What Is the Safe Observation Period Following Image-Guided Percutaneous Renal Biopsies?
Funding: The authors received no specific funding for this work.
This work was presented as an oral presentation at the The European Congress of Radiology (ECR) 2025 in Vienna, Austria.
ABSTRACT
Purpose
To investigate the timing, type, and severity of complications following percutaneous, image-guided renal biopsy and to determine if the current observation period of 4 h can be safely reduced.
Methods
Consecutive image-guided percutaneous renal biopsies performed between 2017 and 2022 in adult patients by radiology medical staff were included. The RIS-PACS imaging systems and electronic medical records (EMR) were accessed to obtain relevant patient information and procedural reports. A retrospective analysis of the type and timing of complications was performed against patient demographics and biopsy-related variables. Probabilities were calculated for a range of observation periods to assess the proportion of complications identified by shortening the observation period from 4 h.
Results
Three hundred and thirty-two percutaneous renal biopsies were included, and 44 (13%) complications were identified within the 4 h observation. Twenty-nine complications were post-operative bleeding, of which 2 developed macroscopic haematuria, 25 peri-nephric haematoma and 2 had haemodynamic instability with either haematuria or peri-nephric haematoma. 64% of all complications occurred within the first hour, and 86% occurred within 2 h. Of the six complications occurring after 2 h, two were post-operative bleeding in non-targeted renal biopsies requiring admission, and the other four did not require additional observation/procedures.
Conclusion
The vast majority of complications after targeted and non-targeted renal biopsies tend to occur within the first 2 h of observation. Complications that occurred after 2 h observation were often pain related, something that can be overcome with a standardised post-operative analgesic regime. It may be possible to safely reduce observation times following image-guided targeted renal biopsies.
1 Introduction
Renal biopsy is a crucial diagnostic tool allowing for histological diagnosis and subsequent management of a range of focal renal lesions and diffuse renal pathologies in both transplanted and native kidneys. However, as with any invasive procedure, renal biopsies can result in a range of complications for the patient. Minor complications, such as pain and mild perinephric bleeding, occur in approximately 4%–5% of patients [1]. Similarly, the incidence of macroscopic haematuria ranges between 3% and 4% [1-3]. The rate of major complications, that is, those requiring further interventions, including blood transfusions, embolisation, or nephrectomy, lies between 1% and 2% [1, 3].
To identify these complications post-operatively, patients must be observed for a period of time. Nursing staff monitor haemodynamic observations, pain scores, and subjective impression, with significant changes in clinical condition identifying those requiring medical review. However, a lengthy observation period requires greater resources, limiting clinical capacity, and thus, a balance between safety and efficiency is sought.
The timing of any complications, and therefore the given monitoring period, varies between locations. Some suggest that the majority of bleeding-related events can be identified shortly following the procedure [4] and advocate for brief observation between 4 and 6 h. Others note a delayed incidence of complications post-renal biopsy, favouring longer monitoring up to 24 h [1, 3].
This study aims to establish the timing of complications following percutaneous, image-guided renal biopsy and to determine a safe and practical observation period duration.
2 Methods
This was a retrospective cohort study. All patients who underwent a percutaneous image-guided renal biopsy at the Department of Radiology of a tertiary referral centre in Victoria, Australia, between 2017 and 2022 were retrospectively collected from the Radiology Information System (RIS) using the following search terms: ‘Renal’ and ‘Biopsy’. Inclusion criteria were all patients aged 18 years and older, undergoing image-guided, percutaneous renal biopsies, targeted and non-targeted, on either a native or transplanted kidney, performed by radiology medical staff. Biopsies performed by other specialities, such as renal physicians, were excluded from the study. The post-procedure instructions were similar for all patients, bedrest and standardised observations until 4 h post-procedure. Outpatients were observed in the Radiology Day Ward, whereas inpatients completed their observation on the ward of the admitting unit.
The electronic medical records (EMR) system was used to obtain information regarding patient condition following biopsy, incidence of any complications, as well as patient data, such as anticoagulation or antiplatelet status. All forms of anticoagulant or antiplatelet were included, with the exception of prophylactic enoxaparin. Our institutional guidelines follow the CIRSE standard of practice on perioperative anticoagulation management during interventional radiology procedures [5]. This guideline recommends withholding prophylactic enoxaparin 12 h before medium/high bleeding risk procedures. All patients routinely get their enoxaparin administered at 20:00; therefore, they automatically have a minimum of 12 h following the last dose of prophylactic enoxaparin.
