Geographic context of black-white disparities in Medicare CAHPS patient experience measures
Funding information
The research in this article was supported by the Centers for Medicare & Medicaid Services’ Office of Minority Health (Contract HHSM-500-2016-00097G).
Abstract
Objective
To examine whether black-white patient experience disparities vary by geography and within-county contextual factors.
Data Sources
321 300 Medicare beneficiaries responding to the 2015-2016 Medicare Consumer Assessment of Health care Providers and Systems (MCAHPS) Surveys; 2010 Census data for several within-county contextual factors.
Study Design
Mixed-effects regression models predicted three MCAHPS patient experience measures for black and white beneficiaries from geographic random effects, contextual fixed effects, and beneficiary-level case-mix adjustors.
Principal Findings
Black-white disparities in patient experiences were smaller in counties with higher average patient experiences. Black-white disparities in patient experiences were not associated with county-level poverty or racial segregation. However, county racial segregation and some measures of poverty were significantly associated with all beneficiaries’ level of health care access. Getting Needed Care scores were higher with greater racial segregation, while Getting Care Quickly scores were lower with higher poverty and racial segregation.
Conclusions
Efforts to reduce black-white disparities in patient experiences should focus on areas with low average patient experiences. Attempts to reduce disparities in timely access to health care should target primarily black, low-income, and racially and economically segregated areas. Positive associations of racial segregation with accessing needed care were unexpected.
1 INTRODUCTION
Racial/ethnic disparities in patient experiences are well-established,1-3 and studies indicate multiple potential sources of black-white disparities in patient experience at various levels in the health care process. These include factors such as provider bias,4 differences in patient characteristics such as health and health literacy,5, 6 and health systems’ organizational elements including cultural competency and proportion of minority patients.7, 8
The location of patients and health care services may also play a role, as patients may receive very different care based on attributes of where they live.9 Numerous studies find links between geographical contexts and racial/ethnic differences in patient care and outcomes. For example, vignette studies of provider decision making find disparities in physicians’ information-seeking behavior, diagnosis, and treatment recommendations for black patients in the United States versus the United Kingdom.10, 11 U.S. studies have documented that racial differences in testing, hospitalizations, and surgical procedures vary dramatically by region.9, 12, 13 Furthermore, studies of the Medicare population show that regional variation in racial disparities in medical treatment persists even after controlling for patient age and gender.9, 14
Prior research has primarily focused on whether the patterns of inequities in health and health care are linked to geographic contexts such as racial and income segregation. These studies have found positive associations between black-white residential segregation and black-white disparities in diagnosis, treatment, and outcomes (for a review, see Kramer, Hogue15 and Williams, Collins16). For instance, compared to less racially segregated areas, residentially segregated black patients are even more likely than their white neighbors to receive late-stage cancer diagnoses,17 have high-risk surgeries at low-quality hospitals,18 and experience higher mortality rates.19 While much less research has examined variation in black-white disparities by income segregation, studies indicate that disparities are worse in high-poverty areas.20-23 Unfortunately, little research has been devoted to disentangling the role of poverty versus racial segregation in health disparities.24
While much research has explored the link between geographical contexts and racial disparities in a variety of health care processes, there is a dearth of research examining whether contexts play a role in the extent of black-white differences in patient experiences. Black-white disparities in patient experiences persist in many health care settings.1, 8 Contexts such as county-level quality of patient experience or the relative size of or segregation of minority and poor populations could shape inequities in patient experiences via several pathways that involve race, place, poverty, and health care quality. Better understanding of these pathways has implications for housing policy, banking and lending policy, and other practices that have contributed to creating and sustaining racial and poverty segregation.
