The Mental Health Effects of the First Two Months of Lockdown during the COVID-19 Pandemic in the UK*
Submitted June 2020.
The authors are grateful to the ESRC-funded Centre for the Microeconomic Analysis of Public Policy (ES/M010147/1) for funding this research and to the UK Data Service for data and access. This work has been supported by the Nuffield Foundation via the IFS Deaton Review, ‘Inequality in the Twenty-First Century’ (reference WEL/43603). The Understanding Society COVID-19 study is funded by the Economic and Social Research Council and the Health Foundation. Fieldwork for the survey is carried out by Ipsos MORI and Kantar. Understanding Society is an initiative funded by the Economic and Social Research Council (ESRC) and various government departments, with scientific leadership by the Institute for Social and Economic Research, University of Essex. The data are distributed by the UK Data Service. The authors are also grateful to Richard Blundell, Rachel Griffith, Paul Johnson, Robert Joyce and Andrew Oswald for their helpful comments on this paper. Responsibility for the analysis and interpretation of the data, and any errors, is the authors’ alone.
Abstract
In this paper, we estimate the effects of the COVID-19 pandemic on mental health in the UK. We use longitudinal micro data for the UK over the period 2009–20 to control for pre-existing trends in mental health and construct individual-specific counterfactual predictions for April 2020, against which the COVID-19 mental health outcomes can be assessed. Our analysis reveals substantial effects at the population level, approximately equal in magnitude to the pre-pandemic differences between the top and bottom quintiles of the income distribution. This overall effect was not distributed equally in the population – the pandemic had much bigger effects for young adults and for women, which are groups that already had lower levels of mental health before COVID-19. Hence inequalities in mental health have been increased by the pandemic. Even larger effects are observed for measures of mental health that capture the number of problems reported or the fraction of the population reporting any frequent or severe problems, which more than doubled. Pre-existing health vulnerabilities had no predictive power for subsequent changes in mental health.
I. Introduction
From the outset, it has been clear that the potential mental health effect of the COVID-19 pandemic, and the lockdown and social distancing that were imposed in response to it, was going to be one of the most important aspects of the crisis. Mental health and subjective well-being outcomes are important in their own right, and they are also risk factors for future physical health and longevity1 so will be an indication of the future indirect health consequences of the pandemic. In addition, mental health and well-being will influence and drive a number of other individual choices, behaviours and hence outcomes.
The impact of COVID-19 on mental health has been identified as an important area of research going forward,2 and a number of papers have pointed out that mental health considerations should be an important element of decisions regarding at what speed and in what way to lift the lockdown and social distancing restrictions that have been imposed.3
Early indicators from cross-sectional studies or bespoke online COVID-specific surveys have already shown lower levels of subjective well-being and higher anxiety in the UK population than those observed in the last quarter of 20194 and that these changes are being sustained through the weeks of the lockdown and social distancing albeit with some small and gradual improvement.5 Similar findings have emerged for other countries using a variety of different data sources and methodologies such as internet surveys,6 helpline data7 and narrative methods based on Google trends search data for the UK, Italy and Sweden.8
Our primary contribution is to exploit newly available data on a pre-existing national longitudinal sample and construct a model of prior trajectories of mental health in order to identify an individual-specific counterfactual level of mental health in the absence of the pandemic. With this in hand, we show that the effects of COVID-19 on mental health in the UK are substantial and are greater for women. In addition, we use our models to show that the effects are also much greater for the young, and hence particularly for young women. These results are in line with emerging studies in other countries that exploit spatial variation to show large mental health effects of the pandemic in Japan,9 Germany10 and Italy.11 The Japanese study also investigates gender differences and shows that effects are greater for women than for men, but none of these studies considers differential effects by age.
Our use of detailed individual-level survey data also allows us to go further and show that only a relatively small part of the disproportionate effect on women and young people can be explained by differential economic and health impacts of the pandemic on these groups. Finally, we show that effects for all groups are greater when we consider measures designed to capture the number of mental health problems or the proportion of the population reporting any problems ‘much more than usual’ as opposed to a more generic indicator of the average level of mental health.
We document and analyse the individual-level effects of the pandemic on mental health using longitudinal data from the Understanding Society study12 in order to look at the distribution of individuals’ mental health outcomes in the context of their pre-pandemic trajectories.13 Since the latest publicly available pre-pandemic data for the Understanding Society sample are already somewhat dated14 and since there are important pre-existing trends in mental health by age, year and month of interview, it is important that we do not attribute all changes between waves to the pandemic itself. Thus, in our analysis, we create a simple individual-specific counterfactual prediction of the likely level of mental health in April 2020 in the absence of the pandemic, based on the trajectories previously observed for that respondent and changes in (observed) personal circumstances between the latest pre-pandemic wave and February 2020. We then compare the actual April 2020 observation with that prediction and discuss how this changes the results in comparison with looking at the raw differences between the most recent Understanding Society wave and the April 2020 observation. Finally, we look briefly at trends in subcomponents of the mental health measure on an item-by-item basis in order to provide suggestive evidence on some of the key mechanisms involved.
The main outcome measure we use in this analysis is the 12-item Generalised Health Questionnaire (GHQ-12) measure of mental health, distress and well-being,15 which is a commonly used indicator, although somewhat broader and more non-specific than would be ideal if one wanted to study specific mechanisms underlying changes in individual mental health conditions such as depression, anxiety or stress. The main advantage of the GHQ-12, however, is that since it is a relatively brief 12-item scale it has been collected in all waves of Understanding Society to date and was also included in the COVID-19 module.16
In keeping with the other ‘real-time’ evidence on mental health that has already emerged in the UK, the Understanding Society COVID-19 data indicate a sizeable deterioration in mental health, and this is true regardless of whether or not (and if so how) we control for recent pre-crisis trends. The average GHQ-12 score (indicating poor mental health) rose by 10.8 per cent between wave 9 and the COVID module, and the ‘effect’ of the crisis was a deterioration of 8.1 per cent when taking into account pre-crisis trends. This average deterioration (of one point on the 36-point GHQ scale) is large, being of a magnitude roughly equivalent to the mean difference in GHQ scores between the top decile and the bottom decile of the income distribution in 2017–18, nearly double the rise in average GHQ scores in total over the last four waves of the pre-pandemic data. We also show that this overall deterioration was driven by more reported problems, and a higher fraction of problems being reported ‘much more than usual’ (which we refer to as ‘severe’ for the purposes of this paper), as opposed to just mild deteriorations in existing problems for all. The number of problems reported rose by one – an increase of roughly 50 per cent – and the fraction of the sample reporting at least one severe problem doubled from 10.2 per cent to 23.7 per cent. Our individual-level analysis shows that these average effects arose from much-greater-than-average changes for women and for young adults, with some groups (particularly older men) being relatively unaffected.17 The magnitude of the effects for the 16–24 age group (a deterioration in GHQ-12 score of 1.8 points and a rise in the average number of problems of 0.8) is particularly striking and a considerable cause for concern.