Specific procedural details, including needle gauge and imaging modality used, were collected from the picture archiving and communication system (PACS). The CIRSE grading system was used to determine the severity of post-procedural complications [6]. In the case of multiple complications, the highest grade was used for analysis.
The Strobe checklist was used for this study. Ethical approval was obtained from the local Human Research Ethics Committee (HREC), reference number: RES-23-0000-015Q, and the need for informed consent was waived.
2.1 Statistical Analysis
Data analysis was performed using RStudio (using R version 3.6.1). The cumulative incidence of complications was calculated between 0 and 4 h. This figure is described both as cumulative incidence and its inverse (1—cumulative incidence), the complication-free probability.
Additionally, the cumulative incidence of complications was calculated from the end of several shorter observation periods until the end of the original 4-hour observation period. For example, having completed 1 h of observation without complication, what was the incidence of complications for patients between hours 1 and 4?
Comparative group analysis of complication incidence within subgroups based on individual patient demographics and biopsy-related variables was performed using the non-parametric statistic Wilcoxon rank sum, as well as Pearson's chi-squared and Fisher's exact tests depending on data type. There were no missing data in this study.
3 Results
3.1 Patient Demographics
A total of 332 biopsies performed on 307 patients were included in this study. Nineteen patients underwent two renal biopsies, two patients underwent three biopsies, and one patient underwent four separate renal biopsies. Data were analysed on a per-biopsy basis. Of the original 445 cases produced by RIS, 109 were excluded as these were not performed by radiology medical staff, and 4 further cases were excluded as the patients were under the age of 18.
There was a slightly higher proportion of men (n = 213, 64%). The median age was 62 years (IQR range 50–72). Biopsies were performed in an outpatient setting in 74% (n = 245). There were more targeted biopsies (n = 214, 64%) performed, and ultrasound guidance was used in 61% of all biopsies (n = 203) and CT in 39% (n = 129). Needle gauge for targeted biopsies was 18G in 77% of cases (164/214). For non-targeted biopsy, 16G gauge was used for 62% (73/118), and 18G in 36% (42/118). Forty-one (12%) biopsies were performed in transplanted kidneys, of which the majority were non-targeted (95%, 39/41). Track closure (e.g., with Gelfoam slurry) was used in 30% of cases (n = 99). Twenty-three per cent of patients (n = 77) were taking a form of oral anticoagulant or antiplatelet therapy prior to the biopsy, with 6% (n = 21) taking dual or single antiplatelets within 24 h of the biopsy (Table 1). NOACs or other anticoagulants were routinely withheld prior.
| N = 332a | |
|---|---|
| Age at time of procedure | 62 (50, 72) |
| Gender | |
| Male | 213 (64%) |
| Female | 119 (36%) |
| Admission status | |
| Inpatient | 87 (26%) |
| Outpatient | 245 (74%) |
| Biopsy approach | |
| Non-targeted | 118 (36%) |
| Targeted | 214 (64%) |
| Imaging modality | |
| US | 203 (61%) |
| CT | 129 (39%) |
| Gauge of biopsy needle | 18 (16, 18) |
| Number of passes | |
| 1 | 96 (29%) |
| More than 1 | 236 (71%) |
| Track closure | 99 (30%) |
| Native kidney | 291 (88%) |
| Timing of last dose of anticoagulant or antiplatelet, n = 77 | |
| Within 24 h | 21 (27%) |
| Longer than 24 h | 56 (73%) |
- a Median (IQR); n (%).
3.2 Complications Within 4-h Observation
Forty-four complications (13%) were recorded within the routine 4 h of observation. Of these, 29 (66%) were classified as CIRSE severity Grade 1, 4 (9%) were Grade 2, and 11 (25%) were Grade 3. There were no Grades 4, 5 or 6 complications in our cohort (Table 2).
| CIRSE grade | < 1 h, N = 28a | 1–2 h, N = 10a | 2–3 h, N = 4a | 3–4 h, N = 2a | Overall, N = 44a |
|---|---|---|---|---|---|
| 1 | 22 (79%) | 3 (30%) | 3 (75%) | 1 (50%) | 29 (66%) |
| 2 | 2 (7%) | 1 (10%) | — | 1 (50%) | 4 (9%) |
| 3 | 4 (14%) | 6 (60%) | 1 (25%) | — | 11 (25%) |
- a n (%).
Of the 44 complications, 15 were pain-related and managed with oral medications; 6 of these required a prolonged period of observation without any further intervention (Table 3). The 29 remaining complications related to bleeding, either solely macroscopic haematuria (2/29), peri-nephric haematoma (25/29), or haemodynamic instability + haematuria/haematoma (2/29). Of the 29 cases of bleeding, 9 were inpatients—1 had a hypotensive episode responding to IV fluids around 6 h later; they were evaluated with contrast-enhanced CT, but no further intervention was required. Twenty were day-case patients—6/20 were admitted for further observation, and 14/20 were discharged at 4 h with no further intervention. Four of those 14 discharged at 4 h had repeat imaging prior to discharge.
| Hours observed | Complication-free probability (95% CI) | Cumulative incidence (95% CI) |
|---|---|---|
| 0 | 87% (83%–90%) | 13% (10%–17%) |
| 1 | 95% (89%–98%) | 5% (2%–11%) |
| 2 | 98% (93%–99%) | 2% (1%–7%) |
| 3 | 99% (93%–100%) | 1% (0%–7%) |
Of the 14 discharged home after experiencing a complication, 2 patients with minor perinephric bleeds on post-procedural imaging, but no further issues identified during the 4-h observation period, had delayed representation. The first patient presented 7 days later with new frank haematuria and loin pain; a biopsy had been performed for a focal, exophytic lesion. The second patient presented at 5 days with loin pain associated with straining and active bleeding; both patients underwent angiography with embolisation on the day of representation to the hospital.
Of the six admitted for further observation, one patient, who had an initial negative CT angiography, ultimately underwent angiography with embolisation on Day 12 post-biopsy.
3.3 Timing of Complication
Of these 44 complications, 28 (64%) occurred within the first hour, 38 (86%) within the first 2 h, and 42 (95%) within the first 3 h. The vast majority, 38/44 (86%) of overall complications, occurred within the first 2 h (Figure 1).
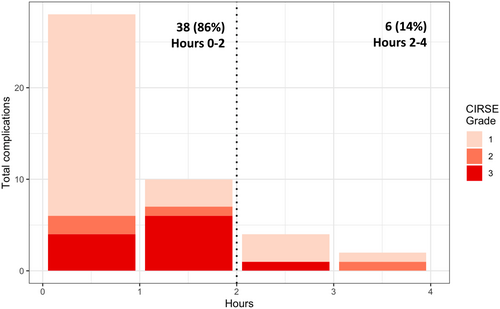
By 2 h, the cumulative incidence of complications was 11% (95% CI, 8%–15%), which rose to a total of 13% (95% CI, 10%–17%) over the remaining 2 h. This difference was comprised of 6 complications (6/332, 1.8% of all patients). Four were post-operative pain (all CIRSE Grade 1), managed with additional analgesia. Two were post-operative bleeding, both in outpatients undergoing non-targeted biopsy and requiring admission for further observation; one case of haematuria in a native kidney (CIRSE Grade 3), and one case of bleeding at the puncture site in a transplanted kidney (CIRSE Grade 2).
After reaching 2 h complication-free, the chance of developing a complication within the remaining 2 h dropped to 2% (95% CI, 1%–7%) (Table 4). That is, once a patient had passed the observation period of 2 h, they had a 98% (95% CI, 93%–99%) chance of completing the remaining 4-h observation period without experiencing a complication.
| CIRSE grade | < 1 h, N = 28a | 1–2 h, N = 10a | 2–3 h, N = 4a | 3–4 h, N = 2a | Overall, N = 44a | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1, N = 22a | 2, N = 2a | 3, N = 4a | 1, N = 3a | 2, N = 1a | 3, N = 6a | 1, N = 3a | 2, N = 0a | 3, N = 1a | 1, N = 1a | 2, N = 1a | ||
| Post-operative pain requiring commencement of additional analgesia beyond midazolam/fentanyl | 3 (14%) | — | — | 2 (67%) | — | 5 (83%) | 3 (100%) | — | — | 1 (100%) | — | 14 (32%) |
| Post-operative pain requiring new commencement of significant analgesia | — | — | 1 (25%) | — | — | — | — | — | — | — | — | 1 (2%) |
| Post-operative haemorrhage | 19 (86%) | 2 (100%) | 3 (75%) | 1 (33%) | 1 (100%) | 1 (17%) | — | — | 1 (100%) | — | 1 (100%) | 29 (66%) |
- a n (%).
