Factors and Growth Trends Associated With the Need for Gastrostomy Tube in Neonates With Congenital Diaphragmatic Hernia
This project was supported by the National Institutes of Health Grant Number T32AI125222 (Schwab). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors report no conflicts of interest.
Authors Contributions: M.S.: project design, data collection/analysis/interpretation, manuscript writing and revisions, final approval of the version to be published, agreement to be accountable for all aspects of the work.
S.B.: project design, data collection and interpretation, manuscript revisions, agreement to be accountable for all aspects of the work.
M.K.K.: project design, data collection and interpretation, manuscript revisions, agreement to be accountable for all aspects of the work.
L.V.: project conception and design, data analysis and interpretation, manuscript revisions, agreement to be accountable for all aspects of the work.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal's Web site (www.jpgn.org).
An infographic is available for this article at: http://links.lww.com/MPG/C380.
ABSTRACT
Objectives:
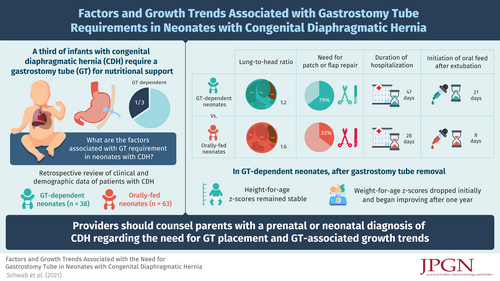
A third of infants with congenital diaphragmatic hernia (CDH) require a gastrostomy tube (GT) for nutritional support. We compared CDH infants who are GT-dependent to those able to meet their nutritional needs orally, to identify factors associated with requiring a GT and evaluate their long-term growth.
Methods:
Patients with CDH repaired at a single institution between 2012 and 2020 were included. Charts were retrospectively reviewed for demographic, surgical, and post-operative details. Mann-Whitney test and Fischer exact test were performed to compare GT-dependent neonates (n = 38, experimental) with orally fed neonates (n = 63, control). Significance was set at <0.05.
Results:
Thirty-eight percent received a GT (median 67 days, interquartile range [IQR] 50–88). GT-dependent neonates were significantly more likely to have a lower lung-to-head ratio (median 1.2, IQR 0.9–1.4, vs 1.6, IQR 1.3–2.0, IQR P < 0.0001), undergone patch or flap repair (79% vs 33%, P < 0.0001), and been hospitalized longer (median 47, IQR 24–75 vs 28 days, P < 0.0001). Fourteen of 38 had their GT removed (median 26 months, IQR 14–36). GT-dependent neonates initiated oral feeds (calculated as time since extubation) later (median 21, IQR 8–26, vs 8 days, IQR 4–13, P = 0.006). Height-for-age z scores remained stable after GT removal, while weight-for-age z scores dropped initially and began improving a year later.
Conclusions:
The need for a gastrostomy for nutritional support is associated with more severe CDH. Over a third of patients no longer needed a GT at a median of 26 months. Linear growth generally remains stable after removal. These results may help counsel parents regarding nutritional expectations.