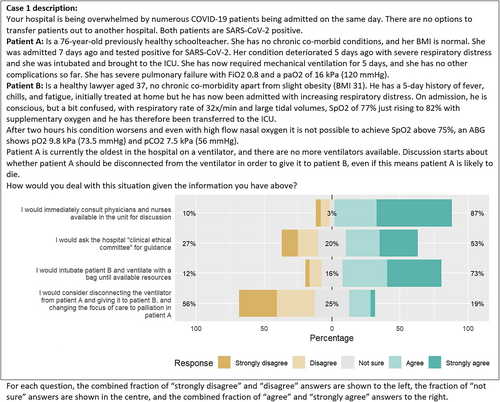
Case 1 (Figure 1) offered the choice between withdrawal of ventilation from 76-year-old patient to re-allocate the ventilator to the 37-year-old patient or extension of capacity (intubation of 37-year-old patient and manual ventilation with a bag).
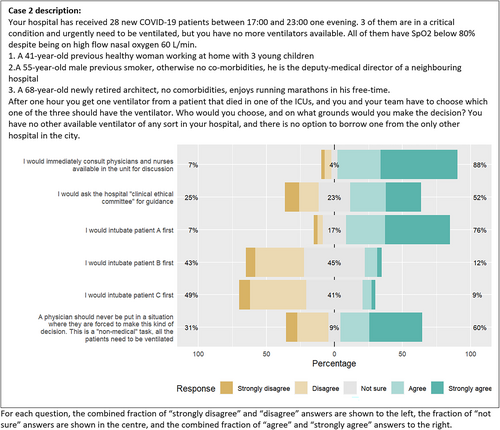
Case 2 (Figure 2) asked to prioritise the last free ventilator between three patients with different age, comorbidity, and social context.
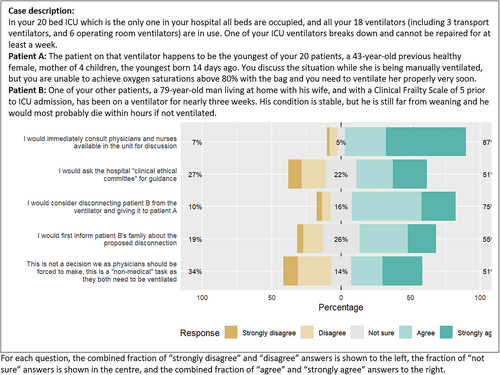
Case 3 (Figure 3) forced a choice resulting from ventilator breakdown in a young patient (43 years old) to possibly reallocate another ventilator after withdrawing it from a 79-year-old ventilated patient.
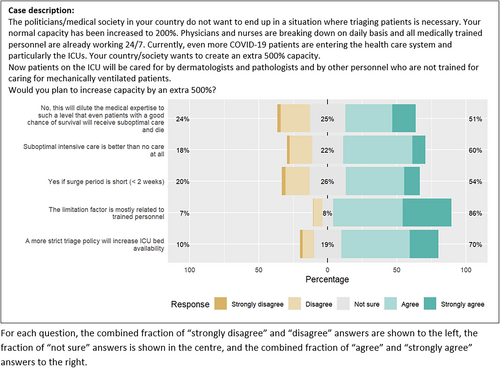
Case 4 (Figure 4) described extreme extension of ICU capacity (health care organisation scenario).
The development of case descriptions was created by a collaboration in the VIP-network's steering group consisting of senior consultant intensivists in European ICUs. Each case was constructed to illustrate variations of specific ethical dilemmas that an ICU physician could potentially encounter. We asked for the respondents' opinion of the cases and compared them to decisions mandated by local guidelines, if available.
Four to six statements following each case could be answered using a five-point Likert scale ranging from ‘Strongly agree’ to ‘Strongly disagree’. The answers ‘agree’ and ‘strongly agree’ were combined to denote ‘agreement’. Likewise, the answers ‘disagree’ or ‘strongly disagree’ were combined to denote ‘disagreement’.