3.4 Associations With Patient Factors
Patients who received biopsies under CT guidance were more likely to experience a late complication (i.e., between hours 2 and 4 of the observation period), compared to those performed with US (p = 0.035). This was the only subgroup based on patient demographics or biopsy-related variables observed to be at a higher risk of a late complication (Table 5).
| Complications | p | ||
|---|---|---|---|
| Late (2–4 h), N = 6a | Early (0–2 h), or none, N = 326a | ||
| Age at time of procedure | 52 (44, 58) | 63 (50, 72) | 0.12b |
| Gender | 0.2c | ||
| Female | 4 (67%) | 115 (35%) | |
| Male | 2 (33%) | 211 (65%) | |
| Admission status | 0.3c | ||
| Inpatient | — | 87 (27%) | |
| Outpatient | 6 (100%) | 239 (73%) | |
| Biopsy approach | 0.2c | ||
| Non-targeted | 4 (67%) | 114 (35%) | |
| Targeted | 2 (33%) | 212 (65%) | |
| Imaging modality | 0.035c | ||
| US | 1 (17%) | 202 (62%) | |
| CT | 5 (83%) | 124 (38%) | |
| Gauge of biopsy needle | 17 (16, 18) | 18 (16, 18) | 0.5b |
| Number of passes | 0.4c | ||
| 1 | 3 (50%) | 93 (29%) | |
| More than 1 | 3 (50%) | 233 (71%) | |
| Track closure | 2 (33%) | 97 (30%) | > 0.9c |
| Native kidney | 4 (67%) | 287 (88%) | 0.2c |
| Timing of last dose of anticoagulant or antiplatelet, n = 77 | > 0.9c | ||
| Within 24 h | — | 21 (28%) | |
| Longer than 24 h | 1 (100%) | 55 (72%) | |
- a Median (IQR); n (%).
- b Wilcoxon rank sum test.
- c Pearson's Chi-squared test.
3.5 Complications After 4 h Observation
Six complications occurred after completing the standard 4 h monitoring period without issue and having been either discharged or returned to routine observations on the inpatient unit; 3 (50%) of these were non-targeted studies. 4/6 (67%) of these complications were bleeding, 2/4 (50%) of which were inpatients.
There were three inpatient cases: one had ongoing pain with no further intervention, one had macroscopic haematuria which required imaging but no further intervention, and one had macroscopic haematuria requiring embolisation the next day.
There were three outpatient cases: one required analgesia for US-confirmed haematoma after 5 h, one presented 4 days later with ongoing pain requiring imaging but no further intervention, and one presented 5 days later with haematuria requiring imaging but no further intervention.
4 Discussion
Percutaneous, image-guided renal biopsies are an important investigation for sampling renal tissue in the assessment of focal renal lesions or diffuse renal disease [7]. However, renal biopsies can produce a variety of complications, from mild pain managed with simple oral analgesia to bleeding requiring blood transfusion, embolisation or, most severely, nephrectomy [8]. Prompt identification and management of complications are essential and usually identified during a post-procedural period of observation.
In our cohort of 332 biopsies, 44 (13%) complications occurred in the 4 h observation period. Fifteen complications were pain-related and managed with additional pain medication. Six of these patients also required a prolonged period of observation. The 29 remaining complications related to bleeding, either solely macroscopic haematuria (n = 2), peri-nephric haematoma (n = 25) or haemodynamic instability + haematuria/haematoma (n = 2). Ultimately, two patients required an angiogram with embolisation, and no patient required surgery/nephrectomy.
Our cohort consisted of both targeted (n = 214) and non-targeted (n = 118) image-guided biopsies; however, when analysing those subgroups separately, in the targeted biopsy group none had solely macroscopic haematuria, 15 (7%) patients had a peri-nephric haematoma, and none required transfusion and/or angiography. These numbers are comparable to the available IR literature on targeted renal biopsies [9, 10]. For the non-targeted group, the bleeding complication numbers are 2 (1.7%) frank haematuria, 10 (8.5%) peri-nephric haematoma and 2 (1.7%) haemodynamic instability, respectively. These compare favourably to the percentages reported in the 2018 KHA-CARI review [8] which consisted mainly of papers on biopsies performed by nephrologists. In our practice, non-targeted renal biopsies are predominantly performed by nephrologists. Patients who have either challenging anatomy/patient factors, have failed a biopsy by nephrology, or are considered high risk are referred for biopsy by Interventional Radiology. One can hypothesise that these would carry a higher complication risk; nevertheless, our complication rate overall is lower than reported by the work of Corapi et al., one of the only meta-analyses available regarding non-targeted renal biopsy complications, which estimates the rate of macroscopic haematuria as around 3.5% (95% CI, 2.2%–5.1%), and RBC transfusion 0.9% (95% CI, 0.4%–1.5%) [11].