The size of these age and gender effects depends on how we control for pre-crisis trends but they are relatively unaffected when we add more idiosyncratic factors to our model in order to control for the individual-level exposure to the effects of the pandemic. Other things equal, key workers had less of a deterioration, and those who were laid off, had young children or had COVID symptoms on the day of the interview had a greater deterioration. There was no evidence of statistically significant differential effects of other factors such as the respondent's pre-existing health vulnerabilities, employment or furlough status, marital status or region of residence. This is despite the fact that, with a sample size of nearly 12,000 observations, we would have a good degree of statistical power to pick up potential effects.
Our results also show clearly that, in addition to impacting on mental health on average, the COVID-19 pandemic has widened mental health inequalities, with the groups that had the poorest mental health pre-crisis also having had the largest deterioration. Qualitatively, this conclusion is obtained regardless of whether one uses past data in their raw form or attempts to control for pre-crisis trends, and indeed this is also unsurprising given what is already known about the deterioration in mental health for specific groups from the pre-existing cross-sectional analysis. In our framework though, we are able to quantify the increase in prevalence, and the increase in between-group inequalities, taking into account individual heterogeneity and with some control for the trends that would have happened anyway.
In addition to showing that some groups were more affected than others, and that the magnitude of these (relative) effects depends on how one controls for pre-crisis trends, we also provide some concluding analysis of the individual elements of the GHQ-12 questionnaire to show that some dimensions of mental health were affected more than others, and by more for some groups than others. We show that whilst measures relating to general happiness deteriorated for all age groups, trends in other dimensions are particularly negative for and/or specific to young adults.
We discuss our data and methodology in Section II, present our results in Section III and draw our conclusions in Section IV.
II. Data and methodology
We use panel data from the UK Household Longitudinal Study (UKHLS), also known as Understanding Society. The study began in 2009 and included 36,000 individuals in the latest wave (wave 9). Interview waves span three overlapping years, with the vast majority of interviews taking place in the first two years, so that wave 1 runs from 2009 to 2011, wave 2 from 2010 to 2012 and so on. Adults aged 16 or older in each household are re-interviewed approximately one year apart, including individuals who move addresses or leave their original households to form new households. The sample is weighted to be nationally representative.
In April 2020, participants of the UKHLS were asked to complete a short online survey on the impact of the COVID-19 pandemic. This survey included the GHQ-12 instrument as well as information on demographics and economic conditions in February 2020 (just before the start of the pandemic) and in April 2020. Full details of sample design, response rates and response patterns are given in Institute for Social and Economic Research (2020). There were 17,452 responses to the survey, and the response rate for individuals previously interviewed at wave 9 was 46.0 per cent.18 After dropping cases without wave 9 information that we need for our pre-crisis analysis and other cases with zero weight (N = 4,506) and dropping cases with missing responses to the GHQ-12 scale (N = 966), we are left with a resulting analysis sample of 11,980 individuals.
We consider three measures of mental health based on the GHQ-12. The first two are the overall GHQ score (the Likert scale) and the number of components with a score of 3 or above (the caseness scale), which are both conventional measures in the literature. In addition, we create a binary indicator of whether any of the components has a score of 4, i.e. if a negative item is reported to be a problem ‘much more than usual’ or a positive item is reported ‘not at all’. We use all three measures to help understand whether the trend in the average score (captured by the Likert measure) is a result of mild trends across all items for all individuals, or of trends in the number of problems reported or the number of severe problems for some people in particular. The caseness measure captures the number of problems reported and our additional measure (which we refer to, simply for brevity, as the presence of ‘severe’ problems) is our best attempt at capturing the proportion of the population with particularly acute problems. Full details of the individual items, and the way they are coded, are given in Appendix B, which is available online.
In order to help interpret the magnitude of our results and understand the units of our key dependent variables, Table 1 presents descriptive statistics for the GHQ-12 measures in the most recent pre-pandemic wave (wave 9). Mean GHQ scores were 11.4 for the sample as a whole, with a difference of around one point on average between men and women and between the top and bottom quintiles of the income distribution. The average number of problems reported was 1.83, although the median number of problems was zero. Far fewer (11 per cent of the total sample) reported ‘severe’ problems, i.e. any problems much more than usual.
| GHQ score | Number of problems | Any severe problems | |
|---|---|---|---|
| 10th percentile | 6 | 0 | 0 |
| 25th percentile | 7 | 0 | 0 |
| 50th percentile | 10 | 0 | 0 |
| 75th percentile | 13 | 2 | 0 |
| 90th percentile | 19 | 7 | 1 |
| Mean (all) | 11.40 | 1.83 | 0.11 |
| (5.60) | (3.12) | (0.32) | |
| Subgroup means | |||
| Male | 10.82 | 1.52 | 0.09 |
| (5.26) | (2.86) | (0.29) | |
| Female | 11.92 | 2.10 | 0.13 |
| (5.84) | (3.31) | (0.33) | |
| By age group: | |||
| 16–24 | 11.83 | 2.14 | 0.16 |
| (5.92) | (3.08) | (0.36) | |
| 25–34 | 11.98 | 2.14 | 0.14 |
| (5.94) | (3.26) | (0.34) | |
| 35–44 | 11.84 | 2.02 | 0.12 |
| (5.77) | (3.28) | (0.33) | |
| 45–54 | 12.06 | 2.10 | 0.12 |
| (5.92) | (3.41) | (0.33) | |
| 55–64 | 11.45 | 1.81 | 0.10 |
| (5.68) | (3.21) | (0.30) | |
| 65 and over | 10.21 | 1.27 | 0.08 |
| (4.65) | (2.55) | (0.27) | |
| By employment status: | |||
| Employed | 11.11 | 1.64 | 0.09 |
| (5.11) | (2.90) | (0.28) | |
| Unemployed | 14.40 | 3.47 | 0.26 |
| (7.08) | (3.95) | (0.44) | |
| Inactive | 11.59 | 1.97 | 0.13 |
| (6.06) | (3.29) | (0.34) | |
| By income quintile: | |||
| 1 (lowest) | 11.92 | 2.06 | 0.14 |
| (5.88) | (3.29) | (0.34) | |
| 2 | 11.35 | 1.84 | 0.11 |
| (5.55) | (3.13) | (0.31) | |
| 3 | 11.35 | 1.74 | 0.10 |
| (5.18) | (2.94) | (0.30) | |
| 4 | 11.03 | 1.59 | 0.08 |
| (5.12) | (2.91) | (0.28) | |
| 5 (highest) | 10.80 | 1.51 | 0.07 |
| (4.77) | (2.71) | (0.26) | |
- Note: Numbers in parentheses are standard deviations.
