Pediatric circumcision using n-butyl-cyanoacrylate plus MS monomer: Bacteriostatic and cosmetic advantages over suture
Funding information: This research received no specific grant from any funding agency in the public,commercial, or not-for-profit sectors.
The copyright line for this article was changed on 4 February 2021 after original online publication
Abstract
Purpose
The aim of this study is to compare the use of n-butyl-cyanoacrylate plus MS monomer (NBCA-MS) glue with suture in pediatric circumcision.
Materials and Methods
Between January 2013 and January 2017, 160 consecutive pediatric patients (range 18 months–14 years, mean 7.5 years) underwent circumcision. Eighty patients were randomly allocated to the glue group and 80 to the suture group. In the glue group wound margins were approximated by n-butyl-cyanoacrylate plus MS monomer (NBCA-MS) glue while in the suture group interrupted 5-0 polyglycolic acid stitches were used. Each group was randomized into two subgroups: forty patients (subgroup A) received antibiotics (6 days of amoxicillin/clavulanic acid) and 40 (subgroup B) patients did not receive any postoperative drug. Operative time, pain score, postoperative complications and cosmesis were statistically evaluated.
Results
The operation time was significantly higher in the suture group; pain severity and duration were not significantly lower in the glue group. In the 80 patients of the glue group no complications occurred; in the suture group 20 (25%) cases of wound edema and 6 (7.5%) infections occurred. Cosmesis evaluation 1 and 6 months postoperatively showed significantly better results in the glue group.
Conclusion
Our study demonstrates that NBCA-MS glue wound closure in pediatric circumcision is a safe and effective technique.
1 INTRODUCTION
The word “circumcision” comes from Latin circum (meaning “around”) and cœdere (meaning “to cut”), and consists in removing the penis foreskin (prepuce). It has been practiced since the Egyptian times and it is still one of the most common surgical procedures: in the United States, nearly 75% of male population has been circumcised for ethnic, religious or medical reasons.1-3 It has been widely proven that circumcised infants have a lower risk of urinary tract infections and balanoposthitis and seems to be a protective factor against sexual transmitted infections (STIs), such as human papilloma virus (HPV), herpes simplex virus (HSV)-2 and human immunodeficiency virus (HIV).4, 5 Morever, circumcision lowers the risk for penile cancer since predisponing conditions like phimosis, smegma, balanitis and HPV infection are uncommon.6 Meanwhile, according to other authors, there aren't randomized studies that could prove that rate of urinary tract infections (UTI) could be reduced by circumcision. The incidence and prevalence of most sexually transmitted diseases in western Europe cannot be significantly influenced by circumcision, assuming regular genital hygiene.7
Different techniques have been described in the literature; the most used are the “Plastibell”, the “sleeve resection”, the “squeeze” and the “guillotine” technique.8
Circumcision is a commonly performed operation and absorbable sutures have traditionally been used for closure. The two most common complications of circumcision are bleeding and wound infection,9 but also the penile adhesions after the surgery.10 Male circumcision had a relatively low incidence of adverse events overall, especially if the procedure was performed during the first year of life, but rose 10–20 fold when performed after infancy.11
The cyanoacrylate tissue glue has been claimed to have the advantages of being hemostatic,12 bacteriostatic13-17 and easy to use; moreover, the stitch marks along the suture lines can be avoided, allowing for better cosmetic results.
The aim of our prospective randomized study is to show advantages of using n-butyl-cyanoacrylate plus MS monomer (NBCA-MS) tissue glue compared to absorbable sutures in pediatric circumcision, with particular focus on bacteriostatic effect.
2 METHODS
All the patients were fully informed about the study and informed consent was obtained. The study was conducted from January 2013 to January 2017. Totally, 160 boys of 18 months to 14 years of age (mean 7.5 years) underwent elective circumcision because of ethnical/religious reason in 125 cases and for congenital and acquired phimosis in 35.
