The role of demographic change in explaining the growth of Australia's older migrant population living with dementia, 2016–2051
The authors have stated they have no conflicts of interest.
Abstract
Objective: To examine the demographic drivers contributing to the future growth in the population of older migrants in Australia living with dementia.
Methods: Using birthplace-specific cohort-component projection models, we projected the number of older migrants living with dementia. ABS data on births, deaths, migration and birthplace were used, alongside Australian Institute of Health and Welfare (AIHW) estimates of dementia prevalence with birthplace dementia weights calculated from administrative data.
Results: The number of older migrants living with dementia is projected to increase from about 134,423 in 2016 to 378,724 by 2051. Increases in populations with dementia varied considerably, from a slight decrease for those born in Southern & Eastern Europe to over 600% increases amongst the South-East Asia, Southern & Central Asia, and Sub-Saharan Africa-born populations.
Conclusions: Cohort flow is the primary driver increasing the number of older migrants living with dementia. This growth is largely inevitable because the cohorts are already living in Australia as part of the migrant population, but currently at ages below 60 years.
Implications for public health: High relative growth and shifting birthplace composition in the number of migrants living with dementia poses implications for culturally appropriate care, health care access and workforce needs to support migrant families, carers and their communities.
Despite declines in the age-specific incidence of dementia in several high-income countries (HICs), some studies suggest dementia rates may be considerably higher among migrant groups compared to the non-migrant population.1, 2 In the Netherlands, the prevalence of mild cognitive impairment and dementia was found to be three to four times higher among the majority of non-Western immigrant groups than in the native Dutch population.2 In the UK, the number of people of Black, Asian and other Minority Ethnic origins living with dementia was estimated to rise by sevenfold by 2051, while the number of people living with dementia is expected to double.3 This difference is often attributed to demographic change; due to immigration and an associated increase in the proportion of older adults from culturally and linguistically diverse (CALD) backgrounds, as well as to the increased risk factors of dementia experienced by certain CALD population groups.4
Dementia is multifactorial so in addition to the presence of genetic risk factors such as APOE ∊4 (a gene linked to Alzheimer's type dementia), racial and ethnic differences in prevalence could be linked to multiple modifiable risk factors such as less education, hearing impairment, depression, low social contact, excessive alcohol consumption, traumatic brain injury, air pollution, and poor cardiovascular health (e.g. diabetes, obesity, smoking, hypertension, physical inactivity).1 Migrant groups may have greater co-presence of these risk factors because of intersections between race, ethnicity and the social determinants of health.5 For example, migrants and other minority populations may experience more frequent social stressors – such as discrimination - which may influence their risks of dementia in later life.6
In the context of population ageing, increasing birthplace heterogeneity and shifting English language proficiency in migrant-receiving high income countries like Australia, there is a need for dementia services to be more inclusive.7, 8 Dementia may be experienced differently by the individual migrants and their families and communities.9-14 Relative to non-migrants, migrants are less likely to receive messages related to prevention, more likely to be diagnosed at an advanced stage of their illness, and when diagnosed with dementia, less likely to be prescribed anti-dementia medication, use long-term care or have access to culturally appropriate services.4, 11, 15, 16 Enumerating differences between migrant groups and modelling for future demographic growth can aid in the development of interventions, therapeutics, and public policy to improve planning for dementia in future populations.
Despite this policy motivation and shifting demographic landscape, there is little information on future growth in the number of older migrants living with dementia, in addition to representative dementia prevalence rates by birthplace in Australia. The Australian Institute of Health and Welfare (AIHW) have produced regular projections for the total population17, 18 and others have produced detailed modelling of population level incidence and prevalence of dementia in the Australian population.19-23 Recent AIHW estimates suggest the number of Australians living with dementia may more than double between 2021 and 2058, from 386,000 to almost 850,000 respectively.24 Existing population-level evidence on dementia prevalence and incidence among culturally and linguistically diverse (CALD) Australians is rare. Indeed, in the only study examining future CALD dementia prevalence and incidence, the authors included neither heterogeneity in migrant prevalence rates nor the underlying demographic processes driving population ageing and growth.20 All of the above studies concord overall population projections with the official population projections produced by the Australian Bureau of Statistics (ABS) that are current at time of publication. This limits the ability to disaggregate the drivers of growth in the population living with dementia – into for example, shifting prevalence as opposed to specific demographic processes such as cohort flow or changes in life expectancy. In its latest 2020 report, the Australian Institute for Health and Welfare identified that the “lack of robust data on dementia among CALD communities, people with intellectual disabilities and other vulnerable populations” as one of the key data gaps on dementia in the country.25
The purpose of this paper is to examine the role of demographic drivers of change in the number of older migrants (60 years and over) living with dementia in Australia to mid-century. In the remainder of this paper, we first outline our birthplace-specific cohort-component model and data sources used to project and decompose the drivers of growth among migrant populations living with dementia to mid-century. Following a statement of our key results, we discuss the policy and practice relevance of our findings, alongside pointing to key data and modelling gaps that require amelioration.