2.1 Statistics
Continuous data were reported as mean (standard deviation) and categorical data as number (percent). Group comparisons were done with the t-test, the t-test on log-transformed data or the chi-square test as appropriate. A logistic regression with the outcomes ‘agree or strongly agree’ was used to analyse Case 1–1, 1–2, 3–3 and 3–5. R version 4.0.2 was used in all calculations.13 Presentation of results was done using the R package Likert.14 In the regression analyses, missing information on the variables age, religion, gender, as well as answers on all cases was imputed using the R package Mice. Applying a multiple imputation approach, a total of m = 100 datasets were generated. Then regression analyses were conducted on each set, results were combined using Rubin's rules.15 No formal power calculation was performed for this observational study.
3 RESULTS
An invitation to participate was sent to 776 ICU physicians in 31 countries within the VIP network. The survey was answered by 437 (56.3%) physicians with a mean age of 44.4 (11.1) and with 13.7 (10.5) years of ICU experience. Respondents were mostly European (88%) (Table S2). Forty-eight percent (n = 208) were religious and 54% (n = 234) worked in a public, university-level hospitals. Triage guidelines were available to 66% (n = 288) of respondents. Of respondents who had guidelines available most found them to reflect their ethical views (n = 252, 88%), and to be practical (n = 227, 79%). Only 18% (n = 52) found available guidelines to be too strict. The mean ICU bed capacity increased during the pandemic (19.6 vs. 36.4 beds; p < .001). Further background data are given in Table 1. Figures 1-34 show first the description of each case vignette and the distribution of answers.
| Demographics | |
| Male, n (%) | 274 (69) |
| Female, n (%) | 123 (31) |
| Age (years), mean (SD) | 44.4 (11.1) |
| ICU experience (years), mean (SD) | 13.7 (10.5) |
| Country | |
| European, n (%) | 388 (88) |
| Non-European, n (%) | 49 (11) |
| Religion | |
| Religious (any), n (%) | 208 (47.6) |
| Not religious, n (%) | 168 (38) |
| Hospital affiliationa | |
| University, n (%) | 243 (56) |
| Public, n (%) | 234 (54) |
| Private, n (%) | 26 (6) |
| ICU bed capacity | |
| Normal bed capacity, median (IQR) | 15 (11–23) |
| Bed capacity after increase, median (IQR) | 26 (18–41) |
| Other ICUS | |
| Other ICUs at your hospital, n (%) | 143 (33) |
| Number of ICU beds in hospital, median (IQR)b | 43.5 (25–60) |
| Number of ICU beds in hospital after increase, median (IQR)b | 62.5 (40–92) |
| Patients | |
| Patients (cumulated) in respondent's ICU, median (IQR) | 32 (10–63) |
| Patients (cumulated) in all ICUs in respondent's hospital, median (IQR)b | 40 (19–68) |
| Guidelines | |
| Guidelines were available for triagec, n (%) | 288 (66) |
| Issued by institution, n (%) | 140 (32) |
| Issued by scientific society, n (%) | 187 (43) |
| Issued by government, n (%) | 113 (25.9) |
| Positive opinion of guidelines, n (%)d | 206 (47) |
| Negative opinion of guidelines, n (%)d | 25 (6) |
| Capacity expansion | |
| Agreement to extreme ICU capacity expansione, n (%) | 195 (45) |
| Disagreement to extreme ICU capacity expansione, n (%) | 96 (22) |
- a More than one answer allowed.
- b Question only available if ‘Other ICUs at your hospital’ was answered with ‘yes’.
- c If the reply were ‘yes’ more than one issuer of guidelines could be marked.
- d Positive opinion to guidelines was defined as having answered Yes to questions 1 and 2 (Table S) and a negative opinion was defined as having answered Yes to questions 3 and 4.
- e Patients who answered Strongly agree or Agree to questions case 4–2 and case 4–3 (demonstrating willingness to expand ICU capacity).
3.1 Consulting colleagues about triage dilemmas
Regarding cases 1–3, the proportion of respondents who reported a positive inclination to consult colleagues in the unit or a clinical ethical committee about triage dilemmas was similar (87–88% or 51–53%, respectively) regardless of the particular dilemma (Figure 1-3). The inclination decreased with age in males but not in females (Figure 5).
3.2 Ventilator allocation and re-allocation
In cases 1–3, regardless of the type of allocation dilemma, the majority of respondents preferred to ventilate the younger patient. A young, healthy patient with small children would be given preference by 76% of the respondents over a 55-year-old and a 68-year-old patient without significant co-morbidities (preferred by 12% and 9% respectively, case 2). In case 1, when given the choice, 73% preferred to extend resources and would ventilate a 37-year-old patient with a bag until a ventilator was available; only 19% would disconnect an older patent to re-allocate the ventilator. In case 2, 76% would select the 41-year-old patient, and in case 3, 74% would disconnect a 79-old patient to re-allocate the ventilator to a 43-year-old patient. In the last case, 55% of respondents would inform the old patient's family first and 60% agreed that this decision was ‘non-medical’ and should not be forced on physicians, while 34% did not agree.
The willingness to reallocate ventilators was not associated with respondents' characteristics, geography, or guideline availability.
3.3 Extreme ICU capacity expansion
In a situation where capacity is already extended to 200% and there is daily break-down of clinicians, 60% said that suboptimal care was better than no care. 54% of respondents agreed to further extension if the surge period were short, but on the other hand, 51% disagreed because of the increased risk of death due to diluted medical expertise. Eighty-six percent agreed that lack of personnel would be the limiting factor, and 70% believed stricter triage would increase ICU bed availability.
4 DISCUSSION
This international survey study undertaken during the first wave of the COVID-19 pandemic provides insight into ethical reasoning of frontline intensivists in times of capacity strain.
The main results were that three out of four intensivists chose to allocate the last free ventilator to the youngest patient. This decision was similar across respondents' age, experience level and religion, and triage guideline availability (Table 1). Similarly, three out of four intensivists were inclined to discuss triage dilemmas with others, and men's inclination decreased with age while women's did not (Figure 5).
A patient's age is often considered when selecting patients for ICU care and increasing age is strongly associated with poor outcome. The possible need for use of strict age limits for triaging was debated during the first wave of the pandemic.2 However, sole reliance on biological age for triage decisions is too simplistic.16 The geriatric concept of frailty is gaining interest in triage17 and is associated with outcome18, 19 and is strongly associated with outcome in elderly COVID-19 patients.20 According to most COVID-19 ethical guidelines, age must not be considered the primary reason for triage but remains a relevant factor when estimating long-term prognosis.11
However, if relevant patient information and history is scarce, weight may be placed on age as a triage criterion as it is easily obtainable.
Accordingly, in the present study, younger age and being a caretaker for young children seemed to be the strongest determinants for allocation of the last ventilator albeit only limited additional information about the patients was available. In a study using a choice experiment with two hypothetical patient profiles, patients' age was found to have the largest impact on the decision of admitting a patient to the ICU, followed by family opinions and severity of the main comorbidity.21
In the ventilator breakdown scenario, three-quarters of respondents would remove a ventilator from an older, frail patient that was already in the ICU and re-allocate it to another patient.
However, in case of a new ICU admission of a younger patient requiring ventilation, a majority would not necessarily reallocate a ventilator from an older, less frail patient revealing an apparent inconsistency in the willingness to reallocate a ventilator. From a simplified triage standpoint, these situations seem similar,6 and a utilitarian approach would suggest reallocation to a younger patient in case of shortage. However, the discrepancy between these cases may point to disagreement or discomfort with such utilitarian approach. The ethics of such a situation are complex. There may be an important gap between utilitarian decision-making and the so-called rule of rescue, that is, the urge to save the life in front of you. A utilitarian approach of reallocation in order to save many people collides with principles of autonomy, beneficence, and non-maleficence with regard to the individual patient and may carry an emotional burden for health professionals. Chu et al argued that the act of reallocating a ventilator from one patient to another is morally inferior to passively palliate.22 Similarly, clinicians may feel that the ethics of selecting one of two patients for the last ventilator differs from reallocating an in-use ventilator to another patient and that withholding treatment differs from withdrawal of treatment. On the contrary, Cameron et al outlined why withholding and withdrawing ventilation should not be differentiated.23 Overall, the complexity of real-world triage may not easily align with ethical theories.24 Underlining this, two-thirds of respondents stated that re-allocation of ventilators should not be the physician's task and half would not communicate the removal of ventilator to the patient's family.
