Histologically Remarkable Eosinophilic Esophagitis Responsive to Dupilumab in a Gastrostomy Tube–Dependent Pediatric Patient on Amino Acid Formula
Castro and Arostegui contributed equally to this work.
Informed consent was obtained from the mother and father of this child for reporting of this case.
The authors report no conflicts of interest.
Abstract
Eosinophilic esophagitis (EoE), an eosinophil predominant, TH2-mediated condition increasing in prevalence in pediatric and adult populations, is typically treated with dietary manipulations to avoid triggering antigens. However, identifying specific dietary causes remains a persistent challenge, and restrictive diets are burdensome. Total dietary modification using amino acid–based formula does not always produce symptomatic or histologic resolution, suggesting that exposure to ingested aeroallergens drives their disease. EoE patients demonstrate symptomatic exacerbation from July to September correlating with higher grass and ragweed pollen counts. We present a 7-year-old tracheostomy- and gastrostomy-dependent girl who was found on surveillance endoscopy to have profound eosinophilic infiltration throughout the esophagus with inflammatory changes including basal cell hyperplasia on histology. She responded partially to topical corticosteroid therapy with fluticasone and had complete resolution of esophageal eosinophilic infiltrate with subcutaneous dupilumab.
INTRODUCTION
Eosinophilic esophagitis (EoE) is an eosinophil predominant, TH2-mediated condition increasing in prevalence in pediatric and adult populations.1 EoE is typically antigen mediated, allowing dietary alterations to serve as a primary therapy. However, identifying specific dietary triggers remains a persistent challenge and a burden of care patients are often unable to meet.1, 2 A significant fraction of EoE patients do not respond to total dietary modification in the form of an amino acid–based formula, suggesting that exposure to ingested aeroallergens drives their disease.3-5 Additional work has identified seasonality to EoE symptoms, demonstrating symptomatic exacerbation from July to September correlating with higher grass and ragweed pollen counts.6 EoE symptoms typically revolve around dysphagia, so identification of EoE in patients who do not feed orally is a problem. We report an asymptomatic tracheostomy- and gastrostomy-dependent 7-year-old girl who was found to have profound eosinophilic infiltration in the proximal esophagus and eosinophilic infiltrates in the distal esophagus with histologic evidence of inflammatory changes including basal cell hyperplasia (Figs. 1 and 2).
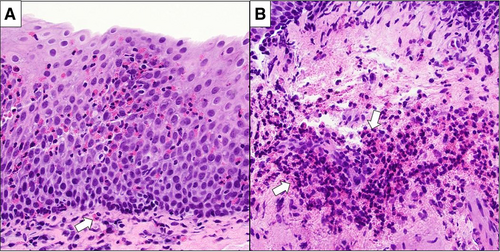
Initial esophageal histology.
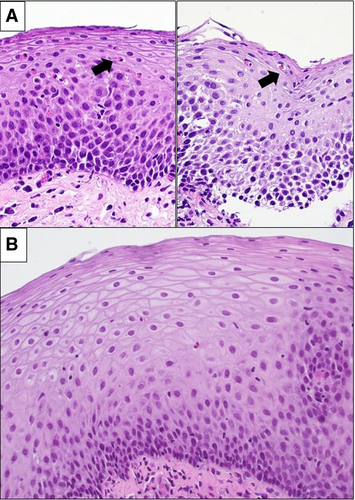
Esophageal histology after budesonide treatment and after dupilumab treatment.
CASE PRESENTATION
A neurodevelopmentally normal, tracheostomy- and gastrostomy-dependent 7-year-old female with a history significant for extreme prematurity (26 weeks gestation), C-section birth, chronic lung disease, and tracheal and subglottic stenosis, underwent endoscopic evaluation before potential airway reconstruction surgery. The child had no complaints of dysphagia, odynophagia, or abdominal discomfort. After birth, she had had a prolonged neonatal intensive care unit stay where she was primarily fed using fortified breastmilk and premature infant nonhydrolyzed protein formula. At 9 months of age, a gastrostomy tube was placed, and she was switched to an amino acid–based formula. She has remained almost entirely gastrostomy dependent, although she had rare low volume tastes of food by mouth (fruit smoothies with yogurt). She has no history of proton pump inhibitors, personal or family history of atopy, or multiple courses of antibiotics. In March 2021 (beginning of the high pollen/grass season), esophagogastroduodenoscopy (EGD) demonstrated mild nodularity in the distal esophagus and pre-pyloric region, and an endoscopic reference score of 0.7
Histopathologic findings were significant for increased intraepithelial eosinophils in biopsy samples from 3 levels in the esophagus. Severe disease was identified in the proximal esophagus, where >100 eosinophils per high power field (hpf) were present in the epithelium and submucosa along with marked basal cell hyperplasia and edema. All the features of the eosinophilic esophagitis histology scoring system (EoEHSS) were evaluated and graded with a pretreatment final score of 15 (basal zone hyperplasia = 2, dilated intracellular spaces = 3, eosinophilic abscess = 3, eosinophilic inflammation = 4, eosinophilic surface layering = 1, and lamina propria fibrosis = 2).8 Although gastroesophageal reflux disease (GERD) remained a possibility, the severe eosinophilia, basal cell hyperplasia, and elevated EoEHSS throughout the esophagus strongly suggested EoE rather than a microbial/GERD-mediated process,9, 10 and treatment was commenced accordingly.
