Mutant Calreticulin in the Myeloproliferative Neoplasms
The authors have indicated they have no potential conflicts of interest to disclose.
Abstract
Mutations in the gene for calreticulin (CALR) were identified in the myeloproliferative neoplasms (MPNs) essential thrombocythaemia (ET) and primary myelofibrosis (MF) in 2013; in combination with previously described mutations in JAK2 and MPL, driver mutations have now been described for the majority of MPN patients. In subsequent years, researchers have begun to unravel the mechanisms by which mutant CALR drives transformation and to understand their clinical implications. Mutant CALR activates the thrombopoietin receptor (MPL), causing constitutive activation of Janus kinase 2 (JAK2) signaling and cytokine independent growth in vitro. Mouse models show increased numbers of hematopoietic stem cells (HSCs) and overproduction of megakaryocytic lineage cells with associated thrombocytosis. In the clinic, detection of CALR mutations has been embedded in World Health Organization and other international diagnostic guidelines. Distinct clinical and laboratory associations of CALR mutations have been identified together with their prognostic significance, with CALR mutant patients showing increased overall survival. The discovery and subsequent study of CALR mutations have illuminated novel aspects of megakaryopoiesis and raised the possibility of new therapeutic approaches.
Introduction
In 2013, 2 seminal papers described mutations in the calreticulin gene (CALR) in a subset of essential thrombocythaemia (ET) or myelofibrosis (MF) patients1, 2; more than 36 different mutations were reported, all of them insertions or deletions (indels) causing a +1 frameshift within exon 9 that generated a novel C-terminal sequence. These mutations were mutually exclusive with Janus kinase 2 (JAK2) and thrombopoietin receptor (MPL) mutations, found in the majority of ET and MF patients. The two most frequent CALR mutations, a 52 base pair (bp) deletion (DEL) and a 5 bp insertion (INS), accounted for 85% of the mutations and were termed type I and II, respectively (Fig. 1A). Apart from the two most common mutations, a myriad of other mutations have been identified. These less common mutations can be classified as either type I-like or type II-like based on predicted helical secondary structure3 or the number of calcium-binding amino acids remaining in the novel C-terminus.4
While previously identified phenotypic driver mutations in MPNs affect genes directly involved in cytokine signaling or its regulation (eg, BCR-ABL1,5 CSF3R,6 JAK2,7-10 MPL 11, 12), CALR instead encodes an endoplasmic reticulum (ER) chaperone that serves multiple functions, including calcium homeostasis and glycoprotein quality control, and is distributed across different cellular compartments.13 CALR is encoded by a highly developmentally conserved gene, with 70% nucleotide homology between mouse and human, and has three domains: an N-terminal lectin domain (N), a proline-rich domain (P), and an acidic carboxyl terminus (C) that terminates in the amino acid sequence KDEL, an ER retrieval signal.14 The N domain of CALR is primarily responsible for its chaperone activity, while its C domain has been identified as the major binding site of calcium in the ER, binding Ca2+ ions with high capacity and low affinity.15 Because no truncating mutations were found in the original patient cohorts, a gain-of-function mechanism for CALR mutations was postulated.16
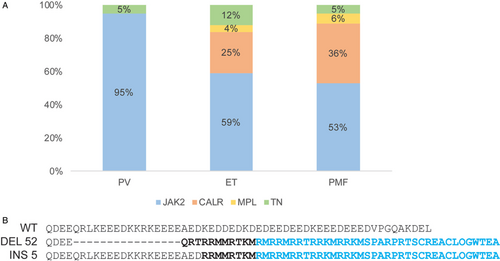
A. Native and type I and type II-mutant CALR primary sequence. The frameshift (frameshifted amino acid residues in bold) within the exon 9 generates a common novel CT in cyan, which is common to all frameshift mutations and substitutes most of the native C domain, involved in the storage of calcium. The ER retrieval signal (KDEL) is also lost. Adapted from Nangalia et al.2 B. Distribution of driver mutations in MPN. TN stands for triple negative, that is, neither JAK2, CALR, nor MPL mutated. Adapted from Klampfl et al.1
Over the past 6 years, extensive work has begun to unravel the mechanisms underlying mutant CALR-driven transformation in cellular systems and animal models. Clinical investigations have started to tease out differences between CALR-positive and negative MPNs as well as between type I and type II CALR mutations. Finally, advances in the understanding of the pathogenesis of CALR-driven MPNs are paving the way for a more tailored treatment regimen for CALR-mutated patients.
Consequences of CALR mutation
Functions of mutant CALR in vitro
CALR mutations are associated with ET and MF, as are JAK2 and MPL mutations, but are mutually exclusive with JAK2 and MPL, suggesting they drive transformation through the same pathway (some reports have found rare patients with co-occurring JAK2 V617F and CALR mutations, but they did not address the possibility of biclonality17-19). Consistent with this finding, initial experiments showed that all of these mutations operate through the constitutive activation of the JAK2 signaling cascade.1, 2 Much of the research to date on the oncogenic effects of CALR mutations has focused on MPL signaling in cytokine-dependent cellular systems. CALR mutations require the expression of MPL to render autonomous cell growth in Ba/F3 cells,20-22 UT-7/TPO cells20, 23 and γ2A cells expressing JAK2.24 Conversely, mutant CALR is unable to induce cytokine independence when co-expressed with erythropoietin receptor (EPOR)20, 24 and drives little24 or no20 autonomous cell growth upon co-expression with the granulocyte-colony stimulating factor receptor (CSF3R). The lack of activation of EPOR by mutant CALR likely explains why CALR mutations are not seen in polycythemia vera (PV) patients (Fig. 1B, Fig. 2).
In order for mutant CALR to drive transformation, the presence of the extracellular domain of MPL is required,24, 25 particularly its sites for N-linked glycosylation,24 where a lectin such as CALR would be predicted to bind. Indeed, the glycan-binding sites of CALR itself are crucial for activating MPL,24 while the polypeptide-binding regions and chaperone activity of CALR are dispensable.25 Mutant CALR also requires its novel positively charged C-terminal residues to activate MPL signaling: mutation of these residues to uncharged glycine residues abrogates its transforming ability.20 Of note, truncation of exon 9 eliminates the transforming abilities of mutant CALR, further underscoring the functional importance of the novel C-terminus.24 Analogously, removal of the 36 most distal residues from the new C-terminus prevents mutant CALR from transforming Ba/F3-MPL cells. This Δ36 mutant is still able to bind to MPL, suggesting that binding to and activation of the receptor may be two separate processes.25 In order to activate MPL, mutant CALR must oligomerize26; oligomerization of wild-type CALR has also been observed when CALR is N-arginylated,27 though the N-arginylation status of mutant CALR is unknown. Mutant CALR can only activate MPL and drive STAT5 activity at the cell surface: if the complex is retained in the ER via treatment with Brefeldin A, an inhibitor of ER-Golgi trafficking, no STAT5 transcriptional activity is observed. Additionally, mutant CALR can rescue the cell surface trafficking of a MPL mutant, MPL R102P, that is normally retained in the ER in some cases of hereditary thrombocytosis.28
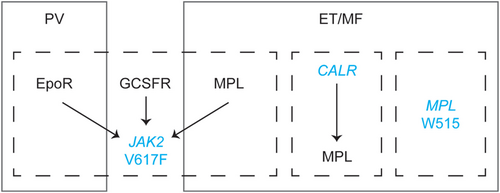
In this model, disease phenotypes reflect, at least in part, the cytokine receptor(s) that are activated by a given driver mutation. Mutant CALR and MPL activate MPL signaling, and so are associated with a megakaryocyte/platelet phenotype (ET or MF). By contrast, JAK2 V617F can activate signaling via EpoR or MPL, which are associated with PV and ET/MF, respectively. The phenotype of an individual patient with a JAK2 V617F mutation also depends on a variety of other factors that affect EpoR or MPL signaling, including genetic background and mutation dose. JAK2 V617F also interacts with GCSFR, probably explaining why JAK2-mutant ET patients show higher neutrophil counts than do CALR-mutant ET patients.
Most work on mutant CALR has focused on human CALR and MPL, but there is some evidence that analogous frameshift mutations in murine Calr can transform γ2A and Ba/F3 cells when co-expressed with either human MPL or CSF3R.20, 29 While the majority of studies on signaling pathways driven by mutant CALR have used well-established cell lines, one study generated induced pluripotent stem cell-derived hematopoietic progenitor cell lines from a healthy donor and a patient with a type II CALR mutation. Here, mutant CALR increased megakaryocyte numbers with premature commitment to megakaryopoiesis.30 Cell lines derived from patients bearing disease-associated mutations may thus represent promising lines of research in the future.
Though constitutive activation of the JAK2 signaling cascade is considered the primary mechanism driving the effects of CALR mutations, other potential mechanisms have been investigated. CALR and JAK2 mutations overlap to some extent in their ability to activate JAK-STAT signalling31; however, additional mechanisms may contribute to mutant CALR-driven oncogenesis.32 CALR mutations lead to the replacement of a series of Ca2+-binding, negatively charged amino acids with a stretch of positively charged residues. This would perturb the ability of CALR to properly retain Ca2+ ions within the ER lumen, affecting Ca2+ signaling pathways. Consistent with this idea, megakaryocytes derived from type I CALR-mutated patients showed an enhanced release of Ca2+ from ER stores compared to those derived from either healthy donors or type II mutated patients.4 This enhanced Ca2+ signaling has been attributed to the process of store-operated calcium entry (SOCE), which is normally mediated by the ER Ca2+ sensor STIM1. The presence of mutant CALR destabilizes a complex between CALR, ERp57, and STIM1, leading to increased SOCE and thus cell proliferation.33 Ca2+ signaling has also been shown to regulate megakaryocyte function34 and could therefore contribute to phenotypic differences between distinct types of CALR mutations, as discussed further below.
It is difficult to predict whether C-terminal mutations would have a significant structural effect on CALR as they are in a region with a great degree of plasticity35; most structural studies of CALR to date have focused on the more structured N-terminal regions of the protein.36 Structural modeling analysis predicts that the C-terminus is intrinsically disordered in both wild-type and mutant contexts.37 Another consequence of CALR frameshift mutations is the loss of the C-terminal KDEL sequence, typically responsible for ER retrieval, resulting in a shift to ER-Golgi intermediate and Golgi compartments compared to WT CALR.24 Mislocalized mutant CALR could therefore produce ectopic effects. For instance, a recent report proposed that mutant CALR interacts with the transcription factor Friend leukemia integration-1 (FLI1) and conveys it to the nucleus, where it regulates the MPL promoter.38 However, this may be a consequence of enhanced JAK2 signaling rather than CALR translocating FLI1 to the nucleus, as FLI1 has been previously detected in the nucleus of megakaryocytes in JAK2-mutated ET patients.39 In any case, topological analyses of subcellular localization are complicated by the low expression of mutant CALR protein, which is significantly less stable than its wild-type counterpart.22-24, 40
Animal models
In addition to extensive work in cellular systems, several groups have also developed animal models to investigate the effects of mutant CALR. In zebrafish embryos, the injection of human type I but not type II mutant CALR mRNA resulted in an increase in CD41+ thrombocytes and a Mpl-dependent thrombocytosis that was abrogated using JAK1/JAK2 inhibitors.41 Most in vivo work to date has been performed in mouse models. In an early study using transplant of retroviral transduced bone marrow cells into lethally irradiated mice, type I and, to a lesser extent, type II mutant CALR produced thrombocytosis, with type I also showing eventual progression to myelofibrosis. This phenotype was MPL-dependent and accompanied by expansion of hematopoietic stem and progenitor cells (HSPCs) and the megakaryocytic lineage.42 A second retroviral model of the type I mutation showed similar results. In this case, a modest expansion of the Lin-Sca1+cKit+ (LSK) compartment, which is enriched for HSPCs, was observed.20 Similarly, transgenic expression of type I mutant CALR also produced an ET-like phenotype associated with increased numbers of HSPCs and megakaryocyte progenitors (MkPs), though HSPCs had no advantage in secondary competitive transplants.43
Species-specific codon preferences mean that frameshift deletions or insertions in the mouse locus would generate a substantially different amino acid sequence to that seen in patients.44 We therefore generated a mouse model in which DNA encoding the human novel C-terminal peptide associated with the type I mutation was knocked into the endogenous mouse Calr locus (ie, a humanized version of the CALR mutation). This approach yielded a hybrid protein with most of the mouse protein intact, but ending in the novel human sequence at the C-terminus, and ensuring an appropriate level of expression under the control of endogenous elements. This model also developed a strong ET-like phenotype, with a two- to three-fold increase in platelet levels, but did not progress to myelofibrosis. When bred to homozygosity, mice developed extreme thrombocytosis (platelet counts greater than 9 × 106/μL) as well as splenomegaly, bone marrow fibrosis, and a further increase in the number of HSCs and MkPs. Interestingly, HSCs harboring mutant CALR had no advantage over their wild-type counterparts in transplantation experiments,44 an observation reminiscent of results from JAK2 V617F knock-in mice.45 Studies engineering frameshift deletions into the endogenous murine locus have typically shown a less prominent phenotype: use of a CRISPR-Cas9 approach to generate a 19-bp deletion in murine Calr yielded only a mild thrombocytosis and weak activation of JAK-STAT signaling.46 Similarly, a recently published mouse model used a similar approach to engineer a 52- or 61-bp deletion in the endogenous mouse locus. The deletions led to increases in platelet levels of 35% and 15% respectively, with the 52-bp deletion also yielding a slow-rising advantage in transplantation experiments. The relatively mild phenotype could be attributed to weak activation of murine MPL by murine mutant CALR protein.47