Estimating the impact of COVID-19 requires an estimate of counterfactual mental health in the absence of COVID-19. Identification of a full and robust individual-specific counterfactual will be a challenge even in the longer run when more extensive data become available. Nevertheless, we should still attempt to create the best pre-crisis measure possible, since if one were to investigate the effects of the pandemic by looking at individual-level changes before and during (or after) the crisis then this would implicitly attribute all observed changes to the crisis, which would be differentially problematic for different groups.
The latest data on each respondent's mental health are from wave 9, which was carried out between January 2017 and May 2019, with 96 per cent of interviews taking place in 2017 and 2018. There are a number of reasons we would expect individuals’ mental health at the onset of COVID-19 to differ from their wave 9 values. First, well-being is U-shaped over the life cycle, with mental health problems peaking in middle age and with particularly steep changes in mental health for young adults and those approaching and moving into retirement. This is shown in Figure 1, which pools data across all waves of the UKHLS.
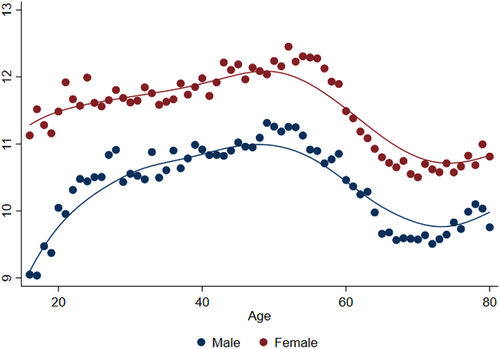
Age profile in GHQ scores, waves 1–9 (January 2009 to May 2019)
Note: Excludes individuals over the age of 80.
Source: UKHLS waves 1–9.
Second, there are pre-existing trends in mental health that vary by age and gender. Figure 2 shows that between wave 6 (January 2014 to May 2016) and wave 9 (January 2017 to May 2019), mental health problems as measured by the overall GHQ score and by the number of problems increased across most age groups, especially among the young. Meanwhile, the share of individuals with any severe problems declined over recent years, with older individuals seeing a steeper decline.
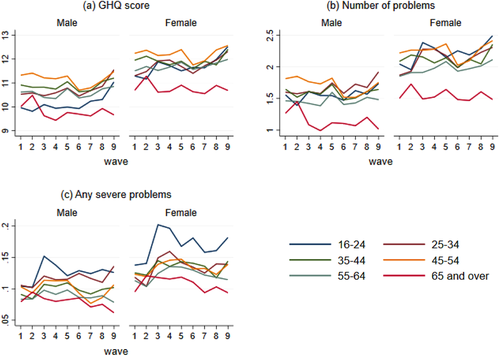
Trends in mental health by age and gender, waves 1–9 (January 2009 to May 2019)
Note: The waves ran as follows: wave 1, January 2009 to March 2011; wave 2, January 2010 to March 2012; wave 3, January 2011 to July 2013; wave 4, January 2012 to June 2013; wave 5, January 2013 to June 2015; wave 6, January 2014 to May 2016; wave 7, January 2015 to May 2017; wave 8, January 2016 to May 2018; and wave 9, January 2017 to May 2019.
Source: UKHLS waves 1–9.
Third, there are seasonal trends in mental health. GHQ scores fall (mental health improves) in the spring and summer months, as shown in Figure 3, which means that a sample interviewed entirely in April will not be comparable to a sample interviewed across a previous year.
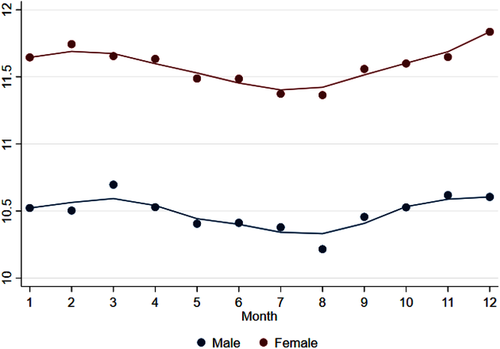
Seasonal trends in GHQ scores, waves 1–9 (January 2009 to May 2019)
Source: UKHLS waves 1–9.
Finally, individuals may have had idiosyncratic changes in circumstances over the two to three years that elapsed between their wave 9 interview and the month immediately preceding the COVID-19 pandemic that may have affected their pre-crisis well-being levels. Some of these changes will be captured in the COVID-19 module, which asks a limited number of questions referring to the respondent's situation in February 2020 – for example, on employment status – and so it is possible to include controls for these in our analysis.