Methods
Projections of Australia's migrant (overseas-born) populations with dementia aged 60 years and above were prepared for the period 2016 to 2051. The projections were calculated by first creating projections of Australia's population by sex, age and migrant group, and second, by applying dementia prevalence rates to the projected populations.
Population projections were calculated with a birthplace-specific cohort-component model using separate projection assumptions for each migrant population. Projections were produced by sex and single years of age for 47 migrant populations plus the Australia-born population in annual increments from 2016 to 2051. The launch year of 2016 for the projections was chosen because this was the latest year for which finalised Estimated Resident Populations by country of birth were available from the Australian Bureau of Statistics at the time of writing. The selected migrant populations consisted of both individual countries of birth for the largest 25 migrant populations in Australia and broader world region birthplace groupings for the rest. This selection of countries of birth represented a balance between capturing the heterogeneity of Australia's overseas-born population groups and limitations in the detail of some available demographic data inputs.
Apart from temporary COVID-related interruptions in the short run, projection assumptions about the long-term trajectories of fertility, mortality, and migration were all conservative in nature. International migration was expected to increase rapidly from the reduced flows of 2020 and 2021 and return to pre-COVID levels by 2025–26, while the slight drop in fertility as a result of economic uncertainties created by the pandemic was also expected to last only until 2025–26. All migrant groups were assumed to experience gradual increases in life expectancy, continuing long-run historical trends. Details of the population projection model equations and input data are available elsewhere.7, 26
Projections of the number of people living with dementia were calculated by multiplying prevalence rates by the population projections. The prevalence rates were estimated using three sets of data. These were:
- prevalence rates for the Australian population as a whole by sex and five year age group published by the Australian Institute of Health and Welfare17;
- prevalence ratios calculated from counts of persons living with dementia by birthplace collected as part of Aged Care Funding Instrument (ACFI) assessments; and
- prevalence ratios calculated from counts of persons living with dementia by birthplace collected as part of the Aged Care Assessment Program (ACAP).
Tabulations from the latter two administrative data sources were kindly provided to the authors by the Australian Institute of Health and Welfare (AIHW) through customised data requests.
Ratios of birthplace-specific to national dementia prevalence were calculated for both ACFI and ACAP data sources. Birthplace-specific prevalence rates by birthplace, age, and sex were then estimated by multiplying the national rates by the average of ACFI and ACAP ratios. The average of the two ratios was selected due to a lack of evidence favouring one data source over the other. The ACFI and ACAP data were supplied by ten broad birthplace groupings, so prevalence rates and dementia projections were calculated for those broad categories (countries of birth in Oceania (excluding Australia), North West Europe, Southern & Eastern Europe, North Africa & Middle East, South East Asia, North East Asia, Southern & Central Asia, Americas, Sub-Saharan Africa, plus Australia). Algebraically, the birthplace-specific dementia rate estimation can be summarised as:

where
p=dementia prevalence rate
s=sex
a=age group
b=broad birthplace grouping
Aus=Australia
AIHW=AIHW dementia prevalence rates
ACFI=ACFI-based dementia prevalence
ACAP=ACAP-based dementia prevalence
For the main set of projections, we assumed that the rates would remain constant through the 2016–2051 projection horizon. However, we also created an alternative ‘best case’ scenario in which prevalence rates decline exponentially by 1.5% per year from 2016 onwards. This rate of decline was selected because it falls between the dementia prevalence declines recorded by Harrison et al. for older people accessing long-term care and those accessing home care in Australia.27 This results in the projected prevalence rates in 2051 being just 59% of their value in 2016, a fall which would be consistent with an almost complete elimination of modifiable risk factors for dementia. Others have reported that 40–48% of dementia risk is regarded as modifiable.1, 28 While this represents a highly optimistic scenario, the purpose is to illustrate the effects of population ageing on the future numbers of people living with dementia in the context of rapid progress against its prevalence.