The 2018 KHA-CARI guidelines, developed for nephrologists performing non-targeted renal biopsies, recommend a 6–8 h period of observation with same-day discharge for low-risk patients [7]. Evidence informing these guidelines was largely based on retrospective, observational studies; however, one RCT by Al-Hweish et al. showed no significant difference between complication rates in patients observed for 6 h versus 24 h of observation [12], and similar observational studies have shown little benefit in longer observational periods for low-risk patients [13-18]. Currently, 4 h of observation is used in our centre. This is more in line with Burke et al., who analysed practice amongst Australasian Nephrologists against the 2018 KHA-CARI recommendations, showing that the majority of centres that responded already observed patients for between 4 and 6 h (89.6%) [19].
The vast majority, 38/44 (86%) of overall complications occurred within the first 2 h. Six complications occurred between 2 and 4 h post-biopsy. Four patients required additional pain relief and could be discharged after the routine 4 h of observation; these were therefore, graded as CIRSE complication grade 1. The two remaining patients who had a bleeding complication after 2 h experienced bleeding at the puncture site and haematuria associated with clot retention: CIRSE complication grade 2 and 3, respectively. The patient with a CIRSE grade 3 complication was an outpatient who underwent a non-targeted renal biopsy of a transplanted kidney under CT guidance.
In the comparative group analysis, the use of CT guidance was independently associated with the development of complications after 2 h. The advantage of US guidance over CT guidance is real-time needle visualisation during the entire procedure. Although we did not specify operator experience for each biopsy, more inexperienced operators tended to prefer CT guidance over US guidance. Secondly, patient factors such as body habitus or location of renal lesions can determine the needle guidance modality. Factors such as anticoagulant/antiplatelet use, needle gauge, and tract closure were not associated with the occurrence or timing of complications.
Of the patients requiring additional pain relief, 4 started developing symptoms after the first 2 h of observation. All were discharged after a standard 4h observation. This observation has triggered the development of a standardised analgesic protocol for patients undergoing targeted and non-targeted renal biopsies at our institute. This may hopefully prevent re-presentation to the hospital should a shorter observation period be implemented.
Two out of 332 biopsies (0.6%) developed a bleeding complication between 2 and 4 h of observation (CIRSE Grades 2 and 3). Both complications occurred in patients undergoing a non-targeted renal biopsy. In order to safely free up recovery bed space, the observation period for non-targeted biopsies could remain at 4 h, and those patients undergoing targeted renal lesion biopsies only require a 2 h observation period to identify complications.
A reduced observation period leads to earlier mobilisation, something that historically has been associated with the risk of the development of bleeding complications [8]. Ishikawa et al., however, showed similar rates of bleeding between a cohort with gentle mobilisation following strict bed rest for 2 h, compared to 7 h with an abdominal bandage [20].
5 Limitations
Patients from a single institute were analysed, and both targeted and non-targeted renal biopsies were included. However, when comparing those groups separately, the occurrence of complications did not differ from published data. Biopsies were performed by either an Interventional Radiologist, Clinical Radiologist with subspecialty interest in Abdominal Radiology or a trainee radiologist with the supervision of the aforementioned. The exact level of experience and degree of supervision was not able to be determined due to the retrospective nature of this study.
While we included patients who presented to our network with complications after 4 h, we will not have been able to identify patients who subsequently presented to other hospitals.
While an aim of this study was to consider exceptions to an overall safe observation period, the low number of late complications overall has limited our ability to assess this. Similarly, for this reason, we did not compare biopsy positioning or biopsy indication—significant further questions in the field of kidney biopsy research.
6 Conclusion
Most renal biopsy complications occur within the first 2 h of observation. Complications after 2 h were mostly non-targeted biopsies and pain-related but also included one case of haematuria requiring admission, CIRSE Grade 3. These results suggest it may be possible to safely reduce observation times following image-guided renal biopsies, particularly for targeted renal biopsies and with the use of a standardised post-operative analgesic regime.
Acknowledgements
Open access publishing facilitated by Monash University, as part of the Wiley - Monash University agreement via the Council of Australian University Librarians.
Ethics Statement
Ethical approval was obtained from the local Human Research Ethics Committee (HREC), reference number: RES-23-0000-015Q, and the need for informed consent was waived.
Consent
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.