Together, animal studies have shown that expression of the human type I CALR mutant C-terminus in hematopoietic cells drives thrombocytosis and is associated with an expansion of the HSPC compartment, though transplantation experiments suggest these cells have no or only a slight competitive advantage.43, 44 All models show increased numbers of MKs within the bone marrow, and some models additionally show myelofibrosis at higher levels of mutant CALR expression, whether as a consequence of retroviral expression42 or homozygosity.44 However, some questions remain unresolved. First, why do mouse models show no or minimal HSC advantage when human patients typically show a clonal disease? This may be due to varying genetic backgrounds and/or additional mutations in patients that are not present in mouse models. In addition, aging typically affects the microenvironment to which HSCs are exposed, which could explain the association of MPNs with increasing age in human patients. Finally, transplantation experiments represent a form of stress hematopoiesis in contrast to the steady state hematopoiesis occurring in patients. The recent use of neutral somatic mutations as barcodes has allowed the study of steady-state hematopoiesis in humans for the first time48 and will additionally permit exploration of stem cell behavior and clonal dynamics in MPN patients. Another outstanding issue is the inability of type II CALR mutations to render a phenotype in animal models. While both type I and II CALR mutations are associated with disease in humans, it is currently unknown why only type I CALR mutant is able to drive an overt myeloproliferative phenotype in both mouse and zebrafish modeling, with type II CALR mutant described to drive mild or no thrombocytosis. Type II mutants may be unable to bind non-human MPL or efficiently activate downstream signaling.
Clinical aspects
Clinical manifestations
Both initial studies identifying CALR mutations noted a distinct clinical picture linked with CALR lesions compared to other driver mutations: CALR mutations were associated with higher platelet counts, lower WBC count, lower incidence of thrombosis, and better survival compared with JAK2 V617F patients.1, 2 Two meta-analyses and distinct cohorts of patients later corroborated these findings.49, 50 Analysis of mutations in individual hematopoietic clones showed an early acquisition of the lesion, compatible with an initiating event.1, 2 In addition, CALR mutations were found in patient hematopoietic stem cells and multipotent progenitors.2 Taken together, these results agree with previously discussed studies showing that CALR mutations serve as a true driver of transformation.
Clinical differences have also been noted between distinct types of CALR lesions, with type I mutations seen significantly more frequently in MF than in ET.1, 2, 4, 51-53 In addition, differences in clinical behavior have been reported between type I and type II CALR mutations both in ET, where type II CALR mutations were associated with a significantly higher platelet count,52, 54 and in MF, where type I patients displayed a higher percentage of circulating blasts and frequency of mutations in EZH2.3
Thrombosis is the main cause of morbidity and mortality in MPN patients, particularly in polycythemia vera (PV) and ET.55, 56 Thrombosis incidence in CALR patients was originally reported to be less than half of that reported in JAK2 V617F patients.1 However, a multivariate analysis in a large cohort of 1053 ET patients showed that differences in thrombosis incidence are not associated with the mutation per se but related to the differences in age and history of previous thrombosis between CALR and JAK2 V617F-mutated patients.57 This was further confirmed in a smaller cohort, where the impact of CALR mutations on the risk of thrombosis was restricted to the group of patients younger than sixty.58 Differences in the risk of thrombosis between type I and II CALR mutations were suggested in one study4 but failed to reach statistical significance in a larger collaborative study with 1027 patients.54 A comparison of different leukocyte and platelet activation markers linked with thrombosis in ET patients found no statistically significant differences between CALR mutated and non-mutated patients.59
Myelofibrotic transformation was reported to be significantly higher among CALR-mutated ET patients than JAK2 V617F patients in one initial report.2 Follow-up studies were inconsistent, some showing no increased risk of transformation,49, 50 but 1 large-scale study again found a higher risk of transformation to MF.60 Interestingly, the increase in the incidence of MF transformation among CALR-mutated ET patients appears to be restricted to type I mutations while patients with type II mutations displayed no differences to JAK2 V617F patients.4 This is in agreement with a recent study on post-essential thrombocythemia myelofibrosis (PET-MF) showing a time to MF progression significantly longer in type II than in type I CALR and JAK2 V617F mutations.61 As a consequence, type I mutations were overrepresented in PET-MF while in ET the distribution of the two most common CALR lesions was balanced.61 Importantly, no transformation from CALR-mutated ET to PV has been reported in any of the published cohorts.2, 49, 50 This stands in stark contrast to ET associated with JAK2 mutations and may reflect the lack of interaction between mutant CALR and EPOR.