In the analysis that follows, we therefore define the ‘effect’ of the pandemic as the difference between an individual's April 2020 mental health and a prediction of their likely level of mental health in April 2020 in the absence of the pandemic. We compare this with a measure of the effect that is just the simple difference between the respondent's April 2020 and wave 9 values. We use three sets of prediction models, each estimated using waves 6–9 (covering the period 2014–19) and including individual fixed effects. The models are estimated separately for six subsamples defined by gender and the individual's broad age group in wave 9 (16–34, 35–64 or 65 and over) to allow time trends to vary by gender and age group, as we saw in Figure 2. The models are nested and defined as follows: Model A simply controls for quadratic age and month effects, Model B adds an additional linear year effect and Model C includes additional controls for work status in February 2020 (i.e. just before the pandemic), living in a couple, the number of children in the household in three age groups (0–4, 5–15 and 16–18) and the region of residence. Each model is then used to predict the respondent's mental health in April 2020 and this will be an individual-specific prediction due to the inclusion of the individual fixed effect.19
The estimates for the most sophisticated prediction model (Model C) for the GHQ score are given in Table A1 in the online appendix; additional results are available from the authors on request. Figures A1–A3 in the appendix show wave 9 values alongside the three predicted counterfactual values from the models described above. We see that predicted counterfactual GHQ scores and the number of problems are higher than their wave 9 values across most gender and age groups, and particularly for younger individuals. This means that a naive comparison of April 2020 with wave 9 GHQ scores would overstate the impact of the pandemic, particularly for young people, for whom the pre-pandemic trend has been steepest. On the other hand, a naive comparison would understate the impact on severe mental health problems for gender and age groups that have been on a downward trend.
III. Results
1. Changes in overall GHQ
Figure 4 shows the distribution of mental health for the April 2020 sample across our three measures by gender and age group. Group-level averages are given for wave 9, our counterfactual prediction (‘April 2020 predicted’) and in April 2020 (‘COVID’). Age groups are defined by individuals’ ages in April 2020, so that the group averages track the same groups of individuals throughout.20 The predictions are based on a model that includes the full set of covariates, as shown in Appendix Table A1, although Figures A1–A3 show that group-level averages are very similar across the three prediction models. Age group averages are shown by grey dots for men and black dots for women. Average GHQ scores across all individuals are marked by the squares.
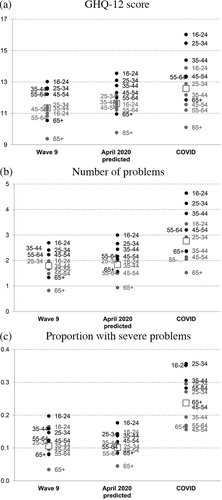
Mental health by gender and age group
Note: Wave 9 refers to January 2017–May 2019. Predicted values are based on prediction using a full set of controls (Model C), with time effects set to April 2020. Values for male age groups are indicated in grey. Values for female age groups are indicated in black. Squares are unconditional averages.
Source: UKHLS waves 6–9 and April COVID-19 survey.
Mental health levels have deteriorated during the COVID-19 pandemic, relative to both wave 9 levels and our counterfactual prediction. Average GHQ scores across all individuals in April 2020 were 1.23 points (10.8 per cent) higher than in wave 9 and 0.94 points (8.1 per cent) higher than our counterfactual prediction. To interpret the magnitude of these changes, it is useful to refer back to Table 1, which provides details of the distribution and subgroup means of mental health scores before the pandemic. As discussed previously, one point on the GHQ (Likert) scale is roughly equivalent to the average difference between men and women at wave 9, and to the average difference between those in the top quintile of the household income distribution and those in the bottom quintile. The previous four waves of data combined, collected over the period 2014–19 during which there was concern about the rising prevalence of mental health problems, showed a rise of GHQ average scores of just over half a point (0.54).
The deterioration in mental health was more marked for our indicators of the number of problems or the fraction of people with any severe problems. Individuals reported an average of one more problem, which is roughly twice the average difference between men and women at wave 9, and twice the difference between the top and bottom income quintiles. The share reporting any severe problems more than doubled, from 10.6 per cent in wave 9 and 10.2 per cent in our counterfactual prediction to 23.7 per cent in April 2020.
COVID-19 appears to have widened inequalities in mental health across gender and age groups and exacerbated pre-existing inequalities. Across all three measures, groups that had poor mental health before the pandemic hit generally suffered the largest deterioration in mental health, in both absolute and percentage terms. Young women saw the largest deterioration in mental health as a result of COVID-19: average GHQ scores among women aged 16–24 rose by 2.5 points or 18.2 per cent relative to the counterfactual prediction, and the share reporting a severe problem doubled from 17.7 per cent to 35.2 per cent. On the other hand, men aged 65 and over saw relatively little change in their GHQ scores and the number of problems reported, though the share reporting any severe problems increased sharply in percentage terms.
We now turn to examining how the effects of COVID-19 on mental health vary across individuals with different characteristics and different levels of exposure to the pandemic in terms of economic and health impacts. Tables 2 and 3 show regression results of the change in mental health measures (GHQ score, number of problems and the share with any severe problems), assessed relative to wave 9 and our counterfactual prediction, respectively. Recall that a one-point increase in GHQ scores is roughly equivalent to moving from the top to bottom quintile of the household income distribution at wave 9; an increase of one mental health problem is roughly double the difference between the richest and poorest groups.
