Salvage surgery using simultaneous clamshell thoracotomy with median sternotomy for mediastinal growing teratoma syndrome
Abstract
This report describes the case of a 17-year-old man who developed mediastinal growing teratoma syndrome following two cycles of chemotherapy, after an initial diagnosis of primary mediastinal nonseminomatous germ cell tumor. The large, rapidly-growing mediastinal tumor was completely resected in conjunction with right pneumonectomy, using simultaneous clamshell thoracotomy and median sternotomy. The salvage surgery with perioperative management involved in mediastinal growing teratoma syndrome is presented here.
Key points
Significant findings of the study
- The diagnosis and surgical management are challenging for patients with mediastinal growing teratoma syndrome. Nevertheless, with proper operative planning, favorable outcomes can be attained with complete resection despite the characteristic rapid growth and massive size of these neoplasms.
What this study adds
- In spite of postoperative sternal dehiscence, we believe that a simultaneous clamshell thoracotomy with median sternotomy approach remains a viable option for an extremely large mediastinal growing teratoma, when tumor size prevents safe resection using other approaches due to limited visualization.
Introduction
Growing teratoma syndrome (GTS) is characterized by the enlargement of a nonseminomatous germ cell tumor (NSGCT) despite the administration of appropriate systemic chemotherapy, normalization of serum marker levels, and absence of any pathologic component other than mature teratoma in the surgical specimen. GTS was first described by Logothetis,1 and is rare among primary mediastinal NSGCTs. Kesler et al. reported an incidence of 2.6% (5/188) of mediastinal GTS identified from 188 patients who underwent post-chemotherapy surgery for primary mediastinal NSGCTs.2 The diagnosis and surgical management are challenging for mediastinal GTS.2, 3 Nevertheless, with proper operative planning, favorable outcomes can be attained with complete resection despite the characteristic rapid growth and massive size of these neoplasms.
Case report
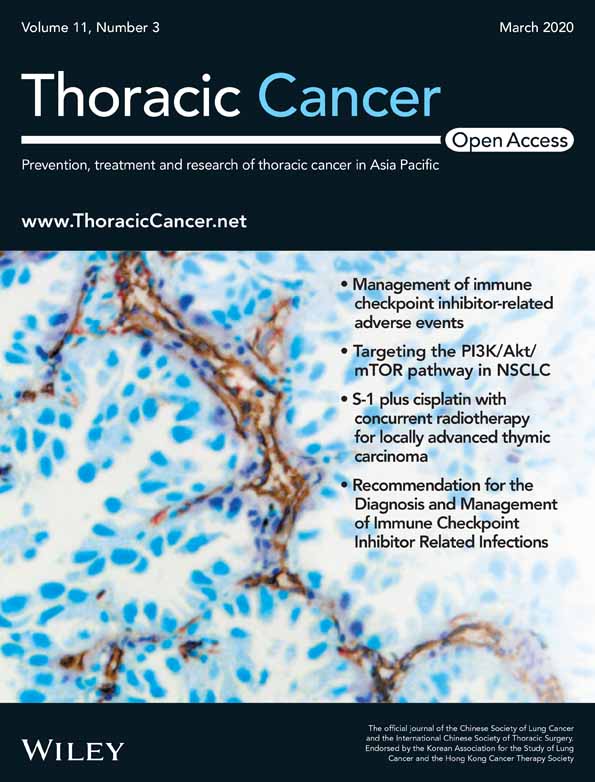
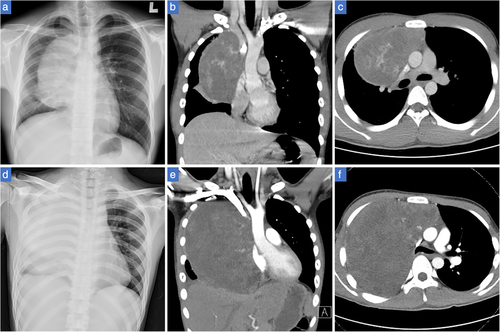
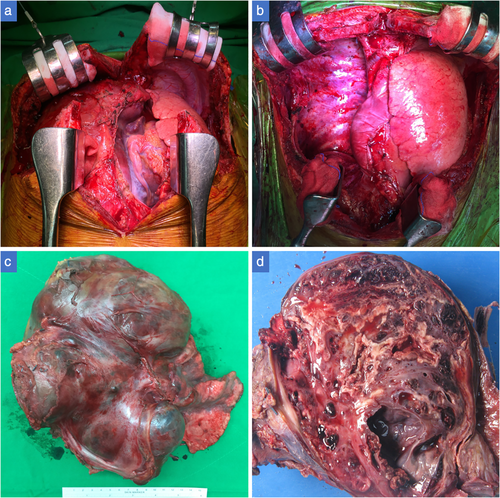
A 17-year-old man presented with a history of worsening chest pain and shortness of breath over a two-week period. A chest X-ray revealed a large anterior mediastinal mass with inhomogeneous components, measuring 13 × 12 × 7 cm on chest computed tomography (CT) (Fig 1a,b,c). Serum tumor markers revealed an alpha-fetoprotein level of 913 ng/mL and a ß-human chorionic gonadotropin level of 321 mIU/mL. CT of the abdomen and pelvis showed no lymphadenopathy or testicular abnormality. Fine-needle aspiration of the mediastinal mass revealed a NSGCT and the patient was started on etoposide, ifosfamide, and cisplatin (VIP) chemotherapy. After completion of the second round of VIP chemotherapy, repeat chest radiography and CT demonstrated a progressive increase in tumor dimensions, with almost complete obliteration of the right hemithorax and marked mediastinal and diaphragmatic compression (Fig 1d,e,f), despite normalization of serum tumor markers. Meanwhile, respiratory distress significantly worsened and the patient developed facial edema. Mediastinal GTS was strongly suspected and urgent surgery was scheduled. Complete resection of the giant mediastinal mass was accomplished via a clamshell approach followed by median sternotomy in conjunction with pneumonectomy for the involved right pulmonary hilum under cardiopulmonary bypass (Fig 2a,b). The resected specimen measured 28 × 19 × 9 cm and weighed 2.2 kg (Fig 2c,d). Final pathologic examination demonstrated a mainly mature teratoma with foci of immature teratoma (<1%) (Fig 3a,b). The postoperative hospital course was prolonged by a nonhealing sternal wound that was successfully managed with negative-pressure wound therapy and subsequent debridement (Fig S1A). Although sternal separation was observed on postoperative CT (Fig S2), there was no sternal instability or cardiopulmonary symptoms. Despite the aforementioned, tumor markers continued to remain in the normal range postoperatively, concomitant multiple splenic nodular lesions were discovered on follow-up CT within one month after surgery, and angiosarcoma was pathologically confirmed on splenectomy. The finding of angiosarcoma in the spleen indicated a high probability of malignant transformation of teratoma. Several cycles of adjuvant chemotherapy were administered thereafter. The patient is alive 15 months following the initial salvage surgery with close follow-up.