A decomposition of the projections was undertaken to reveal which influences contribute most to the projected increase in the numbers of people living with dementia over the 2016 to 2051 period. Growth is divided into contributions from: (1) birthplace-specific dementia prevalence (relative to national prevalence rates), (2) increases in life expectancy in the future, (3) gains to the population from net international migration, and (4) cohort flow, which refers to the entry of new cohorts into the 60+ age group from younger ages, and the depletion of older cohorts from mortality. The decomposition was calculated by running several analytical projection variants in which the selected factors were successively removed. First, the region-specific dementia prevalence rates were removed and replaced with national rates; then increases in life expectancy were removed and replaced with fixed mortality rates for the whole projection horizon; then net international migration gains were removed by setting all migration flows to zero. Any remaining growth over the 2016–2051 period is then the result of cohort flow.
Ethics approval for this project was granted by the Melbourne School of Population and Global Health Human Ethics Advisory Group (HEAG) – Ethics ID: 2021-22105y19137-2.
Results
Table 1 presents estimates and projections of the Australian population aged 60+ living with dementia by broad birthplace category. The older migrant population overall is projected to experience an increase from about 134,400 people living with dementia in 2016 to 378,700 by 2051, a substantial increase of 182% over 35 years. These numbers signify a rise in the proportion of people aged 60+ with dementia from 7.4% in 2016 to 9.9% by 2051. Although prevalence rates by age and sex are assumed constant throughout the projections, the age structure of the 60+ population will gradually become older so that there are proportionally more people in the very oldest ages where dementia prevalence rates are highest.
Increase, 2016–2051 |
||||||
|---|---|---|---|---|---|---|
Birthplace |
2016 |
2021 |
2036 |
2051 |
No. |
% |
Oceania North-West Europe Southern & Eastern Europe North Africa & Middle East South-East Asia North-East Asia Southern & Central Asia Americas Sub-Saharan Africa |
6,344 53,494 43,623 5,322 8,152 6,652 4,229 3,454 3,154 |
8,763 60,675 49,758 7,244 11,723 9,187 5,876 4,829 4,537 |
20,099 83,462 54,588 15,430 31,201 21,687 14,652 10,825 12,021 |
33,129 87,613 42,357 27,107 63,642 46,084 35,946 18,062 24,785 |
26,785 34,119 -1,266 21,785 55,490 39,432 31,717 14,608 21,631 |
422 64 -3 409 681 593 750 423 686 |
All overseas-born Australia-born |
134,423 203,567 |
162,593 231,626 |
263,965 376,632 |
378,724 542,306 |
244,302 338,739 |
182 166 |
Total population |
337,990 |
394,219 |
640,597 |
921,030 |
583,040 |
173 |
- Source: authors’ projections
Increases in dementia cases vary considerably between birthplace groups, from a slight decrease for those born in Southern & Eastern Europe to huge increases amongst the South-East Asia, Southern & Central Asia, and Sub-Saharan Africa-born. The broad-scale picture is one of migrant populations which largely arrived in Australia after the dismantling of the racist White Australia Policy in the 1970s experiencing larger percentage increases in dementia cases than the longer-established migrant populations from Europe.
Figure 1 illustrates the projected changes to the age-sex structure of the birthplace populations with dementia. For most populations there are large increases in dementia numbers projected for almost all age groups, particularly in the octogenarian and nonagenarian ages. The greater number of females living with dementia reflects more females than males in the population at the older ages, primarily due to lower mortality rates than males. The different picture shown for the Southern & Eastern Europe-born is the result of smaller and smaller cohorts entering the older ages over the next few decades due to earlier declines in immigration.
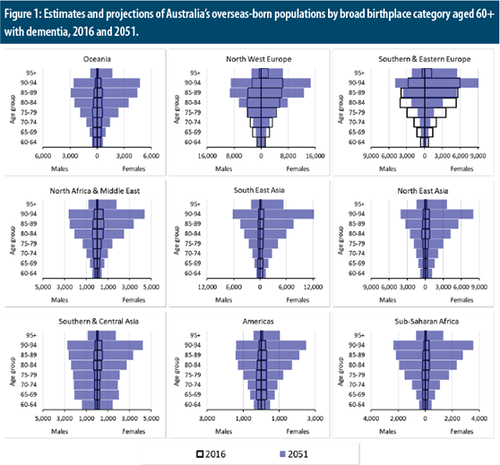
Estimates and projections of Australia's overseas-born populations by broad birthplace category aged 60+ with dementia, 2016 and 2051.
