Cardiopulmonary exercise testing screening and pre-operative pulmonary rehabilitation reduce postoperative complications and improve fast-track recovery after lung cancer surgery: A study for 342 cases
Abstract
Background
An evaluation of cardiopulmonary exercise testing (CPET) screening and pre-operative pulmonary rehabilitation in reducing postoperative complications and improving fast-track recovery in high-risk patients who undergo resection for lung cancer.
Methods
Of 342 potential lung cancer cases, 142 high-risk patients were finally divided into two groups: group R (n = 71) underwent an intensive pre-operative pulmonary rehabilitation program (PRP), followed by lobectomy; group S (n = 71) underwent only lobectomy with conventional management. Postoperative complications, average days in hospital, postoperative days in hospital, and cost were analyzed.
Results
The 142 high-risk patients were screened by smoking history and CPET. Sixty-eight patients had bronchial hyperresponsiveness (BHR) and 47 patients had peak expiratory flow <250 L/minute by CPET. The rate of postoperative total complications in group R (16.90%) was significantly lower than in group S (83.31%) (P = 0.00), as was the rate of postoperative pulmonary complications PPC: group R (12.81%) versus S (13.55%) (P = 0.009); the PPC in the left lung (17.9%) was higher than in the right lung (2.3%) (P = 0.00). The average days in hospital in group S was significantly higher than in group R (P = 0.03). There was no difference between groups in average hospital cost (P = 0.304).
Conclusion
Pre-operative screening using CPET is conducive to identifying high-risk patients for lung resection. Pre-operative pulmonary rehabilitation is helpful to reduce postoperative complications and improve fast-track recovery.
Introduction
Surgery is the major treatment method for lung cancer, especially for non-small cell lung cancer (NSCLC). The prevalence of chronic obstructive pulmonary disease (COPD) in patients with lung cancer is 73% in men and 53% in women.1 Postoperative pulmonary complications (PPC) are the main cause of mortality during the postoperative period2 and pulmonary infection is the most common of these.3, 4 Various reports have highlighted the need to improve lung function and quality of life in patients with COPD.5, 6 However, the value of pre-operative pulmonary rehabilitation in lung cancer patients with COPD, who are candidates for lung resection, is controversial.7, 8 Previous studies have included small sample sizes, using conventional pulmonary function tests (PFTs) for determination of COPD level, and treating with simple physical pulmonary rehabilitation without medication.9 However, none of these studies have included patients with cardiopulmonary high risks who could be determined by cardiopulmonary exercise testing (CPET).1011 There has been no research evaluating CPET and pre-operative pulmonary rehabilitation in lung cancer. Our study was designed to evaluate CPET and pre-operative pulmonary rehabilitation, which may improve postoperative complications and fast-track recovery in high-risk patients who undergo resection for lung cancer.
Material and method
Clinical data and grouping
From November 2008 to June 2011, 342 consecutive lung cancer patients, who were without surgical contraindication and met all eligibility criteria through general pre-operative examinations, pre-operatively underwent CPET (see Fig. 1 & Table 1). There were 142 patients determined to be high risk, according to the following inclusion criteria: (i) smoking index > 800 pack-year, and duration after quitting smoking <2 weeks; (ii) bronchial hyperresponsiveness; and (iii) peak expiratory flow (PEF) < 250 L/minutes/kg, 4.1.0 L < forced expiratory volume in one second (FEV1)<1.2 L and 40% < FEV1% < 60%.
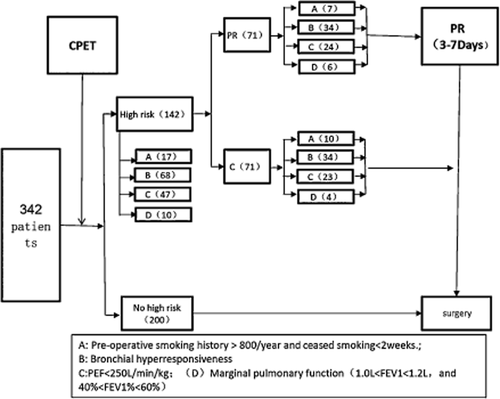
Diagram for patient selection. CPET, cardiopulmonary exercise testing; FEV1, forced expiratory volume in one second; PEF, peak expiratory flow; PR, pulmonary rehabilitation.