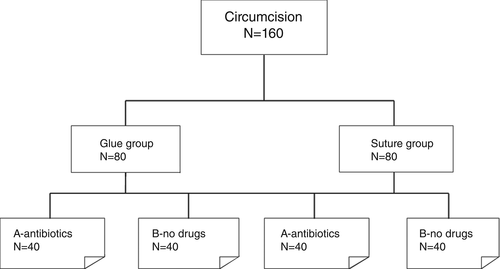
Eighty patients were randomly assigned to the experimental group (glue group) and 80 patients to the control group (suture group). No patient underwent pre-operative treatment nor ointment therapy. Each group was further randomized into two subgroups: 40 patients (subgroup A, mean age 7.2 years) received 6 days antibiotic therapy10 and 40 (subgroup B, mean age 7.8 years) did not received any postoperative drug (Figure 1). In subgroup A, 57 interventions were for ritual purposes, while 23 were for medical reasons (phimosis, paraphimosis, lichen, balanopostitis); in subgroup B 52 were rituals, while 28 were medical. The randomization timing we used was a mean of 12 days before the intervention (range 7–14 days).18
Postoperative antibiotic regimen included 6 days of amoxicillin/clavulanic acid (45 mg/6.4 mg/kg/d).
All patients were operated by the same surgeon under general anesthesia to avoid bias. After povidone iodine disinfection, the penis foreskin was placed in traction and the skin was incised with the cold-scalpel surgery technique along an imaginary line starting from the frenulum and coming obliquely down following the corona glandis penis; the skin was then separated from dartos by round-tip scissors and excised with part of the mucosal cuff. Meticolous hemostasis was ensured by bipolar cauterization.
In the control group the mucocutaneous approximation was done by polyglycolic acid 5-0 stitches in the traditional manner. In the experimental group, a 0.25 mL dose of n-butyl-cyanoacrylate plus MS monomer (NBCA-MS) glue chosen was Glubran2, a product of the Italian pharmaceutical company GEM Italy, which was used for wound closure; we used a linear glue application, drying in about 1 minute (it was clear when the glue surface opacified), which peeled spontaneously off in around 10 days. A damp gauze was used to protect the glans and the urethra to avoid accidental contact with the glue. Mucocutaneous approximation was achieved by using a pair of toothed forceps holding the two edges of wound firmly together. All patients were discharged the day after surgery with recommendation of daily iodine wound disinfection.
Postoperative pain was assessed after 4, 8 and 24 hours respectively, using Children and Infants Postoperative Pain Scale (ChIPPS).19
On the seventh postoperative day after circumcision, the wound was assessed for signs of infection (pain, swelling, fever, leucocytosis) bleeding and edema (highlighted by a swelling around, or just below the glandis); cosmetic outcomes were evaluated by a pediatric surgeon not participating the study, 30 and 180 days postoperatively.
Wound cosmesis was graded as poor, good or excellent, according to Visual Analog Scale (VAS) for scar evaluation.20
Categorical data were described by absolute and relative frequency whereas quantitative data by mean and standard deviation. To analyze qualitative variables as “postoperative pain” and “clinical events” related to the groups, chi square test (or Fisher's exact test when appropriate) and z-test for two proportions were applied. To compare continuous variables as “surgical case duration” and “time spent for sutureless circumcision” with the groups, t-test (two- tailed) was used.
A P-value less than .05 was considered statistically significant. All analyzes, descriptive and inferential, were performed by SPSS v.24 technology.
3 RESULTS
The comparison between the two groups shows a mean of surgical case duration of 20 minutes ± 1.5 (standard deviation, SD) when the suture were used whereas the mean time spent for sutureless circumcision was 14 minutes ± 1.3 (SD). This difference was found to be highly significant (P < .001).
Regarding postoperative pain, there was no significant reduction when glue was used (Table 1).
| After 4 h | After 8 h | After 24 h | ||||
|---|---|---|---|---|---|---|
| Score (ChIPPS) | 0 | 1+2 | 0 | 1+2 | 0 | 1 |
| Suture group | 75 | 5 | 76 | 4 | 78 | 2 |
| Glue group | 79 | 1 | 80 | 0 | 80 | 0 |
| P-value | .212 | .129 | .477 | |||
The comparison of complications using the cyanoacrylate and the suturing for wound approximation of circumcision is shown in Table 2. Wound assessment on the seventh postoperative day revealed 20 cases (25%) of edema occurred in the suture group (11 cases, 27.5%, in subgroup A and nine cases, 22.5%, in subgroup B) while no patient presented with wound edema in the glue group: this difference was statistically significant (P < .001 and P < .005, in the comparisons between the two data subgroups). No patients in either group, treatment or control, experienced wound bleeding or dehiscence. There are also significant differences between the percentage of infection in the suture-no drug group compared to the glue-no drug group (15% compared to 0%; P = 0.034), in fact six patients of the suture group, all previously randomized for not receiving postoperative antibiotics, showed serous wound discharge as a sign of infection, while conversely no infection occurred in the glue group.