There are several mechanisms by which county-level average quality of patient experience may relate to black-white disparities. Areas with above-average overall patient experiences may have higher-quality providers with better access to health care innovations (eg, technologies that improve scheduling and wait times). However, these higher-quality providers may tend to disproportionately serve white patients,25 which may exacerbate racial inequities. In contrast, black-white disparities may be smaller in these areas due to greater adoption of practices such as cultural competence approaches that may improve all patients’ experiences and in particular the experiences of racial/ethnic minorities.8
Areas with high levels of poverty and racial minority populations may also experience larger black-white disparities in the quality of patient experiences. Residents in economically disadvantaged communities may have less access to high-quality and sufficiently resourced health care options. Racial/ethnic minorities, particularly blacks, have a long history of constrained residential choices that have restricted them to disadvantaged areas.26 These areas struggle to attract and retain high-quality health care institutions, professionals, and specialists.20, 27, 28 health care services in these areas are often overburdened because they serve sicker populations with limited funding, staffing, and medical equipment.29-31 Furthermore, health care institutions in disadvantaged areas may also lack training in cultural competency and in resources to be able to equally serve black and white patients.32 Even within the same geographic area, black patients are more likely to be cycled into lower-quality health care institutions.18
Areas characterized by high levels of segregation are also characterized by several factors that affect residents’, particularly black residents’, health status and access along with an area's ability to attract health care facilities and professionals. Racially and economically segregated areas experience higher housing instability,33 poorer education and health,34, 35 and higher unemployment and crime rates.36, 37 Additionally, racial differences in mistrust of health care and resulting lower use of health services38 could be exacerbated by segregation, particularly racial, by reducing opportunities for alternative, positive attitudes toward the medical establishment.
Together, these findings suggest that geographic contexts could contribute to racial disparities in patient experiences. To investigate this possibility, we test whether several types of geographical contexts—county average level of patient experiences, population proportion of black and of low-income residents, racial segregation, and poverty segregation—are associated with black-white disparities in patient experiences measured by the Medicare Consumer Assessment of health care Providers and Systems (MCAHPS), a national survey of Medicare beneficiaries’ patient experiences.
Two policy trends have brought increasing attention to understanding and mitigating racial/ethnic disparities in health care, including patient experience. The first is the shift from volume-based to value-based payment where patient receipt of care, patient outcomes, and/or patient experiences are tied to provider payment. This may be accompanied by providers taking on risk, such as through accountable care organizations. The second, related trend is a renewed interest in understanding and responding to social determinants of health.
This study contributes to the literature by exploring whether racial disparities in patient experiences differ by geographical contexts such as segregation. We also extend prior studies of segregation and racial/ethnic disparities in health care by examining multiple dimensions of geographic context, including composition (proportion of non-white or low-income residents) and segregation. While race and income are deeply intertwined,39 relatively few prior studies have attempted to distinguish the roles of poverty and racial segregation in racial health care disparities.15 Therefore, this study seeks to explore the potentially independent effects that economic and racial segregation can have on racial disparities in patients’ experiences.
2 METHODS
2.1 Data sources
Our analysis merged data from two datasets. The first is the Medicare CAHPS Survey, using Medicare Advantage (MA) and fee-for-service (FFS) data from the 50 states and DC. We pooled data for survey years 2015 and 2016 to increase sample size and reliability of estimates. Response rates were 39 percent and 36 percent for years 2015 and 2016, respectively. CAHPS surveys were administered by mail with telephone follow-up of mail nonrespondents. Potential respondents were selected using a stratified, random sample of Medicare beneficiaries with contracts (MA) or states (FFS) as strata. We restricted the sample to beneficiaries who self-reported their race as non-Hispanic black or non-Hispanic white and whose age was 65 years old and over. Non-Hispanic white and non-Hispanic black are hereafter referred to as white and black, respectively. We classified race/ethnicity based on two survey questions: one about race (white, black, Asian, Native Hawaiian or other Pacific Islander, and American Indian or Alaska Native) and the other regarding Hispanic/Latino origin. We classified all beneficiaries who identified themselves as Hispanic, regardless of race, as Hispanic and classified non-Hispanic respondents who selected multiple racial categories as multiracial. Among non-Hispanic respondents who selected a single race, those who selected only black or white were retained and classified accordingly. Our sample ultimately included 29 014 black and 292 286 white respondents.
The second dataset is the 2010 Census from which county measures of population by race and income and measures of poverty and racial segregation were derived for all U.S. counties.40 These data were merged by respondents’ county of residence.