In case 3, it was by chance that the ventilator of the youngest patient broke down. Still, the majority (75%) opted for a utilitarian approach and gave priority to a younger mother in favour of the old patient and were willing to withdraw ventilation from him. In addition to the moral issues, the legality of such a choice is controversial. Under non-pandemic circumstances withdrawing life support without prior decision-making is illegal in many countries and the implications of such actions under triage conditions in the COVID-19 pandemic, with or without support from available guideline, is uncertain.3
The attitudes of physicians towards triage scenarios have been the subject of previous studies.
Israeli and United States intensivists were surveyed with regard to distributing scarce ICU resources and were asked to rate issues in order of importance when admitting a patient to the last ICU bed.25 For Israeli intensivists the two most important issues were: ability to survive to discharge and reversibility of the acute disorder. United States intensivists found: ‘quality of life’ assessed by the patient followed by ‘ability to survive’ as most important. However, only 40% of US intensivists would consider the ability to survive compared to 80% of Israeli intensivists, indicative of large cultural differences.
In a study of 325 lay people and health care workers where asked: What to do when there are more patients than ventilators? And; should health-care workers ever be allowed to take a ventilator from one patient and give it to another?26 A majority of 63% answered confirmatory to the last question, more health care workers than lay participants. Only 22% were negative to this action. Interestingly, a large majority opposed distributing resources based on chance, or lottery (82%), and most would give priority on the ground of surviving critical illness (71%) and the probability to live longer (56%).
Buckwalter et al surveyed lay people in the US on their priorities for scarce resource allocation principles in a pandemic regarding initial distribution and potential reallocation.27 Respondents prioritised the worst-off patients for the initial distribution (a prioritarian approach). Regarding reallocating of already initiated treatment, an egalitarian, first-come-first served approach was preferred which could be considered in-line with results of the present study and illustrating that laypeople understand the difficulty of such a dilemma. Wilkinson et al surveyed public respondents' views of hypothetical triage dilemmas. Age, chance of survival and life expectancy were, among others, preferred ways of prioritising patients.28 Most respondents considered reallocation of resources acceptable practice.
Ethical frameworks for distribution of drugs and vaccines in a pandemic have also been published4, 29 emphasising goals like saving most lives, decreasing the disparity of case fatalities, and strengthening the community's ability to fight the pandemic such as giving priority to health care workers.30 Other guidelines have a complex triage based on a mixture of frailty, some specific pre-existing conditions (comorbidity and age > 85) and acute condition based on organ dysfunction (e.g., SOFA score).31 The major ethical principles for decision-making each hold disadvantages or conflicts with other principles. A utilitarian principle may put disabled patients at a disadvantage or collide with egalitarianism as does prioritising instrumental value.32
Some of the published guidelines of pandemic triage in COVID-19 have elements of such priorities. In a discussion about the framework around rationing ventilators and ICU beds in United States, the authors advocate the use of ‘life years lost’ and ‘opportunity to pass through the stages of life’ (a ‘fair innings’ principle) ahead of using crude estimates of chances of survival.29
4.1 Consultation of colleagues
Existing triage guidelines place emphasis on the ability of the clinician to assess a patient's prognosis. With a large influx of ICU candidates of similar age and initial disease severity assessment of prognosis is of less value and questions if meaningful triage is at all possible.