| Group | No. | Gender (no) | Average age (year) | Histology (no) | 2009UICC stage (no) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | F | SC | Ad | AS | SCLC | LC | I | II | III | IV | ||||
| Total cases | 342 | 147 | 195 | 63.21 ± 17.09 | 73 | 215 | 28 | 15 | 11 | 184 | 116 | 37 | 5 | |
| No high risk | 200 | 63 | 137 | 60.12 ± 11.44 | 32 | 139 | 13 | 9 | 7 | 117 | 58 | 22 | 3 | |
| High Risk | No. | 142 | 84 | 58 | 65.02 ± 10.25 | 41 | 76 | 15 | 6 | 4 | 67 | 58 | 15 | 2 |
| C | 71 | 44 | 27 | 59.67 ± 13.03 | 14 | 43 | 7 | 4 | 3 | 41 | 19 | 11 | 0 | |
| PR | 71 | 40 | 31 | 66.33 ± 10.17 | 27 | 33 | 8 | 2 | 1 | 26 | 39 | 4 | 2 | |
- Ad, carcinoma; AS, adeno-squamous carcinoma; C, control; F, female; LC, large cell lung cancer; M, male; PR, pulmonary rehabilitation; SC, squamous carcinoma; SCLC, small cell lung cancer.
The 142 high-risk patients were divided into two groups: group R (71) underwent an intensive pre-operative pulmonary rehabilitation programme (PRP), while group S (71) underwent only lobectomy (Table 2)
| Group | PR group | C group | P | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | Total | A | B | C | D | Total | |||
| No | 7 | 34 | 24 | 6 | 71 | 10 | 34 | 23 | 4 | 71 | 0.634- | |
| Male | 7 | 14 | 15 | 4 | 40 | 10 | 15 | 16 | 3 | 44 | 0.221 | |
| Female | 0 | 20 | 9 | 2 | 31 | 0 | 19 | 7 | 1 | 27 | 0.561 | |
| Average age (year) | - | - | - | - | 66.33 ± 10.17 | - | - | - | - | 59.67 ± 13.03 | 0.332 | |
| Operation | Open | 3 | 10 | 15 | 1 | 29 | 5 | 14 | 13 | 0 | 32 | 0.227 |
| VATS | 4 | 24 | 9 | 5 | 42 | 5 | 20 | 10 | 4 | 39 | 0.501 | |
| Histology | Sc | 6 | 4 | 17 | 0 | 27 | 7 | 5 | 2 | 0 | 14 | 0.031 |
| Ad | 0 | 25 | 4 | 4 | 33 | 1 | 22 | 19 | 1 | 43 | 0.050 | |
| AS | 1 | 4 | 3 | 0 | 8 | 0 | 5 | 1 | 1 | 7 | 0.120 | |
| SCLC | 0 | 1 | 0 | 1 | 2 | 1 | 0 | 1 | 2 | 4 | 0.211 | |
| LC | 0 | 0 | 0 | 1 | 1 | 1 | 2 | 0 | 0 | 3 | 0.342 | |
| TNM-Stage (2009UICC) | I (Ia+Ib) | 2 | 14 | 7 | 3 | 26 | 4 | 20 | 16 | 1 | 41 | 0.015 |
| II (IIa+IIb) | 4 | 15 | 17 | 3 | 39 | 5 | 7 | 5 | 2 | 19 | 0.034 | |
| III (IIIa+IIIb) | 1 | 3 | 0 | 0 | 4 | 1 | 7 | 2 | 1 | 11 | 0.063 | |
| IV | 0 | 2 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0.102 | |
- A: pre-operative smoking history > 800/year and ceased smoking < 2 weeks; B: bronchial hyperresponsiveness; C: peak expiratory flow (PEF) < 250 L/min/kg; D: marginal pulmonary function (1.0 L < forced expiratory volume in one second [FEV1] < 1.2 L and 40% < FEV1% < 60%). Ad, carcinoma; AS, adeno-squamous carcinoma; C, control; LC, large cell lung cancer; PR, pulmonary rehabilitation; SC, squamous carcinoma; SCLC, small cell lung cancer.
Method
Pulmonary function test (PFT)
All tests were undertaken by the department of PFT at the West China Hospital,Sichuan University. Test parameters included pulmonary ventilation function (pulmonary ventilation, pulmonary ventilation volume, small airway function, pneodynamics, inhalation of gas distribution, respiratory muscle function) and pulmonary gas exchange function (diffusive function, ventilation perfusion ratio).
Cardiopulmonary exercise testing (CPET)
A treadmill was used to measure cardiopulmonary exercise function, with resistance in 27 watts, moving as fast as possible in six minutes. The heart rate and SpO2 (Pulsox-300, Konica Minolta Sensing, Inc., Osaka, Japan) were measured from tranquilization to the end of exercise; the Borg Dyspnea Score, six-minute walk distance (6-MVD), and energy-consumption were also recorded.12
Pre-operative pulmonary rehabilitation method
Drug intervention13
- Antibiotic treatment: 2 gm of cefmetazole (Sichuan Hexing Pharmaceutical Co. Ltd., Chengdu, China) was administered by intravenous drip twice a day.