2.2 Dependent variables
Using the MCAHPS surveys, we calculated three composite measures of patient experience: Getting Needed Care, Getting Care Quickly, and Doctor Communication. See Table S1 for composite items. We chose CAHPS measures because they are the most widely used and best-validated U.S. measures of patient experience. The composites’ reliability and validity are described elsewhere.41, 42 We excluded measures such as customer service that were centralized health plan functions and were therefore unlikely to be related to beneficiaries’ local residential addresses. We did not use the ratings of care and providers (0-10 scale) because racial/ethnic groups may interpret these scales differently, and thus, comparisons by racial groups may not be valid.43 In contrast, based on a randomized vignette experiment, there is evidence that black and white respondents use response scales similarly for CAHPS composites.44
2.3 Independent variables
County-level racial and poverty population proportions and segregation measures were derived from the 2010 Census. To disentangle the potential effects of living in a disproportionately poor or black county from a living in a county with high internal segregation, we first measured each county's proportion of residents who self-identified as non-Hispanic black and the proportion of residents in households with incomes below the federal poverty level (FPL). These county-level proportions, which by themselves reflect poverty and racial segregation between counties, were distinguished from residential segregation by Census tract within counties. In what follows, we refer to the microlevel within-county segregation as “within county.”
We measured poverty (poor-nonpoor) and racial segregation (black-white) using two forms of residential segregation: dissimilarity and isolation indexes. This resulted in four measures for each county: black-white dissimilarity, black-white isolation, poor-nonpoor dissimilarity, and poor-nonpoor isolation. We considered beneficiaries who reside in households with incomes below 100 percent of the FPL to be poor. This income threshold is appropriate for Medicare beneficiaries.45 All segregation measures were created using Reardon's “seg” package in Stata.46 See Table S2 for segregation measure equations. While we measured both poverty and racial segregation, we describe dissimilarity and isolation indexes using county black-white segregation as an example below.
Dissimilarity, the more commonly used measure in segregation analyses, assesses how far from equal the distribution of black and white residents is across an area. It is constructed from census tract and county population data. Dissimilarity can be interpreted as the proportion of black residents who would need to move to another tract to evenly distribute black residents across tracts within a county. Dissimilarity within a county is higher when the variance of tract proportions of black residents is higher.
We also measured isolation, another common segregation index, which can be interpreted as a black resident's isolation from whites based on a black resident's probability of randomly encountering another black resident in their residential area. Isolation at the county level not only is positively related to variance in tract proportions of black residents but is also positively related to the mean tract proportion of black residents.
Both segregation indices are scaled from 0 to 100 whereby 0 indicates no residential segregation and 100 indicates complete residential segregation. While the two measures are related, they are mathematically and conceptually distinct. For an example, consider the evolution of northern U.S. urban areas. Prior to the Great Migration of blacks from the rural south, the black population in northern areas was small and lived in just a few neighborhoods. Dissimilarity was therefore high as black residents were clustered together, but their isolation was low because they lived in primarily white neighborhoods. With the Great Migration, the black population increased in a few neighborhoods, which left dissimilarity levels the same but increased black isolation as there were relatively fewer white residents with whom to interact. The “white flight” of the 1950s resulted in some neighborhoods that were virtually exclusively black or virtually exclusively white, a point at which black-white dissimilarity and black isolation are at their maximum, 100.
2.4 Other covariates
To account for other characteristics that may affect patient experiences and use of the patient experience scales, we included the following individual-level variables as case-mix adjusters: age, education, general health, mental health, proxy assistance to complete survey, and low-income indicators (dually eligible for Medicare and Medicaid, receipt of the Medicare low-income subsidy). To control for potential coverage differences, we included an indicator variable of MA vs FFS. To adjust for geographic variation in health care availability, we measured dearth of health care professionals using partial and whole county indicators of health professional shortage areas (HPSAs) in primary care. Partial HPSA county indicators identify counties where only part of the county is classified as a HPSA. We also measured whether a county is urban using a metropolitan statistical area (MSA indicator). To account for potential differences across years, we controlled for survey year.