Leukemic transformation was shown to be significantly lower in patients with CALR-mutated ET compared to those with JAK2 V617F mutated ET using a competing risk approach, but the differences did not reach statistical significance after adjusting for age.49 A recent retrospective study found that CALR-mutated ET had a lower incidence of leukemic transformation compared to JAK2 V617F mutation and that the leukemic risk was not significantly affected by myelofibrotic transformation in a multivariate analysis.62 No differences in leukemic transformation in patients with MF51, 63 or leukemia-free survival64 have been found.
Overall survival (OS) was increased in CALR-mutated patients compared to JAK2 V617F-mutated patients after correction for disease phenotype and the patient cohort1; this was confirmed in MF using models that also corrected for patient age.17, 49 Some reports have found a significantly longer survival in type I CALR-mutated MF compared to type II,3, 65 while others reported similar trends that did not reach statistical significance.4, 66 In ET patients, no difference in OS between type I-like and type II-like patients was reported.67 A recently published meta-analysis and large collaborative study have confirmed that CALR type I but not type II mutations are associated with a superior overall survival.64, 68 CALR- and JAK2-mutated MPNs are broadly similar in their spectra of co-occurring mutations.69 Interestingly, type I-like CALR mutations in MF are not only associated with longer survival but may also correct the detrimental effect of ASXL1 and SRSF2 mutations, typically linked to a poorer prognosis.64, 70
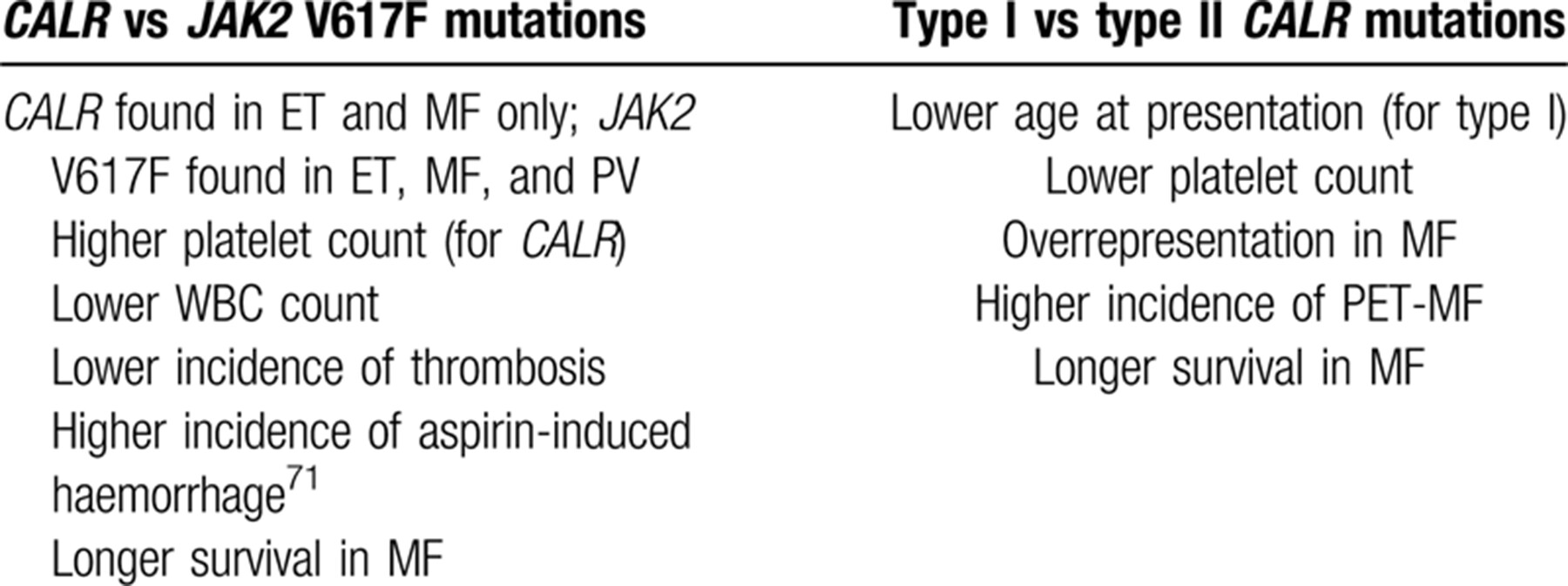
Overall, CALR mutations tend to be associated with a more benign natural history compared to JAK2 V617F-mutated disease. Differences between type I and II CALR mutations are also seen (Table 1), but the biological basis for this difference remains unclear.