| Suture Group | Glue Group | Suture group | Glue group | |||
|---|---|---|---|---|---|---|
| Clinical events | Drug | Drug | P-value | No drug | No drug | P-value |
| Edema | 11 (27.5%) | 0 (0%) | .001 | 9 (22.5%) | 0 (0%) | .005 |
| Bleeding | 0 | 0 | – | 0 | 0 | – |
| Wound dehiscence | 0 | 0 | – | 0 | 0 | – |
| Infection | 0 | 0 | – | 6 (15%) | 0 (0%) | .034 |
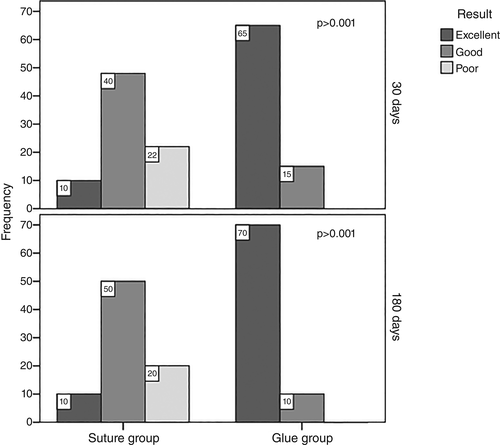
Thirty days after circumcision, the regularity of the wound edges and the overall cosmesis were better in the glue group; this difference was found to be highly significant (P < 0.001). Similarly, after 180 days cosmetic advantage of tissue glue was confirmed (Table 3). Moreover it is important to assess the fact that in our series the cost of intervention using the glue was cheaper than in the suture group; in fact 0.25 mL of Glubran2 (registered brand) cost 27 US dollars ($), against the $49.50 of the suture).
4 DISCUSSION
Traditionally, the circumcision wound is closed using interrupted absorbable suture;
currently, alternative methods are being proposed to overcome the shortcomings of the conventional closure like complications, postoperative pain, time consumed and cosmetic problems. The use of glue seems to solve all these issues providing greater aesthetic results,20-23 also the incidence of postoperative bleeding and hematoma formation in pediatric circumcision is reduced with the use of tissue glue.20
Cyanoacrylate is a liquid-adhesive monomer which polymerizes on contact with basic substances such as blood or water. The polymerization occurs at room temperature and does not require the use of solvent or an added catalyst.24-27
As already shown by Voznesensky et al. the use of glue can lead to a reduction in the operative time with beneficial economic effects;28 similarly in our work the sutureless technique allowed significant shortening of the time needed for surgery.
Moreover, tissue glue has an important haemostatic effect;29 in haemophilic patients the use of glue reduces the duration of clotting factor replacement after surgery, thus decreasing the high costs of treatment.30
Finally, bacteriostatic advantage of n-butyl-cyanoacrylate has been already stated in the literature,31, 32 and, to our knowledge, our study confirming the antimicrobical effects of NBCA-MS in a group of pediatric patients undergoing circumcision.
In the glue group, no infection occurred irrespective of the postoperative antibiotic therapy was administered or not, demonstrating a protective role of the n-butyl-cyanoacrilate against infections.
Avoiding the use of antibiotics is considerably favorable in pediatric patients, who dislike the administration of drugs by mouth as well as the application of local therapies for wound care.
In addition, avoiding the use of antibiotics helps to prevent bacterial resistance and unexpected adverse reactions.
5 CONCLUSION
In conclusion our study confirms that, in comparison with the traditional procedure, the sutureless technique with NBCA-MS for wound closure in pediatric circumcision allows to reduce the operative time, provides better cosmetic results and protects against infections.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest.