Vital sign measurements demonstrate terminal digit bias and boundary effects
Abstract
Objective
The measurement and recording of vital signs may be impacted by biases, including preferences for even and round numbers. However, other biases, such as variation due to defined numerical boundaries (also known as boundary effects), may be present in vital signs data and have not yet been investigated in a medical setting. We aimed to assess vital signs data for such biases. These parameters are clinically significant as they influence care escalation.
Methods
Vital signs data (heart rate, respiratory rate, oxygen saturation and systolic blood pressure) were collected from a tertiary hospital electronic medical record over a 2-year period. These data were analysed using polynomial regression with additional terms to assess for underreporting of out-of-range observations and overreporting numbers with terminal digits of 0 (round numbers), 2 (even numbers) and 5.
Results
It was found that heart rate, oxygen saturation and systolic blood pressure demonstrated ‘boundary effects’, with values inside the ‘normal’ range disproportionately more likely to be recorded. Even number bias was observed in systolic heart rate, respiratory rate and blood pressure. Preference for multiples of 5 was observed for heart rate and blood pressure. Independent overrepresentation of multiples of 10 was demonstrated in heart rate data.
Conclusion
Although often considered objective, vital signs data are affected by bias. These biases may impact the care patients receive. Additionally, it may have implications for creating and training machine learning models that utilise vital signs data.
Key findings
- Normal (i.e. in range) values are overrecorded in heart rate, oxygen saturation, and systolic blood pressure data, indicating statistically significant recording bias influences vital signs measurement.
- Other numerical biases, including even number bias, exist in heart rate, respiratory rate, blood pressure but not oxygen saturation data.
Introduction
Vital signs, or clinical observations, provide critical information to healthcare practitioners. These parameters, such as heart rate (HR), respiratory rate (RR), oxygen saturation (SpO2) and systolic blood pressure (SBP), are traditionally evaluated periodically by staff in general medical wards. Observations are widely considered to be objective indicators of an individual's physiological status.1 However, biases may affect these vital signs. Identifying and evaluating these biases is important not only to ensure adequate care escalation but also for medical research.2
Several biases have been demonstrated in the collection and recording of vital signs. The frequency of vital signs recording – particularly SpO2 – may be influenced by racial bias.3 Furthermore, for SBP, terminal digit preference for multiples of 10 (also known as ‘round number bias’) has been observed previously.2, 4, 5 Other anomalies have been observed, including an overreporting of temperatures of 36.0°C, especially for older patients, patients of Asian descent and patients measured during the first observational round of the day.2 Even number bias – a preference for numbers divisible by 2 – has been observed for HR and RR.2
Outside of medicine, it has also been shown that humans may demonstrate numerical biases when boundaries are set upon numbers (known as ‘boundary effects’).6 Typically, values inside a desirable reference range (such as a lower tax bracket) are more likely to be recorded. In economics, this phenomenon is referred to as ‘bunching’.7 Many hospitals employ rapid detection and response (RDR) or similar observation charts that use vital signs to inform clinical escalation, either in the frequency of subsequent observations or nursing/medical assessment. These parameters in such charts are based upon deviation from a statistical norm for the adult population.8 These charts create artificial boundaries that may predispose measurements to boundary effects. Published histograms have indicated the possible presence of this effect in SpO2 data,2 although this effect is yet to be specifically investigated.
The present study aimed to evaluate for biases in the distribution of observations for a diverse inpatient cohort. In particular, it aimed to: (i) evaluate whether there was evidence of boundary effects, as it relates to RDR chart thresholds, in recorded observations; and (ii) examine whether there was evidence of terminal digit bias in recorded observations.
Materials and methods
Participant recruitment and data collection
This retrospective cohort study included patients admitted to general medicine and acute medical units at a tertiary hospital over 2 years (from 1 March 2020 to 1 March 2022). All recorded values for selected vital signs (HR, RR, SpO2 and SBP) were collected from electronic medical records. Cases with none of the specified recorded vital signs were excluded.
The most common methods for recording vital signs in this hospital are observation for RR, non-invasive automatic blood pressure cuffs for SBP and HR, and associated pulse oximetry monitors for SpO2. However, manual blood pressure cuffs or pulse evaluation may sometimes be employed. Nursing staff most commonly collect vital signs. Data on the use of manual/automatic observations were not available.