All oral feeding was subsequently discontinued, and the patient was treated with swallowed fluticasone (110 µg/actuation), 2 puffs by mouth twice per day, and esomeprazole 20 mg daily. Allergy/immunology evaluation did not identify any dietary allergen sensitizations. Follow-up EGD after 5 months was visually unchanged from prior, although histology demonstrated substantial improvement at all sites as measured by the number of eosinophils, which were <15 in the mid- and proximal esophagus, and up to 50/hpf in the distal samples, and improvement of the EoEHSS from 15 to 8 post-treatment. To optimize the mucosal eosinophilic infiltration as far as possible before open airway reconstructive surgery, and as family did not want to increase or alter oral topical corticosteroids, she was initiated on subcutaneous dupilumab therapy. She received a loading dose of 600 mg, then 300 mg once a month as maintenance therapy. After 4 months on dupilumab therapy, follow-up EGD was endoscopically normal; biopsies demonstrated histological resolution of the eosinophilic infiltration with no intraepithelial eosinophils in distal esophagus, and focal rare intraepithelial eosinophils <2/HPF in mid- and proximal esophagus with a EoEHSS of 4.
DISCUSSION
The pathogenesis of EoE has not been fully elucidated, but current data demonstrate significant mediation by T helper cell-2 (Th2) via signaling in various cytokine pathways including interleukin (IL)-5, IL-4, and IL-13.11 These cytokines drive subsequent activation and recruitment of eosinophils to the esophageal mucosa via eotaxin-3.12, 13 Approximately 5% of EoE cases is believed to result from environmental or aeroallergen exposure.3-5 Our G-tube–dependent, amino acid formula fed patient's disease likely is driven primarily by aeroallergen/environmental exposure rather than her very limited food exposure.
Our experience with this patient raises an important question in understanding which patients with other risk factors (atopy/asthma) who are not fed by mouth may require investigation. Studies in adult patients undergoing endoscopy have demonstrated a range of incidental EoE finding of 0.4% or higher,14 suggesting a significant burden of atypical or asymptomatic disease. Given the normal appearance of the esophagus on visual examination, without biopsies this inflammatory process would have been missed, potentially complicating airway reconstruction. Tools such as EndoFLIP may help determine need for biopsies or establish health in real time. Further study is needed to identify the true prevalence of EoE in these populations to assess any possible need for screening endoscopy in asymptomatic patients with these conditions, especially if they are not oral feeders and will have a delayed symptomatic presentation.
This case also highlights an interesting challenge in management of EoE. Typical first-line therapy includes 6-food elimination diet, swallowed topical corticosteroids, and proton pump inhibitors.15 Novel biologic therapies such as dupilumab, a monoclonal antibody targeting IL4 receptor and inhibiting IL4 and 13 signaling, have also shown efficacy in treating EoE.14 The receptor IL-4Rα has 2 components: type I (IL-4Rα and γc) and type II (IL-4Rα and IL-13Rα1) IL-4R complexes. If the IL4Rα was to bind to the IL4 and IL13, it would lead to gene transcription of cytokines for eosinophil migration into affected tissues. Dupilumab continues to emerge as one of the most successful treatments to target the IL-4R axis.15 Given the shared pathophysiology among eosinophilic conditions, dupilumab is used to induce both histologic and symptomatic remission in EoE.16 In EoE, dupilumab has been shown to reduce dysphagia, eosinophilic infiltration, and increase esophageal distensibility.16
Notably, dupilumab has recently been Food and Drug Administration approved for pediatric patients older than 12 years and greater than 40 kg, based on results of the TREET trial that demonstrate improvement in esophageal eosinophilia (58.8% of patients achieving histologic remission) and in symptom scores, without significant safety signals.17
In our case, large volume topical corticosteroid therapy with budesonide presented a parental concern, and significant dietary modifications were not possible as the patient was already fed with an amino acid formula. Our partially successful therapy with swallowed fluticasone demonstrates the value of that approach, but also underpins its limitations, with the best impact on proximal esophageal disease as expected. Dupilumab, however, showed marked efficacy, with complete histologic resolution and mucosal healing documented by improved EoEHSS score, raising the need for further work on this monoclonal antibody as part of the EoE management in the pediatric population, including efforts to lower age the range of the Food and Drug Administration indication.
ACKNOWLEDGMENTS
T.W., D.A., and K.C. completed the endoscopic evaluation. K.C., D.A., J.P., and S.G. wrote the manuscript. M.P. completed EoEHSS scoring, histological review, and created figures. T.W., S.R., and S.S. edited the manuscript. D.A., K.C., S.G., and J.P. completed chart review and literature review.