The decomposition analysis reveals which broad-level influences are driving the projected rise in dementia numbers. Table 2 reports growth multipliers for the key processes. The multipliers in the ‘total’ column are defined as ratios of projected dementia numbers in 2051 to estimated numbers in 2016 if national dementia prevalence rates applied to all birthplace populations. For each of the key processes the multipliers indicate the factor by which that process contributes to growth. For the older migrant population overall the growth multiplier is 3.10, indicating that the projected dementia numbers in 2051 are a little over three times the number they would have been in 2016 if national dementia prevalence applied to all birthplace groups. Region-specific dementia rates increase the numbers slightly (1.08), as does net international migration (1.03), while increasing life expectancy contributes more (1.20). However, by the far the largest contribution is from cohort flow (2.32), which refers to large net gains to the 60+ population over time as a result of large migrant population cohorts reaching age 60 over the course of the 2016–2051 projection horizon. This cohort flow is inevitable because the cohorts are already living in Australia as part of the migrant population, but currently at ages below 60.
Birthplace |
Region-specific dementia rates |
Increasing life expectancy |
Net international migration |
Cohort flow |
Total |
|---|---|---|---|---|---|
Oceania North-West Europe Southern & Eastern Europe North Africa & Middle East South-East Asia North-East Asia Southern & Central Asia Americas Sub-Saharan Africa |
1.02 1.08 1.17 1.12 1.14 1.04 0.97 1.16 1.08 |
1.27 1.25 1.18 1.17 1.14 1.21 1.25 1.09 1.18 |
0.87 1.08 1.10 1.15 0.97 0.94 1.05 1.04 1.18 |
4.85 1.23 0.74 3.62 6.82 5.90 6.42 4.71 5.60 |
5.42 1.79 1.12 5.46 8.54 7.01 8.21 6.17 8.47 |
All overseas-born Australia |
1.08 0.96 |
1.20 1.39 |
1.03 1.00 |
2.32 1.93 |
3.10 2.55 |
Total population |
1.00 |
1.31 |
1.01 |
2.07 |
2.75 |
- Source: authors’ projections
For most birthplace groups the contribution of cohort flow is dominant, though for those born in Southern & Eastern Europe cohort flow actually works to reduce dementia numbers. This is because the population currently consists of people primarily in the older ages; over the coming decades mortality from these cohorts will exceed the number entering the 60+ age group from younger ages. For the newer migrant populations of Australia, especially those born in Asia and Africa, cohort flow will be very considerable. Currently these populations are young with relatively smaller proportions in the older ages and most in the young adult and childhood age groups. Over time these large cohorts will age and enter the 60+ age group.
The dominance of cohort flow means that even non-trivial deviations from the projection assumptions for increasing life expectancy and net international migration would not alter the broad picture of our projections. Even in the extremely unlikely event of no further increase in life expectancy among the overseas-born and no international migration, the 2051 population aged 60+ with dementia would still be over 200,000 (with the growth multiplier being 1.08 × 2.32 = 2.52).
In the alternative set of projections with declining prevalence rates the projected growth in the number of people living with dementia at ages 60 and above is, as expected, more modest. Table 3 presents a summary of these alternative projections. The overseas-born population with dementia increases by 89,600 (or 67%) over the 2016–2051 period instead of 244,000 (182%). But the ranking of growth between the broad birthplace populations remains the same, with far more growth expected among the Asia-born and Sub-Saharan Africa-born migrant groups than the Europe-born populations.