Data analysis
The data were analysed using a non-parametric method for assessing boundary effects adapted from the counterfactual polynomial method discussed by Kleven.9 A flexible polynomial of order 810 was fitted to the data histogram. Extreme vital signs values were excluded to leave points in the following ranges: 20–160 for HR; 70–220 for SBP; 80–100 for SpO2; and 0–50 for RR. Points around the boundaries of reference ranges (where boundary effects may be expected) were added as separate terms to assess for differences against the rest of the distribution. For HR and SBP, a ‘window’ of two points on either side of each target point was also excluded.9 RR and SpO2 used ‘windows’ of 1 and 0, respectively. Additional linear terms were added to the distribution for all multiples of 2, 5 and 10 to assess for terminal digit bias for even numbers, multiples of 5 and round numbers. For SpO2, the analysis for boundary effects and terminal digit bias was conducted separately due to the small range of data. Data S1 provides further detail on the analysis and these values. Descriptive statistics are also presented, with either mean with standard deviation (SD) or median with interquartile range (IQR). All data analysis occurred on R version 2023.06.2 using default libraries.
Ethical approval
The present study received institutional human research ethics committee approval with a waiver of individual consent. CALHN Human Research Ethics Committee approval number: 16860.
Results
Patient characteristics
There were 15 734 individual visits included in the study, including 11 746 unique patients. The mean age was 69.6 years (SD 18.7 years) and 7715 were female (49.0%). A total of 2 724 782 measurements of the target vital signs were recorded. A total of 749 941 HR, 644600 RR, 757726 SpO2 and 572 515 SBP measurements were recorded. The mean HR was 81.2 beats per minute (SD 15.9), mean RR was 18.9 breaths per minute (SD 3.4), median SpO2 was 96% (IQR 95–98) and mean SBP was 127.5 mmHg (SD 21.1).
Heart rate
HR measurements demonstrated terminal digit preference for multiples of 2, 5 and 10 and boundary effects at the high (100) and low (60) margins of the normal range as specified by the RDR chart (Fig. 1a). HRs of 60 (P < 0.001) and 99 (P < 0.001) – each at the boundaries of the ‘normal’ range – were over-recorded. Even numbers were 26.1% more likely to be recorded than odd numbers (P < 0.001). Similarly, multiples of 5 were 22.8% more likely to be recorded (P < 0.001). In addition to the two above effects, multiples of 10 were 12.9% more likely to be recorded (P = 0.005).
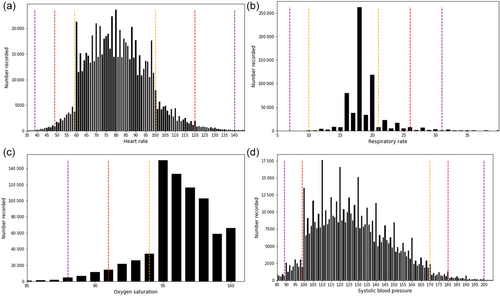
Respiratory rate
RR measurements demonstrated no boundary effects, including at 20, the upper boundary of normal (P > 0.1). This observation is validated by the symmetry of the distribution as RRs of 19, 20 and 21 have similar frequencies compared to rates of 17, 16 and 15 (Fig. 1b). There is a strong even number bias with a 93.5% overrepresentation of even numbers (P < 0.001) (Fig. 1b). No bias for multiples of 5 (P > 0.1) or 10 (P > 0.1) was observed.
Oxygen saturation
SpO2 demonstrated a boundary effect at 95% (P = 0.003) (Fig. 1c), corresponding to the lowest possible number prior to the threshold for escalation of monitoring. There were no round number, even number or other terminal digit biases (P > 0.1).
Systolic blood pressure
SBP recordings demonstrated terminal digit biases and boundary effects (Fig. 1d). Even numbers were 18.8% overrepresented (P < 0.001), and multiples of 5 were 34.9% overrepresented (P < 0.001). There was no independent preference for multiples of 10 in addition to the above two effects (P > 0.1). SBPs of 100 (P < 0.001) were overrepresented, corresponding to the RDR boundary where SPBs under 100 require additional monitoring frequency. Boundary effects around 170 and 180 were not observed independently of terminal digit bias (P > 0.1) (note, peaks at these values are still present on the histogram due to the terminal digit bias described above).