2.5 Statistical analyses
All analyses used person-level poststratification weights that account for sample design and nonresponse by matching weighted sample and enrolled populations in each contract by county combination on sex, age, race/ethnicity, Medicaid eligibility/low-income subsidy status, Special Needs Plan enrollment, and zip-code level distributions of income, education, and race/ethnicity.47, 48
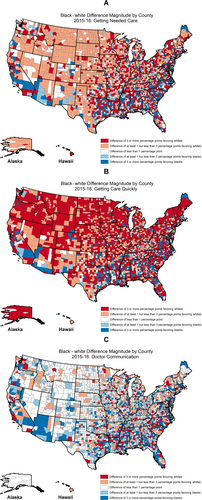
To depict the degree of black-white disparities in patient experience by county, we calculated the difference in adjusted mean scores for black and white beneficiaries for each county. Using a map of the United States, we then plotted these differences by percentage point for each county (Figure 1A-C).
2.6 County average level of patient experience models
Our first set of models estimated whether a county's black-white disparities for a patient experience are associated with the county's average level of patient experience. In our base models, we used mixed-effect models that predict patient experience from a black indicator, fixed-effect case-mix adjusters, and random effects for county and the interaction between county and black, using an unstructured covariance matrix so that we could estimate slope-intercept correlations. Using this approach, the county random effect indicates the county's overall performance, while the interaction between county and being black random effect captures the county's black-white disparity.
After estimating the base models, we added predictors measuring county-level race and poverty population proportions and segregation to test whether the slope-intercept correlation between a county's level of patient experience and its black-white disparity changes after accounting for racial and poverty contexts.
To illustrate how black-white disparities in patient experience relate to the county average level of patient experience, counties were classified into quintiles by their overall average adjusted patient experience. Within each quintile, we calculated and plotted mean black and white patient experience scores. The mean scores were calculated from the slope-intercept correlation models that did not include the county-level race and poverty predictors. All correlations from mixed-effect models are disattenuated correlations, so sampling error does not bias them toward zero.
2.7 County poverty/racial population proportion and segregation models
Our second set of analyses used mixed-effects regression models to estimate each patient experience measure using the key predictors of county racial and poverty segregation and population proportions of black residents and of residents living below FPL. This approach let us assess whether poverty and racial geographic contexts are associated with patient experience. We interacted these key predictors with the individual-level black indicator to test whether the black-white disparity differed systematically by these county-level contextual factors.
3 RESULTS
As shown in Table 1, at the county level, white beneficiaries’ adjusted mean composite scores of Getting Needed Care and Getting Care Quickly were slightly higher than blacks’, while mean scores for Doctor Communication were approximately the same for both groups. However, black beneficiaries’ ranges of scores were much larger than whites’. In terms of segregation, counties generally had low levels of poverty and racial segregation, on average, with values less than 30.0; racial dissimilarity was moderate with an average value slightly above 30.0 but well below 60.0.49 Ranges of racial segregation were greater than poverty segregation.