Increase, 2016–2051 |
||||||
|---|---|---|---|---|---|---|
Birthplace |
2016 |
2021 |
2036 |
2051 |
No. |
% |
Oceania North-West Europe Southern & Eastern Europe North Africa & Middle East South-East Asia North-East Asia Southern & Central Asia Americas Sub-Saharan Africa |
6,344 53,494 43,623 5,322 8,152 6,652 4,229 3,454 3,154 |
8,130 56,291 46,163 6,721 10,876 8,523 5,452 4,480 4,209 |
14,890 61,830 40,439 11,431 23,114 16,066 10,855 8,019 8,905 |
19,597 51,828 25,057 16,035 37,648 27,261 21,264 10,685 14,662 |
13,253 -1,666 -18,567 10,713 29,496 20,609 17,035 7,231 11,508 |
209 -3 -43 201 362 310 403 209 365 |
All overseas-born Australia-born |
134,423 203,567 |
150,845 214,889 |
195,550 279,016 |
224,036 320,804 |
89,614 117,237 |
67 58 |
Total population |
337,990 |
365,734 |
474,566 |
544,840 |
206,850 |
61 |
- Source: authors’ projections
Table 4 presents growth multipliers for the alternative projections for the 2016–51 period. Only the cohort flow multipliers, which are substantially lower, are changed from the main set of projections. This is due to the effect of declining prevalence rates dampening the projected increase in the size of cohorts of people living with dementia over time. The life expectancy and overseas migration assumptions are the same as in the main set of projections.
Birthplace |
Region-specific dementia rates |
Increasing life expectancy |
Net international migration |
Cohort flow |
Total |
|---|---|---|---|---|---|
Oceania |
1.02 |
1.27 |
0.87 |
2.87 |
3.21 |
North-West Europe |
1.08 |
1.25 |
1.08 |
0.73 |
1.06 |
Southern & Eastern Europe |
1.17 |
1.18 |
1.10 |
0.44 |
0.66 |
North Africa & Middle East |
1.12 |
1.17 |
1.15 |
2.14 |
3.23 |
South-East Asia |
1.14 |
1.14 |
0.97 |
4.04 |
5.05 |
North-East Asia |
1.04 |
1.21 |
0.94 |
3.49 |
4.15 |
Southern & Central Asia |
0.97 |
1.25 |
1.05 |
3.80 |
4.86 |
Americas |
1.16 |
1.09 |
1.04 |
2.79 |
3.65 |
Sub-Saharan Africa |
1.08 |
1.18 |
1.18 |
3.31 |
5.01 |
All overseas-born |
1.08 |
1.20 |
1.03 |
1.37 |
1.83 |
Australia |
0.96 |
1.39 |
1.00 |
1.14 |
1.51 |
Total population |
1.00 |
1.31 |
1.01 |
1.23 |
1.63 |
- Source: authors’ projections
Discussion
The older migrant population overall is projected to experience an increase from about 134,423 people living with dementia in 2016 to 378,724 by 2051. However, increases in populations with dementia vary considerably between birthplace groups, from a slight decrease for those born in Southern & Eastern Europe to over 600% increases amongst the South-East Asia, Southern & Central Asia, and Sub-Saharan Africa-born. Even considering a very optimistic set of scenarios, in which dementia prevalence falls by 41% by mid century (‘best case’ scenario in which prevalence rates decline exponentially by 1.5% per year), the overseas-born population with dementia still increases by 89,600 (or 67%) over the 2016–2051 period instead of 244,000 (182%). Nonetheless, the ranking of growth between the broad birthplace populations remains the same, with far more growth expected among the Asia-born and Sub-Saharan Africa-born migrant groups than the Europe-born populations.
Our results are significant for HICs with a permanent migration program and large diaspora communities. In Australia's case, most health and aged care services are predominantly Anglo-centric with migrant-specific aged care services mainly directed at Southern European born older people.7, 26 However, with the rapid decline in these cohorts and the Asian-born dominance in older migrants by mid-century, services must plan now to effectively meet future need. This includes more targeted programming around dementia risk reduction, workforce planning, providing care in language, and developing models to support migrant families to deliver and sustain high-quality, culturally appropriate care at home.