Discussion
Primary germ cell tumors of the mediastinum represent 3% to 10% of all tumors in this location.3 However, after the diagnosis is established and chemotherapy is initiated, a few patients develop a growing mediastinal mass, despite normalization of serum tumor markers, with or without symptomatic compression of cardiopulmonary structures. This has been defined as mediastinal GTS and requires salvage surgery.2, 3
Surgical issues specific to this condition warrant consideration. Traditionally, median sternotomy has been the accepted approach for dealing with mediastinal tumors or bilateral pulmonary disease, but exposure to the lower lobes and access to mediastinal tumors with extensive involvement of the hemithorax is often difficult. A clamshell incision enables access to both hila and the pleural cavity.4 Due to the characteristic rapid progression and large size, an uneventful operative approach usually involves combined sternotomy/thoracotomy or clamshell thoracotomy, with or without partial upper hemisternotomy.2, 3, 5 In our case, surgical approach using an initial clamshell approach followed by upper hemisternotomy was performed to afford exposure of the mass and surrounding structures as previously mentioned (Fig S1b).5 A right hemiclamshell approach was deemed inadequate for exposure of the mass which was observed on CT scan (Fig 1e,f). However, owing to almost total obliteration of the right chest by the mass and obvious compression of diaphragm, subsequent lower hemisternotomy was carried out to obtain the best access to the right chest wall, diaphragm, mediastinum, and right pulmonary hilum. Eventually, the mass was completely resected with right pneumonectomy under a cardiopulmonary bypass. As this extreme salvage surgical approach has not previously been reported in the literature, several postoperative adverse events must be discussed. First, sternal dehiscence including override or separation is a major complication following clamshell thoracotomy. We used a parasternally crossed technique, similar to that reported by Koster et al. which effectively reduces the incidence of sternal dehiscence.6 Postoperative sternal separation did occur, but reconstructive surgery was not required and the patient had no sternal instability. Second, sacrifice of the internal mammary arteries restricts future options for coronary revascularization. Sternal wound complications should not be underestimated. With early recognition and aggressive treatment in this case, recovery from a superficial nonhealing sternal wound was uneventful, without progression to a deep sternal wound infection or mediastinitis.
In addition to mediastinal GTS, mediastinal tumors refractory to previous local treatments with curative intent or exclusive chemotherapy in case of bulky tumors often require mediastinal salvage surgery, which can offer a chance of curative treatment in selected patients with an acceptable morbimortality.7
In conclusion, we believe that this salvage surgery (simultaneous clamshell thoracotomy with median sternotomy) remains a viable option for an extremely large mediastinal tumor, when tumor size prevents safe resection using other approaches due to the limited visualization and inherent difficulty in manipulating such large lesions.
Acknowledgments
This work was supported by Kaohsiung Medical University Hospital (KMUH107-7M19). The authors acknowledge the help of Jadzia Chou with regard to language revision.
Disclosure
The authors declare that there are no conflict of interests.