| Mean | St. Dev. | Min | Median | Max | |
|---|---|---|---|---|---|
| Dependent variables | |||||
| CAHPS composites | |||||
| Getting Needed Care | |||||
| Adjusted white mean | 88.44 | 1.77 | 77.82 | 88.57 | 94.01 |
| Adjusted black mean | 86.35 | 5.87 | 28.94 | 86.38 | 106.66 |
| Adjusted black-white difference | −2.09 | 6.04 | −62.43 | −2.03 | 17.03 |
| Getting Care Quickly | |||||
| Adjusted white mean | 72.80 | 3.91 | 48.80 | 73.06 | 86.26 |
| Adjusted black mean | 69.79 | 6.94 | 17.73 | 70.20 | 98.06 |
| Adjusted black-white difference | −3.02 | 6.43 | −54.96 | −3.18 | 29.68 |
| Doctor Communication | |||||
| Adjusted white mean | 91.01 | 1.62 | 76.88 | 91.18 | 96.51 |
| Adjusted black mean | 91.04 | 3.48 | 55.73 | 91.05 | 100.26 |
| Adjusted black-white difference | 0.03 | 3.97 | −35.35 | 0.03 | 16.69 |
| Independent variables | |||||
| Percent black | 8.93 | 14.53 | 0.00 | 2.00 | 85.70 |
| Percent in poverty | 16.74 | 6.20 | 3.10 | 15.90 | 50.10 |
| Racial segregation | |||||
| Black-white dissimilarity | 31.25 | 17.46 | 0.00 | 30.61 | 84.39 |
| Black-white isolation | 14.88 | 19.82 | 0.00 | 4.57 | 88.97 |
| Income segregation | |||||
| Poor-nonpoor dissimilarity | 18.13 | 10.66 | 0.00 | 17.64 | 53.70 |
| Poor-nonpoor isolation | 19.18 | 7.33 | 0.00 | 18.46 | 53.54 |
| Percent of counties | |
|---|---|
| Primary care health provider shortage area | |
| No shortage | 13% |
| Partial county | 61% |
| Whole county | 26% |
| Live in metropolitan statistical area (MSA) | |
| No | 62% |
| Yes | 38% |
- Notes: County-level adjusted means are from mixed models with fixed effects for black and case-mix adjustment and random effects for county and interaction term black × county. Adjusted survey weights were used to fit models. All variables are on a 0-100 scale.
Figure 1A-C visually illustrate the county distribution of case mix adjusted black-white differences in each patient experience measure. As shown, Figure 1A,B demonstrate better patient experience for white than black beneficiaries in most counties for Getting Needed Care and especially for Getting Care Quickly. In contrast, black and white beneficiaries reported similar patient experience regarding Doctor Communication in most counties. CAHPS differences of less than 1 point on a 0-100 scale are considered very small, those of 1-3 points are considered “small,” and those of 3 points or more are considered “medium” or “large.”50, 51
3.1 County average level of patient experiences models
Table 2 shows the results of base models estimating the association between county-level patient experience scores and black-white disparities in patient experiences for each patient experience measure. The first column shows the average adjusted difference between black and white beneficiaries. The negative point estimates indicate that black beneficiaries reported significantly worse experiences accessing care than whites. Black and white beneficiaries reported similar experiences with Doctor Communication.
| Average county-level black-white PE difference | County-level correlation of black and white PE | Correlation of black-white disparities and overall county-level PE | ||||
|---|---|---|---|---|---|---|
| Est | SE | P-value | Est | Est | P-value | |
| Getting Needed Care (n = 229 428) | −2.09 | 0.51 | *** | 0.05 | −0.20 | 0.004 |
| Getting Care Quickly (n = 305 240) | −3.02 | 0.47 | *** | 0.13 | −0.14 | 0.007 |
| Doctor Communication (n = 275 123) | 0.03 | 0.29 | 0.09 | −0.36 | <0.001 | |
- ***P < 0.001.
The second column displays the correlation between scores for black and white beneficiaries in the same county. The low correlations of black and white experiences by county (0.05 to 0.13) suggest that black-white disparities in scores varied markedly by county (P < 0.001 for the interaction of county and black for all three measures).
The third column shows the correlation between black-white disparities and overall patient experience levels within the county. The statistically significant negative correlations indicate that black-white disparities in patient experiences were smaller in counties with higher patient experience levels. These results were unchanged when we added the key geographic context predictors: within-county poverty and racial segregation and population proportions (data not shown).
Figure 2A-C graphically illustrate the relationship between county-level overall patient experience and black-white differences in patient experience calculated at each quintile of the patient experience measure. As depicted, black-white disparities were smaller in counties with higher overall patient experience levels. This convergence occurred across the full range of performance for Getting Needed Care and Getting Care Quickly, but the convergence of Doctor Communication only reflected a wider gap in the lowest quintile than in other quintiles.