Discussion
The present study has shown that HR, SpO2 and SBP recordings exhibit boundary effects. In certain instances, values within predefined ranges were more likely to be recorded than out-of-range values. These results suggest a bias favouring the recording of in-range vital signs. While these data are often collected with automatic equipment, fluctuations when observing a continuous parameter (e.g. SpO2) may allow for the introduction of bias as only one number is recorded out of a series. These boundary effects, irrespective of the reason for their presence, have clinical and research implications.
While the present study has identified the presence of boundary effects, it cannot identify the reason for this phenomenon in this setting. The extent to which these boundary effects are conscious or unconscious cannot be determined by the present study. For example, it could be hypothesised that the observed boundary effects could in part be linked to operant conditioning,11 where persons measuring vital signs are disadvantaged by recording out-of-range values (e.g. due to consequences following a recording, such as colleague-feedback or the requirement to escalate monitoring frequency). It could be hypothesised that such patterns may be linked with high demands on nursing and/or medical staff. Alternately, these boundary effects may also be a response to the clinical judgement of the person recording vital signs: if the requirement for additional monitoring conflicts with a practitioner's determination of health status, they may be subconsciously or consciously inclined to record a ‘normal’ vital signs result. Accordingly, this effect may be a manifestation of incorrectly positioned vital sign cutoffs. The presence of boundary effects indicates certain patients are not receiving the recommended care escalation as defined by the local RDR chart, which has uncertain implications for clinical outcomes.12
Even number bias was also present in HR and SBP measurement. A terminal digit preference for multiples of 5 was observed in HR and SBP data. An independent preference for multiples of 10 was only observed for HR data. It is worth noting that the concomitant presence of a preference for even numbers and multiples of 5 results in an overrepresentation of multiples of 10 even if no independent effect was observed (see Fig. 1d).
The present study continues prior research regarding even number bias and other terminal digit preferences. The presence of even number bias across HR, RR and SBP may be a consequence of methods used for measurement. For example, a common method of measuring HR and RR is to count for 30 s and then multiply the result by 2 – this approach inherently results in even numbers being recorded. Many manual SBP gauges are only reliable to the nearest even number, contributing to even number overrepresentation in this measurement. It was uncertain what proportion of SBP measurements was conducted manually or with a machine in the electronic medical record data collected. Preferences for multiples of 5 (as observed for HR and SBP) and multiples of 10 (as observed for HR) may have a less mechanistic explanation. There is evidence to suggest that humans inherently subconsciously prefer multiples of 5 and 10.13 Terminal digit biases in vital signs, while perhaps less likely to affect care escalation, may have implications for the use of health data in research settings. In particular, machine learning models that do not account for this bias when learning from human-collected data may perform poorly when given data free from such biases (for example, via wearable telemetry and oximetry).
A strength of the present study was that, aside from SpO2, multiple possible biases were assessed simultaneously. This method allowed a more valid attribution of boundary effects and terminal digit bias to the effects themselves. For example, a boundary effect at a SBP of 170 mmHg was excluded as insignificant because biases favouring multiples of 2 and 5 accounted for its overrepresentation. However, some boundary effects may have been invalidly enhanced by interventions titrating to a particular vital sign (e.g. giving supplementary oxygen to achieve a SpO2 above 95%). Other biases not accounted for in the present study may also affect the validity of the above conclusions.
It should also be noted that the present study, while in a large and diverse patient cohort, was conducted at a single centre. It is therefore possible that the biases observed are contributed to by local factors. Studies in other diverse centres would improve the external generalisability of these findings. The data used in the present study were retrospective. In addition, the present study did not evaluate the clinical impact of these biases, nor did it assess the possible effect of clinical interventions on the vital signs observed.
Future research may seek to evaluate factors associated with these biases, such as whether these biases in observations are more common at times of reduced staffing. Research may also evaluate strategies to mitigate these biases, including using real-time continuous observation monitoring with electronic devices or increased staffing. Evaluation for numerical biases in other aspects of medicine, including the recording of patient weights and medication dosing, may be useful.
Competing interests
None declared.
Open Research
Open access publishing facilitated by The University of Adelaide, as part of the Wiley - The University of Adelaide agreement via the Council of Australian University Librarians.
Data availability statement
Data available on request due to privacy/ethical restrictions.