- Bronchodilator treatment: Aerosol inhalation of ipratropium bromide (Atrovent, Boehringer Ingelheim Shanghai Pharmaceutical Co., Ltd, Shanghai, China) and budesonide inhalation suspension (AstraZeneca Pty Ltd. UK) was administered twice a day.
- Expectorant treatment: 60 mg of ambroxol hydrochloride (Boehringer Ingelheim Shanghai Pharmaceutical Co., Ltd) was administered by intravenous drip twice a day.
- Corticosteroid treatment: 40 mg of methylprednisolone (Pfizer Manufacturing, Belgium NV) was administered by intravenous drip twice a day.
- Never-smokers or patients whose smoking index was less than 400 package-years and non-smoking time was longer than two weeks, underwent antibiotic, bronchodilator, and expectorant treatments three days prior to surgery. Patients with a higher smoking index (400 to 800 package-years) or a shorter non-smoking time (less than 2 weeks) received additional pulmonary rehabilitation physical training and required a corticosteroid treatment one day prior to surgery. Patients with a significantly high smoking index (more than 800 package-years) received all pulmonary rehabilitation measures, which included not only drugs but physical training.
- Patients with bronchial hyperreactivity received bronchodilator and expectorant treatments three days prior to surgery.
- Patients with lower PEF (PEF<250 L/minutes) underwent the same treatments as patients with a high smoking index.
- Patients whose lung function was in critical condition received all of the rehabilitation measures, except for antibiotic treatment.
Pulmonary rehabilitation training with physical intervention
- Training for abdominal breath: Patients were in a supine position, with a deep slow inspiration through their nose and held their breath for a short time, followed by a slow expiration via the mouth. When the diaphragm descended, the abdomen was convex in inspiration; when the diaphragm ascended, the abdomen was concave in expiration. This training was undertaken twice a day, with a sequence of 20–30 breaths each time.
- Breath training device: Patients used a volumetric exerciser (Voldyne 5000, Sherwood Medical Supplies, St Louis, MO, USA) for training. Patients were sitting with a tight suction nozzle after calm expiration, then deeply inhaled as fast as possible, holding their breath for two to three seconds. Patients then moved the nozzle and pursed their lips, slowly exhaling. The excise was repeated four times, for a 20-minute duration.
- Lower extremity endurance training: (a) Power bicycle exercise training. Patients could progressively regulate their speed and power. Total power was controlled with a five to seven point BORG score. If the patients felt obvious shortness of breath, leg exhaustion, a decrease of SpO2 (<88%), or any other malaise resulting from complications, the exercise must cease until their condition can withstand subsequent training. Each training session should last 15 to 20 minutes twice a day. (b) Stair climbing. Professional therapists should accompany patients. Patients should purse their lips in breath and avoid holding their breath when climbing. If patients feel dyspnea, they should have a short rest, but should continue to climb as soon as possible. Each training session should last 15 to 20 minutes twice a day.
Surgical method
Video assisted thoracic surgery (VATS) and conventional posterolateral thoracotomy were used in our research. The VATS procedure was a single-direction thoracoscopic lobectomy, as reported by Liu et al.14 All surgeries included systematic lymph node dissection (No. 5,6,7,8,9,10 group in left; no. 2,3,4,7,8,9,10 group in right).
Post-surgical management
Intravenous patient-controlled analgesia (Tramadol Hydrochloride, Medochemie Ltd., Cyprus, UK) was provided to all patients; a non-steroidal analgesic (oxycodone or ibuprofen) provided added effect for patients as required. The presence of an air leak and the volume of thoracic drainage fluid determined when patients required a chest X-ray. The tube should be removed in accordance with chest X-ray results. Once the tube is removed, analgesic management should cease.
Observation index
Postsurgical complications included: diarrhea, allergy, aerodermectasia, arrhythmia, aconuresis, aerothorax, pleural effusion, and lung infection. The diagnostic criteria for lung infection included: clear etiology; atelectasis or mass shadows in imaging; fever; and a white blood cell count of more than 15 000/ml.15
The average hospital stay included pre-operative and postoperative duration. Pre-operative hospital stay was from the date of admission to the date of surgery; postoperative hospital stay was from the date of surgery to the date of discharge.