3.2 County poverty/racial population proportion and segregation models
Table 3 shows the results of mixed-effects regression models estimating the associations between the key geographic context predictors and black-white disparities in patient experience. Contrary to our hypothesis, we found no statistically significant relationships between any of the key indicators and black-white disparities in scores, as tested by the interactions between black indicators and geographic contexts. In addition, we did not find significant associations between poverty or racial segregation and experiences with Doctor Communication.
| Model 1 | Model 2 | Model 3 | Model 4 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Est | SE | P-value | Est | SE | P-value | Est | SE | P-value | Est | SE | P-value | |
| Getting Needed Care (N = 229 344) | ||||||||||||
| Black (0 = white) | −2.974 | 1.418 | * | −2.546 | 1.423 | −1.936 | 1.289 | −3.220 | 2.007 | |||
| County population proportion | ||||||||||||
| Black | 0.029 | 0.007 | *** | |||||||||
| Below FPL | 0.016 | 0.017 | ||||||||||
| Segregation | ||||||||||||
| Racial dissimilarity | 0.015 | 0.006 | * | 0.017 | 0.006 | ** | ||||||
| Black × racial dissimilarity | 0.000 | 0.034 | ||||||||||
| Income dissimilarity | −0.007 | 0.011 | −0.004 | 0.012 | ||||||||
| Black × income dissimilarity | 0.009 | 0.061 | ||||||||||
| Racial isolation | 0.017 | 0.005 | *** | 0.016 | 0.005 | ** | ||||||
| Black × racial isolation | −0.023 | 0.024 | ||||||||||
| Income isolation | 0.006 | 0.015 | 0.005 | 0.015 | ||||||||
| Black × income isolation | 0.016 | 0.071 | ||||||||||
| Getting Care Quickly (N = 305 141) | ||||||||||||
| Black (0 = white) | −2.181 | 1.275 | −3.163 | 1.268 | * | −1.265 | 1.156 | −2.087 | 1.835 | |||
| County population proportion | ||||||||||||
| Black | −0.120 | 0.009 | *** | |||||||||
| Below FPL | −0.330 | 0.021 | *** | |||||||||
| Segregation | ||||||||||||
| Racial dissimilarity | −0.017 | 0.008 | * | −0.006 | 0.008 | |||||||
| Black × racial dissimilarity | 0.019 | 0.031 | ||||||||||
| Income dissimilarity | 0.048 | 0.014 | *** | 0.019 | 0.014 | |||||||
| Black × income dissimilarity | 0.050 | 0.056 | ||||||||||
| Racial isolation | −0.058 | 0.007 | *** | −0.059 | 0.007 | *** | ||||||
| Black × racial isolation | −0.018 | 0.022 | ||||||||||
| Income isolation | −0.116 | 0.019 | *** | −0.116 | 0.019 | *** | ||||||
| Black × income isolation | 0.006 | 0.066 | ||||||||||
| Doctor Communication (N = 275 040) | ||||||||||||
| Black (0 = −white) | −0.221 | 0.801 | 0.068 | 0.796 | −0.100 | 0.724 | −0.289 | 1.140 | ||||
| County population proportion | ||||||||||||
| Black | −0.001 | 0.005 | ||||||||||
| Below FPL | −0.015 | 0.012 | ||||||||||
| Segregation | ||||||||||||
| Racial dissimilarity | 0.002 | 0.005 | 0.003 | 0.005 | ||||||||
| Black × racial dissimilarity | 0.009 | 0.020 | ||||||||||
| Income dissimilarity | −0.004 | 0.008 | −0.005 | 0.009 | ||||||||
| Black × income dissimilarity | 0.002 | 0.035 | ||||||||||
| Racial isolation | −0.001 | 0.004 | −0.001 | 0.004 | ||||||||
| Black × racial isolation | 0.004 | 0.014 | ||||||||||
| Income isolation | −0.005 | 0.011 | −0.005 | 0.011 | ||||||||
| Black × income isolation | 0.014 | 0.041 | ||||||||||
- *P < 0.05, **P < 0.01, ***P < 0.001.
