Morphometric Changes in Children With Small Bowel Crohn Disease During Induction of Therapy
A Pilot Study
Supplemental digital content is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal's Web site (www.jpgn.org).
D.B.S. is currently at the Mayo Clinic, in Rochester, Minnesota.
J.R.D. is currently at Cincinnati Children's Hospital Medical Center.
This study was partly supported by grant number 2UL1TR000433 from the National Center for Advancing Translational Sciences. The content is solely the responsibility of the authors and does not necessarily represent the official views of NCATS or the National Institutes of Health.
Clinicaltrials.gov number: NCT01593462
The authors report no conflicts of interest.
An infographic is available for this article at:http://links.lww.com/MPG/C87.
ABSTRACT
Objective:
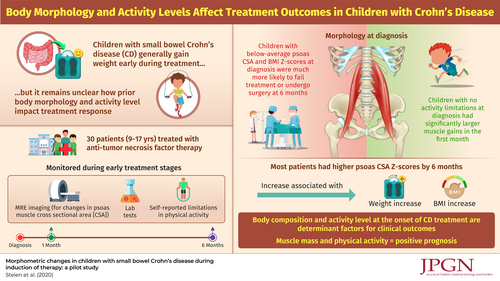
Children and adolescents with Crohn disease (CD) commonly gain weight during treatment induction, which is thought to be a marker of better health. Body composition is, however, rarely assessed at diagnosis, and changes during early treatment are not often quantified. Therefore, it is unknown if these gains are truly healthy. We sought to evaluate skeletal muscle changes during initial treatment for CD by using routine imaging.
Methods:
Single-center prospective study. Pediatric patients diagnosed with small bowel CD underwent serial magnetic resonance enterography (MRE) imaging, laboratory testing, and disease-activity assessment, at diagnosis, 1 and 6 months of treatment. MRE-based cross-sectional morphometry was used to measure psoas muscle cross sectional area (CSA). Psoas CSA z-scores were calculated using normative data.
Results:
We enrolled 30 children (ages 9--17 years). Twenty-eight of 30 (93%) received anti-tumor necrosis factor therapy and 4 required surgical resection. Children with below-average psoas CSA and body mass index (BMI) z-scores at diagnosis were much more likely to fail treatment or undergo surgery by 6 months compared with those with higher z-scores (55% vs 0%; P = 0.001). Children with no activity limitations at diagnosis had significantly larger muscle gains in the first month, compared with those whose activity was limited at diagnosis (P = 0.012). Most patients had higher psoas CSA z-scores by 6 months, and these increases were associated with weight and BMI z-score increases.
Conclusions:
Skeletal muscle growth contributes to weight gain during treatment induction in most patients with CD. Psoas muscle CSA on diagnostic imaging may have prognostic value in children with CD.