Average hospital costs included the costs of examinations, surgery, drugs, and the cost of staying in a ward. Pulmonary rehabilitation costs included the costs of the test of cardiopulmonary function, physical treatment, drugs, and the cost of the volumetric exerciser.
Statistical analysis
Data were analyzed using SPSS statistical software, version 13.0 (IBM Corporation, Armonk, NY, USA). Enumeration data were presented as mean ± standard deviation. Descriptive group data were compared using the unpaired the Pearson chi-square test and the rank sum test. Statistical significance was at P < 0.05.
Results
Analysis of high risk patients with lung cancer
Of the 342 patients, there were 17 with a significantly high smoking index (more than 800 package-years) and shorter non-smoking time (less than 2 weeks; 4.970%, 17/342) and 10 whose lung function was in a critical condition (1.0 L < FEV1 < 1.2 L, and 40% < FEV1% < 60%; 2.924%, 10/342). Eighty-four patients (19.88%) had post bronchial hyperresponsiveness (BHR), and 47 (47/342, 13.74%) had PEF < 250 L/minute by CPET. (Table 2)
Analysis of the complications of patients with lung cancer
The total rate of postoperative complications in group R (16.90%)was significantly lower than in group S (83.31%; P = 0.00). Group R experienced fewer instances of the most common type of postoperative pulmonary complications, with the exception of allergies (P = 0.10) (Table 3).
| Kinds | PR | C | P |
|---|---|---|---|
| Diarrhoea | 1.40% (1/71) | 8.45% (6/71) | 0.02 |
| Anaphylactic reaction | 1.40% (1/71) | 0% (0/71) | 0.10 |
| Subcutaneous emphysema | 1.40% (1/71) | 12.67% (9/71) | 0.00 |
| Arrhythmia | 2.81% (2/71) | 18.30% (13/71) | 0.02 |
| Urinary incontinence | 2.81% (2/71) | 8.45% (6/71) | 0.02 |
| Aerothorax | 1.40% (1/71) | 14.08% (10/71) | 0.00 |
| Pleural effusion | 2.81% (2/71) | 9.85% (7/71) | 0.02 |
| Pulmonary infection | 2.81% (2/71) | 13.55% (8/71) | 0.009 |
| Total | 16.90% (12/71) | 83.31% (59/71) | 0.00 |
- C, control; PR, pulmonary rehabilitation.
Analysis of lung infection
The rate of postoperative lung infection in group R (2.81%) was significantly lower than in group S (13.55%) (P = 0.009), and the lung infection in the left lung (17.9%) was higher than in the right (2.3%) (P = 0.00).
Analysis of hospital stay
The average hospital stay in group S (19.21 ± 9.89d) was significantly higher than in group R (14.54 ± 4.71d) (P = 0.03), and the length of postoperative hospital stay in group S (11.07 ± 4.66d) was significantly longer than in group R (7.21 ± 3.18d) (P = 0.00).
Analysis of the average cost in hospital
There was no difference between the two groups in the average hospital costs (R = 40131.72 ± 4663.28¥ and S = 36943.33 ± 3663.28¥; P = 0.304); the cost of pulmonary rehabilitation for all patients is 1013.30 RMB.
Discussion
The rate of postoperative pulmonary complications (PPC) after lung resection was 2–51% (average 25%),1, 16, 17 with lung infection as the major PPC,18 which was the main cause for postoperative mortality, longer hospital stay, and increase in costs. Since the 1970's there have been vast improvements in surgical technology, medical apparatus and instruments, and antibiotics; however, the rates and types of complications of lung resection over this period remain remarkably similar.17, 19 The spectrum of diseases eligible for lung resection have not varied, and the excisional lobectomy margin has not changed. Why have the developments in surgery and postoperative management failed to diminish the complications? According to our analysis of reported data, there were some pre-operative high-risk causes that could not be found through routine examination or were even neglected prior to surgery. Dancewicz et al.20 reported that 30% of patients with lung cancer had a respiratory tract colonized by microorganisms prior to surgery, which was the main cause of postoperative lung infection. Another high risk was found in patients in critical condition with comparatively low lung function.21 Although some reports have shown that pulmonary rehabilitation could improve symptom management, lung functional status, and quality of life,8, 22 no research has reported similar results in patients with lung cancer who have undergone lobectomy. To our knowledge, this is the first study to examine the effects of CPET and pulmonary rehabilitation for lung cancer prior to surgery.