Population proportion of black residents and racial segregation were statistically significantly associated with health care access (Getting Needed Care, Getting Care Quickly) scores (P < 0.05), but in opposing directions for the two measures of access. In counties with greater racial segregation and/or higher proportions of black residents, all beneficiaries’ reports of Getting Needed Care were higher on average (main effect of racial dissimilarity in Models 1 and 2, of racial isolation in Models 3 and 4, and of county proportion black in Model 1). However, we see the opposite relationship with Getting Care Quickly (main effect of racial dissimilarity in Model 1, of racial isolation in Models 3 and 4, and of county proportion black in Model 1). We note that racial dissimilarity had an independent association with health care access after controlling for the relative size of the black population (Model 1).
Poverty segregation only had a statistically significant relationship with Getting Care Quickly. Like racial segregation, poverty isolation (main effect in Models 3 and 4) and the population proportion of residents below the FPL (Model 2) had a negative relationship with Getting Care Quickly, while poverty dissimilarity had a positive relationship (Model 1). However, poverty dissimilarity's relationship was much smaller and no longer significant once we controlled for a county's population proportion of below-FPL residents, which also demonstrated a significant negative relationship with Getting Care Quickly (Model 2).
Both poverty and racial contexts retained their associations with Getting Care Quickly when included in the same model, suggesting separate associations with beneficiaries’ timely access to care.
4 DISCUSSION
While many studies have found evidence that local area residential contexts shape health processes and outcomes, few have investigated their role in patients’ experiences, particularly racial disparities in these experiences. We found evidence that several types of geographic contexts were associated with patient experiences in general, but only a county's overall quality of patient experience was associated with black-white disparities. Furthermore, the relationship between geographic context and patient experience differed across patient experience measures.
We found that counties’ overall levels of patient experience were associated with black-white disparities. While both white and black beneficiaries’ patient experiences were worse in counties with poor overall patient experiences, black-white disparities were greatest in these counties, which indicated that blacks’ care experiences were particularly poor. While all patients do worse when faced with low-quality health care, these results echo previous findings that minority patients are often more negatively affected.8
The results also suggest that both racial and poverty residential contexts shape patient experiences, but in different ways. First, we found no evidence that these contexts affected beneficiaries’ experiences communicating with doctors; this is consistent with several studies that found little or no black-white disparities in beneficiaries’ ratings of Doctor Communications.3, 52, 53
Second, health care access measures (Getting Needed Care and Getting Care Quickly) were related to a county's racial composition and segregation, but in opposing directions: while beneficiaries reported better access to needed care in disproportionately black and racially segregated counties, they also reported less timely access to care. Similarly, we found that beneficiaries reported less timely access to care in counties with more residents living below the FPL than counties with more residents living above the FPL. It should be noted that disproportionately poor and black counties reflect segregation at a macrogeographic level (concentration of poor and black residents in certain counties), whereas the direct measures of segregation we employ reflect microgeographic segregation-segregation by Census tracts within counties.
Some of these relationships were unexpected since we hypothesized a negative relationship between disproportionately black, racially segregated, and economically disadvantaged counties and access to care due to difficulties attracting sufficient high-quality health care resources, including hospitals.20, 27-31 We also found evidence that racial segregation, in addition to racial composition, may affect health care access. This echoes foundational arguments by Wilson39 and Massey, Denton26 that racial segregation is a distinct organizational structure of communities that shapes residents’ life chances. Similarly, our results suggest that poverty and racial segregation may have independent roles: poverty and racial segregation are both negatively related to Getting Care Quickly, suggesting particular difficulties for residents in counties affected by both contextual factors.
Unexpectedly, we found that counties’ poverty and racial residential context were not related to black-white disparities in patient experiences. This suggests that the magnitude of black-white disparities in beneficiaries’ experiences does not systematically differ for beneficiaries who (a) live in affluent and primarily white areas compared to (b) those who live in areas that are disproportionately black and/or segregated by poverty and race. These findings are contrary to much of the research on segregation and racial health disparities, which finds that black patients often have poorer health care and health outcomes than whites when residential segregation is greater.16, 54 However, in contrast, Wilson-Frederick et al55 found that, although disparities in physical inactivity favoring whites over blacks existed at the national level, blacks and whites in the same communities experienced similar rates of physical inactivity. Similarly, Thorpe et al56 found that black men reported rates of preventive screening tests similar to or greater than white men when living in the same community.56 This suggests that health care access in segregated areas is an insufficient explanation for black-white disparities in health care quality and health outcomes.