| (1) GHQ score | (2) Number of problems | (3) Any severe problems | ||||||
|---|---|---|---|---|---|---|---|---|
| (a) Age & gender | (b) All covariates | |||||||
| Coeff. | p-val. | Coeff. | p-val. | Coeff. | p-val. | Coeff. | p-val. | |
| Female | 0.80 | <0.01 | 0.78 | <0.01 | 0.53 | <0.01 | 0.05 | <0.01 |
| 16–24 | 2.16 | <0.01 | 2.13 | <0.01 | 0.98 | <0.01 | 0.05 | 0.15 |
| 25–34 | 1.47 | <0.01 | 1.26 | <0.01 | 0.56 | <0.01 | 0.09 | <0.01 |
| 35–44 | 0.63 | 0.01 | 0.35 | 0.19 | 0.15 | 0.35 | 0.03 | 0.15 |
| 55–64 | 0.02 | 0.94 | 0.28 | 0.22 | 0.25 | 0.06 | 0.04 | 0.03 |
| 65 and over | 0.30 | 0.09 | 0.75 | 0.01 | 0.59 | <0.01 | 0.06 | 0.01 |
| High risk | –0.14 | 0.43 | –0.12 | 0.24 | 0.03 | 0.06 | ||
| Very high risk | –1.13 | 0.01 | –0.66 | <0.01 | –0.04 | 0.20 | ||
| NHS shielding | –0.05 | 0.89 | –0.04 | 0.86 | 0.04 | 0.13 | ||
| Had COVID-19 symptoms | 0.36 | 0.12 | 0.30 | 0.03 | 0.02 | 0.26 | ||
| Has COVID-19 symptoms | 2.02 | 0.03 | 0.96 | 0.05 | 0.11 | 0.05 | ||
| Self-employed in Feb | 0.03 | 0.92 | –0.07 | 0.63 | 0.02 | 0.40 | ||
| Not working in Feb | 0.06 | 0.81 | –0.09 | 0.53 | 0.03 | 0.15 | ||
| Hours fell Feb–Apr but not furloughed or laid off | 0.25 | 0.28 | 0.16 | 0.22 | 0.03 | 0.11 | ||
| Furloughed Feb–Apr | –0.20 | 0.48 | –0.05 | 0.78 | 0.03 | 0.17 | ||
| Laid off Feb–Apr | 1.79 | 0.03 | 1.05 | 0.02 | 0.01 | 0.83 | ||
| Pay fell Feb–Apr | –0.03 | 0.89 | –0.04 | 0.78 | –0.00 | 0.88 | ||
| HH earnings fell Feb–Apr | 0.22 | 0.29 | 0.22 | 0.07 | 0.02 | 0.17 | ||
| Shut-down sector in wave 9 | 0.73 | 0.01 | 0.46 | <0.01 | 0.04 | 0.06 | ||
| Key worker | –0.20 | 0.32 | –0.13 | 0.26 | 0.00 | 0.90 | ||
| Caring responsibilities | 0.18 | 0.21 | 0.16 | 0.05 | 0.01 | 0.22 | ||
| Youngest child 0–4 | 0.98 | <0.01 | 0.47 | <0.01 | 0.01 | 0.71 | ||
| Youngest child 5–15 | 0.40 | 0.11 | 0.27 | 0.06 | 0.01 | 0.52 | ||
| Youngest child 16–18 | –0.35 | 0.30 | –0.22 | 0.26 | –0.01 | 0.67 | ||
| Constant | 0.32 | 0.05 | –0.24 | 0.61 | 0.01 | 0.98 | 0.03 | 0.43 |
| Observations | 11,980 | 11,980 | 11,980 | 11,980 | ||||
| R2 | 0.015 | 0.030 | 0.030 | 0.017 | ||||
| Adjusted R2 | 0.014 | 0.026 | 0.026 | 0.013 | ||||
- Note: All columns include a quadratic in age and month and year effects. Columns 1b, 2 and 3 also include controls for highest qualification, ethnicity, region, whether in a couple and whether living with others (coefficients not reported). p-values below 0.05 are in bold.
| (1) GHQ score | (2) Number of problems | (3) Any severe problems | ||||||
|---|---|---|---|---|---|---|---|---|
| (a) Age & gender | (b) All covariates | |||||||
| Coeff. | p-val. | Coeff. | p-val. | Coeff. | p-val. | Coeff. | p-val. | |
| Female | 0.98 | <0.01 | 1.01 | <0.01 | 0.51 | <0.01 | 0.06 | <0.01 |
| 16–24 | 1.70 | <0.01 | 1.80 | <0.01 | 0.80 | <0.01 | 0.07 | 0.06 |
| 25–34 | 0.99 | <0.01 | 0.82 | <0.01 | 0.35 | 0.04 | 0.10 | <0.01 |
| 35–44 | 0.43 | 0.05 | 0.17 | 0.46 | 0.03 | 0.81 | 0.04 | 0.04 |
| 55–64 | 0.05 | 0.76 | 0.28 | 0.17 | 0.21 | 0.08 | 0.05 | <0.01 |
| 65 and over | 0.01 | 0.96 | 0.55 | 0.03 | 0.37 | <0.01 | 0.05 | <0.01 |
| High risk | –0.05 | 0.78 | –0.09 | 0.31 | 0.02 | 0.06 | ||
| Very high risk | –0.34 | 0.30 | –0.26 | 0.18 | 0.01 | 0.82 | ||
| NHS shielding | 0.01 | 0.98 | –0.07 | 0.69 | 0.05 | 0.02 | ||
| Had COVID-19 symptoms | 0.27 | 0.19 | 0.21 | 0.08 | 0.02 | 0.32 | ||
| Has COVID-19 symptoms | 2.04 | <0.01 | 0.99 | 0.02 | 0.08 | 0.10 | ||
| Self-employed in Feb | 0.15 | 0.53 | 0.03 | 0.80 | 0.01 | 0.59 | ||
| Not working in Feb | –0.32 | 0.17 | –0.28 | 0.03 | 0.01 | 0.64 | ||
| Hours fell Feb–Apr but not furloughed or laid off | 0.26 | 0.21 | 0.16 | 0.18 | 0.04 | 0.02 | ||
| Furloughed Feb–Apr | –0.21 | 0.42 | –0.04 | 0.79 | 0.02 | 0.42 | ||
| Laid off Feb–Apr | 1.89 | 0.01 | 1.16 | <0.01 | 0.01 | 0.90 | ||
| Pay fell Feb–Apr | –0.10 | 0.68 | –0.07 | 0.61 | –0.01 | 0.59 | ||
| HH earnings fell Feb–Apr | 0.28 | 0.15 | 0.24 | 0.03 | 0.03 | 0.04 | ||
| Shut-down sector in wave 9 | 0.57 | 0.03 | 0.36 | 0.01 | 0.04 | 0.03 | ||
| Key worker | –0.36 | 0.04 | –0.20 | 0.05 | –0.02 | 0.13 | ||
| Caring responsibilities | 0.12 | 0.36 | 0.11 | 0.13 | 0.02 | 0.12 | ||
| Youngest child 0–4 | 0.95 | <0.01 | 0.49 | <0.01 | 0.00 | 0.87 | ||
| Youngest child 5–15 | 0.36 | 0.12 | 0.27 | 0.04 | 0.02 | 0.36 | ||
| Youngest child 16–18 | –0.43 | 0.13 | –0.20 | 0.22 | –0.02 | 0.46 | ||
| Constant | 0.12 | 0.40 | 0.13 | 0.76 | 0.48 | 0.04 | 0.06 | 0.05 |
| Observations | 11,980 | 11,980 | 11,980 | 11,980 | ||||
| R2 | 0.016 | 0.033 | 0.033 | 0.022 | ||||
| Adjusted R2 | 0.016 | 0.029 | 0.029 | 0.018 | ||||
- Note: All columns include a quadratic in age and month and year effects. Columns 1b, 2 and 3 also include controls for highest qualification, ethnicity, region, whether in a couple and whether living with others (coefficients not reported). p-values below 0.05 are in bold.
In both tables, the first pair of columns (a) shows the change in GHQ scores regressed on gender and age group alone (relative to men aged 45–54). As with the earlier figures, we see that the increase in GHQ scores is larger for women and young people. The coefficient on women is larger and the coefficients on younger age groups smaller using the counterfactual prediction than using wave 9, which reflects differential trends prior to COVID-19. Using the counterfactual prediction – our preferred specification (Table 3) – the coefficient on women is 0.98. The increase in GHQ scores is 1.7 points higher among 16- to 24-year-olds than among those aged 45–54, and 0.99 points higher among 25- to 34-year-olds.
The second pair of columns in each table (b) adds controls for other demographic variables (educational qualifications, ethnicity, region) and individual-level exposure to COVID-19 in terms of household composition and caring responsibilities, whether individuals are medically vulnerable to COVID-1921 or have suffered symptoms of COVID-19, and the extent to which they have been economically affected by the pandemic. We see that the size of the coefficients on gender and younger age groups is relatively unaffected by the inclusion of these controls, which indicates that they matter in their own right and are not simply proxying for other dimensions of exposure. However, the size of the coefficients on older age groups increases when controls are added, and we start to see more of a U-shaped profile in age, with larger mental health impacts on younger and older individuals than on those in middle age.
The positive coefficients on older cohorts disappear when our covariates capturing the economic impacts and the presence of children are dropped (the results of this additional regression are not presented here). So, whilst being older is associated with a larger deterioration in mental health all else equal, the smaller effects on older ages that are apparent in column 1a are a consequence of the fact that older people are more insulated from the economic and childcare shocks of the pandemic.
Women and younger people also experienced a larger increase in mental health problems controlling for other factors. Using our preferred specification (the counterfactual prediction model presented in Table 3), women saw an increase of half a mental health problem more than men, all else equal, and the share of women with any severe problems increased by 6 percentage points more than for men. Recalling Table 1, this doubles the wave 9 gender gap in the number of problems, and more than doubles the percentage point difference in the shares of men and women with severe problems.
Medical vulnerabilities do not significantly affect the impact of COVID-19 on mental health using our preferred specification. But using a naive comparison with wave 9, being at ‘very high risk’ of COVID-19 complications (based on pre-existing conditions) appears to reduce the impact of the virus on mental health. This is because this group consists of older people, who have had better mental health trends in recent years – which again illustrates the need to account for differential pre-trends in assessing the impact of COVID-19. Having symptoms of the virus at the time of the survey – predictably – has a very large and significant effect on all three measures. Its coefficient in the overall GHQ score is 2.04 under our preferred specification, and the increase in the share with severe problems is 8 percentage points. Having had COVID-19 symptoms is also associated with more deterioration in mental health, but to a much smaller degree, and this is only statistically significant at the 10 per cent level when looking at the number of mental health problems (not the other two measures).
Falls in household earnings since February 2020 are associated with a larger deterioration in mental health as a result of COVID-19 that is statistically significant in our preferred specification in terms of both the number of problems and the prevalence of severe problems. Being laid off since February 2020 has a large impact on overall mental health problems (a 1.89 higher GHQ score and 1.16 more problems in our preferred specification), but does not appear to affect the measure of severe mental health problems. Conditional on changes in earnings, being furloughed appears to reduce the negative impact on mental health. Working in a sector that has been shut down during the lockdown – based on the classification in Joyce and Xu (2020) and wave 9 values since information on industries is not available in the April 2020 survey – appears to have a negative effect over and above the direct effect on hours and earnings, perhaps reflecting increased precarity in these roles and uncertainty about future prospects. All else equal, the deterioration in mental health was smaller among key workers, and the effect is statistically significant using our preferred specification.
Those with very young children (aged 0–4) saw a significantly larger increase in overall mental health problems (but not severe problems), by around one GHQ point and half a mental health problem under our preferred specification. Those with school-aged children aged 5–15 also saw a larger increase in mental health problems that is statistically significant in some measures and specifications – the coefficient is between a third and a half of that on very young children.
Coefficients are not shown in the tables due to a lack of statistical significance, but there is no evidence of differential effects by educational qualifications or by whether individuals are single or live alone. There are also no significant differences by ethnicity, with the exception of black individuals, who saw a smaller deterioration in mental health all else equal. There is no evidence of differential effects across regions of the UK, despite differences in the spread of the virus in April.
We also ran our preferred specification separately for men and women,22 mainly to assess whether any of the crisis exposure variables have impacted on mental health differentially across genders. The unconditional age profile is steeper for men, which reflects the fact that the impact of COVID-19 on mental health is concentrated in younger men (with only a small effect on older men), whereas women of all ages were negatively affected. Having symptoms of COVID-19 at the time of the survey appeared to have a much larger effect on the mental health of women: the coefficient on GHQ score is nearly four times larger. The negative effects of being laid off and working in a shut-down sector (in wave 9) are mainly driven by women: the effects are not statistically significant for men. The effect of having very young children (aged 0–4) is higher for women – the coefficients on GHQ score and the number of problems are around double those for men (for whom they are not statistically significant) – which may reflect the uneven distribution of childcare responsibilities under lockdown.23
2. Changes in individual GHQ components
Given that the GHQ-12 mental health scores are calculated from responses in 12 separate dimensions as described in Appendix B, it is possible to consider each of these dimensions separately in order to build an understanding of which types of dimensions are underlying the striking deterioration in mental health scores identified above. Such analysis can only be indicative, since the single questions in each dimension do not capture the dimension with enough precision or granularity to build a definitive picture of what is happening within that dimension. For example, the question on depression in the GHQ-12 questionnaire – ‘Have you recently been feeling unhappy or depressed?’ – is not sufficiently detailed to study the effects on depression in its own right. In addition, negative and positive language issues in the wording of individual questions mean that the GHQ-12 scale should be primarily thought of as a unidimensional measure of general mental health rather than a set of subscales representing distinct constructs.24
Nevertheless, to conclude our empirical analysis, we provide some preliminary descriptive findings along these lines to get some broad idea of the underlying changes in dimensions and to suggest future directions for analysis when more granular data on the various dimensions do become available. Reflecting the more limited goals of this exercise, rather than rerun the detailed multivariate analysis previously carried out for our overall mental health outcomes, we simply chart the main underlying trends.
Figure 5 shows trends in each individual component of the GHQ-12 scale over the course of the Understanding Society study from wave 1 (January 2009 to March 2011) up until the COVID module in April 2020, with trends plotted separately for young adults versus those aged 25 and over. The graphs are labelled to reflect the question content (see Appendix B), but responses are coded on a scale of 1 to 4 so that in each case higher values reflect poorer mental health.
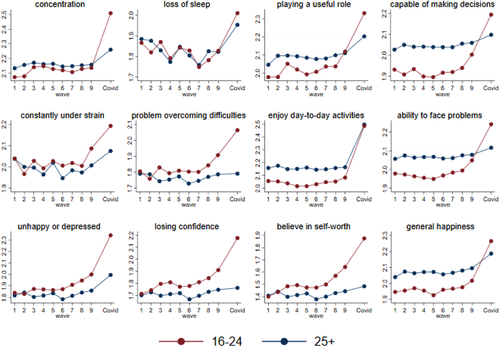
GHQ-12 component scores, by age group, waves 1–9 (January 2009 to May 2019) and April 2020
Note: All items are scored negatively, so higher numbers indicate worse outcomes in each domain. The waves ran as follows: wave 1, January 2009 to March 2011; wave 2, January 2010 to March 2012; wave 3, January 2011 to July 2013; wave 4, January 2012 to June 2013; wave 5, January 2013 to June 2015; wave 6, January 2014 to May 2016; wave 7, January 2015 to May 2017; wave 8, January 2016 to May 2018; and wave 9, January 2017 to May 2019.
Source: UKHLS waves 1–9 and April COVID-19 survey.
There was a marked deterioration in measures relating to happiness – enjoying day-to-day activities, general happiness, and feeling unhappy or depressed – that is seen across both age groups, though to somewhat different extents. But in many dimensions where young adults saw large declines in mental health – such as feeling capable of making decisions, having problems overcoming difficulties, and the ability to face problems – we do not see any particular deviation from the pre-COVID trend for older adults.
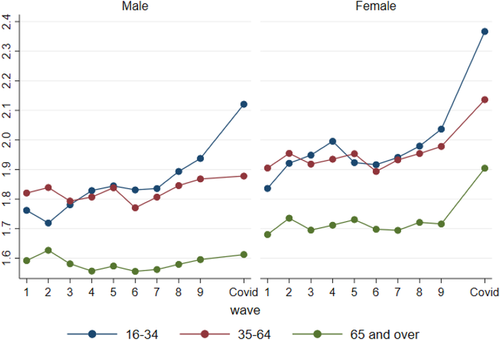
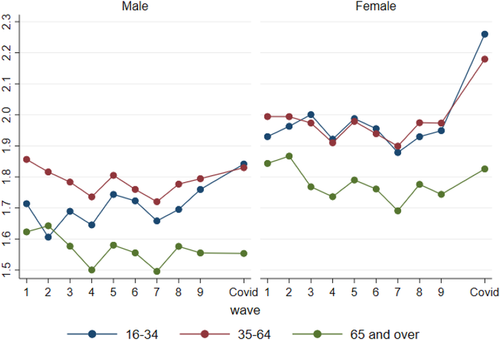
For dimensions of particular interest, we can also break down trends by the six age–gender groups that we have been working with previously in our analysis. We consider four key dimensions: enjoyment of day-to-day activities, depression, sleep and the perception of playing a useful role. Figure 6 indicates that changes in enjoyment of day-to-day activities were strikingly similar for all age–gender groups, perhaps unsurprisingly since the lockdown and social distancing have affected all our lives and the way that we live them. There is more variability, however, in the evolution of specific dimensions that might be thought more fundamentally important for current or future health, such as depression, sleep and even perhaps sense of purpose, which is where we see many of the changes that underlie the age and sex differences in the overall GHQ score. Increases in feelings of unhappiness or depression have been greater for the young (Figure 7), and reductions in sleep due to worry have been apparent for women but not for men, although somewhat similar across age groups within each gender, with the exception of a small rise in difficulty sleeping for younger males, as shown in Figure 8. The gender difference in loss of sleep through worry is likely to be particularly important when coupled with recent evidence that has emerged on time-use differences between women and men.25 Similarly, when it comes to looking at whether people feel they are playing a useful role, it is also the youngest group (both male and female) and the older groups of women where we see the largest deterioration relative to pre-COVID trends (Figure 9).

(Lack of) enjoyment of day-to-day activities, by gender and age group, waves 1–9 (January 2009 to May 2019) and April 2020
Note: Higher values reflect poorer mental health. The waves ran as follows: wave 1, January 2009 to March 2011; wave 2, January 2010 to March 2012; wave 3, January 2011 to July 2013; wave 4, January 2012 to June 2013; wave 5, January 2013 to June 2015; wave 6, January 2014 to May 2016; wave 7, January 2015 to May 2017; wave 8, January 2016 to May 2018; and wave 9, January 2017 to May 2019.
Source: UKHLS waves 1–9 and April COVID-19 survey.
Unhappy or depressed, by gender and age group, waves 1–9 (January 2009 to May 2019) and April 2020
Note and source: See Figure 6.
Loss of sleep, by gender and age group, waves 1–9 (January 2009 to May 2019) and April 2020
Note and source: See Figure 6.
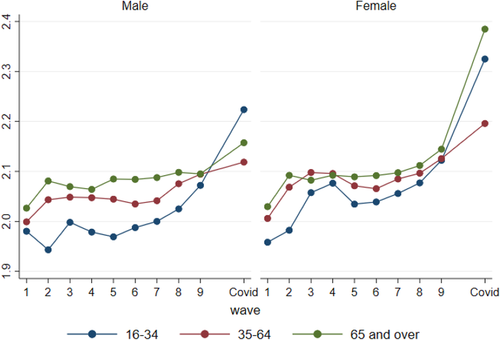
(Not) playing a useful role, by gender and age group, waves 1–9 (January 2009 to May 2019) and April 2020
Note and source: See Figure 6.