Of interest, our respondents strongly supported seeking advice from others. Consulting co-workers was preferred by close to 90% in each case, followed by advice from a ‘clinical ethical committee’. However, the latter is often of theoretical interest as such help is seldom immediately available when a decision is urgently needed. For this to work, committees must be present by one or more members in close vicinity to the ICU to be available on short notice. The capacity of such committees could easily be overwhelmed. This aligns with a paper describing triage in the different phases of a pandemic, and that in a surge, if decisions must be made on ‘non-medical grounds’ proposed by the community/society this should not be made by physicians alone.10 Nonetheless, far into the pandemic the availability of guidelines for front-line personnel with specific advice and mandate for triage decisions in ‘no-equipment left’ scenarios varies considerably.11
4.2 ICU capacity expansion
The last question in case 4 tested the willingness of physicians to stretch their own resources.
Close to half of respondents would accept a several-fold increase in ICU capacity. This extent of expansion may not be rational and may hurt the work and emotional capacity of the staff. The topic of burnout among ICU personnel has gained interest over the past years. Even in non-pandemic times burnout and related symptoms are highly prevalent in ICU physicians.33, 34
The prevalence of symptoms of burn-out have increased during the pandemic.35
Triage tasks, concern of own safety, increased workload, heavy use of personal protective equipment etc. may contribute to feelings of loss of influence on work situation and burnout. Naidoo et al suggested increased use of triage committees to alleviate emotional burden.36
Hospitals worldwide have had to increase their ICU capacity during the pandemic. However, there is a limit to how ICU capacity can be stretched, even if physical space in the hospital is available. Many local factors determine this limit, above all the personnel resources. Trained intensivists and nurses can be regarded as the scarcest resource. This was reflected in the answers as 85% agreed that lack of competent personnel was the major limitation. Participants were equally divided in refusing to increase bed capacity to 500% increase because it would dilute expertise too much (51%) and in agreeing because suboptimal care is better than no care at all (60%) and if the surge was short (less than 2 weeks, 54%).
4.3 Limitations
This study has some limitations. The survey was distributed within an established research network which could have created selection bias. However, the participating units represent a broad range of ICU types and geographic locations. Distributing questionnaires in this manner could have resulted in more than one answer from some hospitals/ICUs. For confidentiality reasons names of hospitals and ICUs were not collected, hence we cannot completely correct for an asymmetric response.
However, we identified 373 unique responses using the combination of countries, type of hospital, number of ICU beds and number of increases in ICU beds during the surge. Further, this was a study on the opinions of individual physicians, not the opinion of an ICU or hospital.
With an acceptable response rate spread across many countries, we believe our study is representative of the target group.
We did not ask to what extent the respondent's ICU was affected by the pandemic, which could have influenced opinions. A well-known limitation of the Likert scale is the tendency for respondents to avoid the extremes. However, in this study a large portion of respondents chose extreme values. The answers are subjective and for example ‘agree’ may hold different meaning to different respondents. The questions concerning consulting the hospital's ethical committee was ambiguous as such a body may not exist at some hospitals. Descriptions of patient cases do not at all convey the information available to the clinician at the bedside.
5 CONCLUSIONS
Our findings from the first pandemic wave show gaps in the practical implementation of local triage guidelines. Although guidelines were available to most and considered useful, physicians' allocation decisions were not straightforward. Intensivists may prefer a utilitarian approach for allocation of the last ventilator although this was less clear if this first required withdrawal of ventilation from another patient. The inclination to consult colleagues about triage dilemmas declined with physician's age and male gender. Many found extreme triage tasks to be non-medical and believed that authorities and triage committees should assume responsibility such decisions in case of scarcity of resources.
AUTHOR CONTRIBUTIONS
Jesper Fjølner: idea, first draft and final review; Øystein Ariandsen Haaland, Christian Jung, Dylan W. DeLange, Wojciech Szczeklik, Susannah Leaver, Bertrand Guidet, Sigal Sviri, Peter Vernon Van Heerden, and Michael Beil: idea and review; Christiane S. Hartog: first draft and review; Hans Flaatten: idea and first draft.
ACKNOWLEDGEMENTS
None.
FUNDING INFORMATION
No funding was received for this study.
CONFLICT OF INTEREST
The authors have no conflicts of interest.
Open Research
DATA AVAILABILITY STATEMENT
Data is available upon reasonable request.