Further research is needed, since this is the first study to our knowledge that examines the potential role of poverty and racial segregation in variations in black-white disparities in patient experiences. Future research should include younger populations to investigate whether similar patterns persist when access to health insurance is not universal as it is in Medicare. Additional health care quality measures should also be incorporated into models to explore potential mechanisms behind these patterns. Prior research with younger, commercially insured respondents finds no black-white differences in scale use.44 However, if poorer beneficiaries experience worse pre-Medicare health insurance than more affluent beneficiaries, the contrast might influence their expectations of care.
Our study has three primary limitations. First, geographic contexts were measured at the county level. Using smaller areas such as Census tracts may reveal different results. Second, response rates were modest, so nonresponse bias may have influenced our findings. However, research on CAHPS surveys has found little evidence of nonresponse bias after adjustment for case mix.57, 58 Third, county racial and economic makeup could have substantially changed over the 5-6 years between when Census and CAHPS data were collected. Thus, CAHPS respondents’ patient experiences may have been shaped by different geographical contexts than captured in the 2010 Census. However, estimated correlations between each segregation measure in 2010 and in 2000 at the county level were at least 0.90, suggesting that most counties’ racial and economic composition change little over 5-6 years relative to one another. To the extent that this generally small difference was unsystematic, it would cause small amounts of attenuation, resulting in slight underestimates of the true strength of association between Census characteristics and patient experience.
Despite these limitations, our study adds to the large literature examining the contributions of geographic contexts to racial health care disparities by examining their association in a particular health care realm, patient experiences. We found that counties with better overall patient experience had the smallest black-white disparities. Our results also suggest that, while primarily black and racially segregated counties may offer protective benefits to beneficiaries in terms of access to necessary care, health care institutions struggle to provide timely access in these areas, including those also characterized by poverty.
A large literature finds that black-white disparities in health care processes and health outcomes rise with racial and economic segregation.54 However, this is the first study of which we are aware to explore segregation effects on patient experiences and one of the few studies to test the joint effects of poverty and racial segregation, which has several implications for care interventions. One implication is that improvements should target beneficiaries, particularly black patients, in areas with low care quality. Efforts to expand cultural competence may improve care for all groups and reduce disparities at a relatively modest cost.8 In addition, interventions should also focus on improving timely access to care both in primarily black and poor areas and in areas with poverty and racial segregation. For example, the Centers for Medicare & Medicaid Services’ (CMS) Office of Minority Health offers technical assistance to health plans and providers to help improve their ability to identify and develop interventions to reduce racial disparities in access to care.59 In another initiative, CMS and the National Quality Forum created a measure development framework for using telehealth to deliver care, with potential to reduce disparities in access to care and patient experience.60 While these interventions, such as increases in staff and hours or investment in telehealth may be costly, efforts that target at-risk populations living in more segregated areas may be important parts of closing the disparities in patient experiences. This may be particularly important given the recent shift in the reimbursement system from volume-based to value-based care, in which providers are being paid based on patient outcomes, including patient experience with care.
ACKNOWLEDGMENTS
Joint Acknowledgment/Disclosure Statement: The research in this article was supported by the Centers for Medicare & Medicaid Services’ Office of Minority Health (Contract HHSM-500-2016-00097G). All authors declare no conflict of interest. However, please note that Shondelle Wilson-Frederick and Sarah Gaillot are employees of the sponsoring agency. The authors would like to thank Biayna Darabidian, BA for help with preparation of the manuscript. No Other Disclosures.
CONFLICT OF INTERESTS
All authors declare no conflict of interest. However, please note that Shondelle Wilson-Frederick and Sarah Gaillot are employees of the sponsoring agency.