A conventional cardiopulmonary function test, including a general lung function test, electrocardiogram, and echocardiography showing static cardiopulmonary function cannot reflect the dynamic cardiopulmonary capacity on load conditions and the role of determining the potential risk of cardiopulmonary diseases for surgery is limited.11 CPET is a global test of the cardiopulmonary capacity, which can show the entire oxygen transport system starting with the lungs and ending with the skeletal muscles, a supplement for the currently available conventional cardiopulmonary function test.23 Our research shows that patients with lung cancer with lower PEF (PEF < 250 L/minutes) (13.74%) and bronchial hyperreactivity (19.8%), detected by CPET, cannot be determined through a conventional cardiopulmonary function test. The two risks were significant predictors of postoperative complications in the lungs, especially for bronchial spasm and lung infection. The pre-operative pulmonary rehabilitation programme (physical therapy and drugs) for patients at high risk, such as lower PEF, bronchial hyperreactivity, significantly high smoking index (more than 800 package-years) and shorter non-smoking time (less than 2 weeks), and lung function in critical condition, could have a 5-fold decreased risk of postoperative pulmonary complications, including lung infection.
Another parameter, such as max VO2, characterized the effective integration of the neural, cardiopulmonary, and metabolic systems. Much research has shown that for patients undergoing a lung resection, an estimated postoperative max VO2, FEV1, and diffusion capacity should be mandatory before proceeding with the resection.
A pulmonary rehabilitation plan could reduce pulmonary complications by: (i) improving pulmonary ventilation: aerosol inhalation of bronchodilator or corticosteroid prior to surgery could remove bronchial spasm and drain sputum in the airway; (ii) improving the microenvironment of the airway: heavy smokers and patients of advanced age have a different airway microenvironment, with an increase in pathogenic bacterium or opportunistic pathogens; the use of drugs (exp. pertinence antibiotics) prior to surgery could control potential infection caused by pathogens; and (iii) physical rehabilitation training could partly improve lung function, especially respiratory muscle endurance, which could improve the power of the drain of sputum for postoperative patients.
In 34% of cases of lung cancer, the colonization of potentially pathogenic bacteria was isolated; both gram-positive and gram-negative bacteria were included.20 Bronchial colonization with potentially pathogenic microorganisms may represent an independent stimulus for additional airway inflammation.24 Pulmonary complications were one of the major factors contributing to postoperative short-time mortality, particularly in current smokers. Interventions targeting prevention and early treatment of pulmonary complications have the likelihood of reducing postoperative mortality after elective surgery.25 Testing the pre-operative prediction of pathogens, which may be involved in airway infection, could guide antibiotics.26 Of course, the emergence of antimicrobial resistance has been contemporaneous with the intensive use of antibiotics.27 Therefore, pre-operative antimicrobial therapy is not routinely recommended in all patients with high risks, but only in heavy smokers and patients of advanced age.
The improvement of pulmonary function was positively correlated with the duration of pulmonary rehabilitation training. However, patients' compliance decreased if the length of pulmonary rehabilitation training was too long,22 and a long duration prolonged the average hospital stay. Frésard et al.28 reported that three to 15 days was an acceptable interval of pre-operative rehabilitation training that could improve pulmonary function significantly, and balanced the contradiction between patients' compliance and the effect of pulmonary rehabilitation. In our study, the duration was from three to seven days. Although the pre-operative stay was prolonged by rehabilitation, the postoperative stay was significantly shortened. Compared with the control, the total hospital stay of group R (rehabilitation group) was shorter. The cost of pulmonary rehabilitation was 1000 RMB (about $180 USD). However, because less days were spent in hospital, the cost of pulmonary rehabilitation did not increasing the total cost. According to the data from our study, pulmonary rehabilitation in patients with lung cancer with operative high risks had a significant financial benefit.
Our research had some limitations. Some of the patients underwent VATS in both groups (R & S). Because VATS could decrease postoperative pulmonary complications and the average hospital stay,23 the interaction between VATS and pulmonary rehabilitation should be investigated in a further study. The intervention of pulmonary rehabilitation should be deeply investigated and optimized for individualization. Finally, the duration of pulmonary rehabilitation should be determined by more objective quota rather than subjective sensation.
Conclusion
In conclusion, half of the lung cancer patients studied had a varied risk correlated with postoperative complications. We found that 41.52% (142/342) of patients were at high-risk prior to surgery. Pre-operative screening using CPET was conducive in identifying high-risk patients for lung resection. Pre-operative pulmonary rehabilitation could improve cardiopulmonary function, control pre-operative potential lung infection, decrease postoperative complications, and promote a faster recovery. Pulmonary rehabilitation did not increase the total hospital stay or cost.
Disclosure
No authors report any conflict of interest.