First, by estimating dementia prevalence by migrant heterogeneity, mechanisms to culturally adapt existing evidence on dementia prevention can be established.29 Better targeting of specific communities is also possible. To date, risk reduction messaging targeted at older migrants has been inadequate. Asian and African migrant groups are particularly underrepresented, a shortcoming which leaves risk factors that are exacerbated in these communities unaddressed.30 For example, South Asians have a 1.5-2 times greater prevalence of CVD, higher risk of stroke, and four times the prevalence of diabetes compared to Caucasians, all of which put them at greater risk of experiencing related cognitive impairment and dementia.31, 32 It should be noted here that meta-analysis data on dementia risk factors are mostly derived from Europe and North America, and evidence from Australia remains relatively limited.33
Prevention is one side of the coin; care is the other. Concurrently, the migrant aged care workforce in HICs must be leveraged. Similar to the US, UK, and Canada, one in four care workers in Australia is a migrant.34, 35 Most are from Asia and Africa: between 2011 and 2016, there have been influxes from South Asia (333 percent increase) and sub-Saharan Africa (145 percent); care workers from India and Nigeria having increased by 389 percent and 204 percent respectively.36 These workers can offer more diverse cultural activities and language skills to older people with dementia as well as linking them, their carers, and aged care facilities to diverse ethnic communities.37, 38 Capacity to offer such services in language is critical given that aphasia, common in dementia, affects older migrants who tend to lose their non-primary languages first, followed by eventual loss of the primary language(s).39, 40 Leveraging a shared language is a crucial first step to establishing care relationships between older migrants with dementia and aged care workers, and as the dementia advances, facilitates the transition to non-verbal communications (e.g. embodiment, use of objects, physical environment).41
Cultural matching – i.e., the alignment of provider and patient cultural backgrounds – may also be achievable given our forecast demographic transitions. Cultural matching is a long-held preference among healthcare patients, especially those with language difficulties.42 Historically, it has been notoriously difficult to achieve at scale. However, it may be possible over time for Asian- and African-born migrants in Australia. Whether it will lead to improved dementia care outcomes is debatable as negative cultural perceptions of dementia have been widely noted among these communities and care workers from these groups.43 Therefore training and upskilling workers is integral to changing perceptions, lest existing stigmas be mutually reinforced.
Finally, noting the strong preference in migrant families for dementia care to occur at home,44 digital technologies to enhance dementia care are needed to support sustainable high-quality, culturally appropriate care at home. Via smartphones, tablets, and computers, family carers can learn in their own language and cultural context about dementia, prevention, and how to offer social support. In Australia, 20 million people (88% of the population) already use the internet, often spending >40 hour/week online and rate of digital inclusion are even higher in migrant communities (+2.8 points/national average).45, 46 Digital technologies, especially digital media, are therefore a crucial platform to improve dementia care in migrant families.
Our decomposition of growth in migrant populations living with dementia reveals region-specific dementia rates increase the numbers slightly (1.08), as does net international migration (1.03), while increasing life expectancy contributes slightly more (1.20). However, by the far the largest contribution is from cohort flow (2.32), which refers to large net gains to the 60+ population over time as a result of large migrant population cohorts reaching age 60 over the course of the 2016–2015 projection horizon. This cohort flow is inevitable because the cohorts are already living in Australia as part of the migrant population, but currently at ages below 60. This underscores the fact that even withstanding hypothetical reductions in the prevalence of dementia of up to 41% (the ‘best case’ scenario in which prevalence rates decline exponentially by 1.5% per year from 2016 onwards), cohort flow continues to increase the number of overseas born Australians living with dementia. Thus, due to the changing demography, increase in the number of this population with dementia is largely irreversible.
Limitations
Given the extant data environment, it is important to note the limitations of our study. The macrosimulation model did not adjust for education levels, CVD prevalence, and whether existing CVDs are being effectively managed; factors that will modulate dementia risk.1, 47 However, even assuming a 1.5% decline per year, dementia prevalence still increases by sheer weight of numbers. There are very few population level data sources on national level prevalence of dementia by birthplace in Australia. Estimation of birthplace-specific dementia prevalence via ACFI and ACAP administration data involves a number of approximations. Although we utilise ACFI and ACAP data to create weights of the migrant to Australian born dementia prevalence, it is important to recognise that these administrative data sources underestimate the total number of people living with dementia.48 Nonetheless, as our results indicate, cohort flow, rather than reasonable shifts in prevalence are the key drivers of the growth of dementia cases among migrant Australians, and the shifting cultural composition of dementia in Australia.
Improving the quality of routinely collected dementia data and ensuring cultural inclusivity/identification, along with conducting larger and more nationally representative or geographically diverse prospective studies, will be required to strengthen dementia prevalence estimates to better guide service planning and delivery for older migrant Australians. Notwithstanding this need for increased precision, high relative growth in the number of people living with dementia (regardless of prevalence levels) poses implications for culturally appropriate prevention and care, health care access and support for migrant families, carers and their communities.
Acknowledgements
The project was funded by the Australian Research Council's Centre of Excellence in Population Ageing Research (CE1101029).