IV. Conclusions
The mental health effects of the COVID-19 pandemic have been large, as initially speculated and as previous cross-sectional real-time analysis has shown. Our contribution in this paper has been to set these changes in the context of the distribution of individuals’ previous longitudinal trajectories of mental health, to form a prediction of what mental health would have been in April 2020 in the absence of the pandemic, and to use this framework to quantify the size of the effects of the crisis on mental health as measured by the GHQ-12. We show that the effects are large and that they differ both in size and in nature according to which population subgroups are being looked at, with young people and women experiencing the largest declines in mental health.
Differing patterns and magnitudes are also seen when we look at the number of reported problems or the severity of mental health problems as opposed to just average scores, and our analysis reveals that the deterioration in average scores is driven by more problems, and more ‘severe’ problems, as opposed to just a general mild worsening of pre-existing problems for everyone. Indeed, the increase in the prevalence of reporting at least one severe problem, and the increase in between-group inequality in this prevalence, is striking. More generally, as well as worsening mental health on average, the COVID-19 pandemic in the UK can clearly be seen to have increased mental health inequalities.
Our data relate to April 2020 when the UK was in the depths of the full lockdown and COVID-19 deaths were still rising rapidly. Future waves of data on the same respondents, to be collected monthly over the next year, will provide an invaluable resource for documenting month-to-month variation and tracking the permanence or otherwise of these mental health effects in the context of the longer-run mental health trajectories that have been observed for these same individuals over the previous 10 years. Thus, researchers will be able to look at the permanence or otherwise of the mental health effects, and at the extent and speed at which different groups are able to bounce back as the distancing restrictions unwind and as government policies aiming to protect groups from the harmful effects of the crisis are withdrawn.
Whilst the pre-existing longitudinal data and the large representative sample from the Understanding Society study are undoubted advantages of the analysis we have been able to carry out here compared with previous work on COVID-19 and mental health, our analysis has nevertheless been limited by only being able to use the somewhat crude GHQ-12 measure of mental health, due to the general-purpose nature of the Understanding Society survey questionnaire. But our results on the magnitude of GHQ changes and on the differences in trends in some of the components driving those changes do suggest that it will be imperative that researchers assess the complex and multifaceted mental health consequences of the pandemic in more detail as more and better data become available. Specifically, soon-to-be-available COVID-specific data modules from UK studies such as the Centre for Longitudinal Studies (CLS) cohort studies and the English Longitudinal Study of Ageing (ELSA), and European studies such as the Survey of Health, Ageing and Retirement in Europe (SHARE), will provide more granular and detailed measures of specific dimensions of mental health both in terms of respondents’ outcomes and in terms of their past trajectories. These data will facilitate more detailed analysis of outcomes such as depression, anxiety and sleep, and the specific mechanisms that might underlie changes. As this paper has shown, it is important to understand these effects within the contexts of the individuals’ longer-run trajectories, and so research using these and other pre-existing nationally representative longitudinal studies, as well as further research using the Understanding Society COVID modules, should be considered a priority for the next few months as researchers and policymakers alike seek to understand the distribution and permanence of the mental health effects of the crisis in more detail.
References
- 1 See Kivimäki et al. (2017).
- 2 Holmes et al., 2020.
- 3 For example, Layard et al. (2020).
- 4 Office for National Statistics, 2020.
- 5 Fancourt et al., 2020.
- 6 Yamamura and Tsutsui (2020) for Japan.
- 7 Brülhart and Lalive (2020) for Switzerland and Armbruster and Klotzbücher (2020) for Germany.
- 8 Tubadji, Boy and Webber, 2020.
- 9 Yamamura and Tsutsui, 2020.
- 10 Armbruster and Klotzbücher, 2020.
- 11 Tubadji, Boy and Webber, 2020.
- 12 University of Essex, 2020a and 2020b.
- 13 Understanding Society has been collecting information annually on a sample of almost 100,000 individuals since 2010 (see Institute for Social and Economic Research (2019) for details) and introduced a monthly internet component in May 2020 for a subset of almost 20,000 respondents to cover the duration of the pandemic (see Institute for Social and Economic Research (2020)). The COVID-19 data used here are those for the first COVID wave, collected in April 2020.
- 14 The most recent pre-COVID observation currently publicly available on Understanding Society respondents relates to sometime between May 2017 and May 2019, depending on when the respondent was interviewed, with only very few cases being collected after January 2019.
- 15 See Cox, Blaxter and Buckle (1987).
- 16 In addition, with the exception of wave 1 of Understanding Society when it was collected as part of the face-to-face interview, it has always been collected as part of a self-administered module, so we might expect minimal mode effects in measurement as a result of the COVID-19 questionnaire being administered online.
- 17 The raw gender effects in terms of changes between wave 9 and the COVID module are also documented in Etheridge and Spantig (2020), who argue social factors (friends and loneliness) and, to some extent, changes in family and caring responsibilities can account for these differences.
- 18 In all our analysis, we use the COVID-19 module cross-sectional weights to adjust for unequal selection probabilities and differential non-response, since even though our predictions are formed from longitudinal data, our key analysis is of the COVID module cross-sectional data. These weights model response probabilities conditional on past response to wave 9 and assign zero weight to individuals who had not responded to wave 9; hence we are implicitly providing estimates that are representative of the UK household population in 2017–19.
- 19 To test the validity of the models, we used data from waves 6–8 to predict mental health in wave 9. Predicted average Likert scores were within 3 per cent of actual average Likert scores for each of the 12 age–gender groups considered below with the exception of young males aged 16–24, for whom results differed by 5 per cent.
- 20 The small differences in average wave 9 values between Figure 4 and Figure 2 above partly reflect compositional differences between the COVID sample and the wave 9 sample as a whole and partly reflect differences in the definition of age groups between the two figures. Figure 4 presents groups defined by age at the COVID module, on a constant cohort basis, whereas Figure 2 uses current age at each wave. Hence, for example, the age group labelled ‘16–24’ in Figure 4 is actually 14–22 in wave 9, and those under age 16 would not have completed a questionnaire at wave 9.
- 21 Based on whether they have ever been diagnosed with a medical condition that places them at ‘high risk’ or ‘very high risk’ to the virus, and/or been asked by the NHS to shield. See COVID-19 derived variables documentation in Institute for Social and Economic Research (2020) for more details on medical conditions.
- 22 The results are not shown but are available from the authors on request.
- 23 Andrew et al., 2020.
- 24 Gnambs and Staufenbiel, 2018.
- 25 See Andrew et al. (2020).