Diagnostic approaches
CALR mutations are almost exclusively confined to ET and MF patients, though they were also identified in rare cases of myelodysplastic syndromes (including refractory anemia with ring sideroblasts (RARS)) and myelodysplastic-myeloproliferative syndromes.1, 2 CALR point mutations have also been described in some cases of chronic neutrophilic leukemia.72, 73 Due to their role as oncogenic drivers, CALR mutations have recently been added to the list of mutations considered major diagnostic criteria for ET and MF in the World Health Organization classification of hematological malignancies.74 The screening for these mutations is part of the current diagnostic work-up for suspected ET and MF, usually after obtaining a negative result for the JAK2 V617F mutation.75, 76 Increasing amounts of genetic data for patients have also allowed the classification of MPNs based on their underlying biological mechanisms, not solely clinical features, resulting in improved prognostic predictions.60
As more than 50 distinct CALR mutations have been described in ET and PMF and all of them are insertions or deletions, 2 main molecular diagnostic strategies are currently used: Sanger sequencing and fragment analysis, with the latter the most practical approach in terms of sensitivity and efficiency.77 Other alternative methods have been proposed, including high resolution melting curve analysis and real-time PCR, but these techniques have been validated for only the two most frequent mutations and offer only modest sensitivity improvements over fragment analysis.78 Next generation sequencing (NGS) strategies are quite attractive since the detection of additional mutations in MPN has a proven prognostic value. However, accurate indel variant calling is still challenging and distinguishing them from technical errors remains difficult.79, 80
Treatment
The treatment goals for ET and MF patients are the same irrespective of the driver mutation: controlling the symptoms and extending the lifespan of the patients by reducing their thrombohemorrhagic risk. In ET, young patients without thrombotic risk factors generally benefit from thromboprophylaxis with low dose aspirin, while the combination of low dose aspirin and hydroxycarbamide significantly reduces the incidence of thrombosis in patients older than 60 years or with a previous thrombosis.56, 81, 82 Other available cytoreductive agents such as anagrelide56 or interferon alfa83, 84 are used as second line options in specific cases, including young or pregnant patients requiring cytoreduction.
MF presents with a progressive clinical picture, ranging from the absence of symptoms to anemia, splenomegaly, constitutional symptoms, or transformation to acute myeloid leukemia. In contrast to ET, patients with MF tend to have a substantially reduced lifespan. However, the only curative treatment currently available for MF is allogeneic stem cell transplant. The current guidelines therefore recommend a symptom- and risk-based approach: although most patients are treated symptomatically, higher-risk and otherwise fit patients may be recommended for stem cell transplant. Management of symptoms include erythropoiesis-stimulating agents or danazol for anemia; hydroxycarbamide for splenomegaly, thrombocytosis, and leucocytosis; and ruxolitinb or fedratinib for splenomegaly and constitutional symptoms. Ruxolitinib and febratinib, both non-specific JAK inhibitors, exert their therapeutic effects through the downregulation of pro-inflammatory cytokines,85, 86 which is partially mediated via JAK1 inhibition.87
Current recommendations for ET and MF are based on clinical trials conducted prior to the discovery of CALR or JAK2 V617F mutations.56, 75, 76, 81, 82, 88 Nevertheless, as explained above, CALR-mutated patients have some distinct clinical characteristics and could potentially benefit from a more tailored management. For instance, in a recently published retrospective study in low risk ET patients, low-dose aspirin was not only unable to reduce risk of thrombosis but was also associated with an increased risk of hemorrhage.71 However, most guidelines consider that this is not enough evidence to recommend withholding aspirin in CALR-mutated ET before these results are confirmed by clinical trials.75, 76 In addition to response to antiplatelet therapy, time free from cytoreduction is also shorter in CALR-mutated ET than in JAK2-mutated ET, usually because of extreme thrombocytosis in the former.71
Most patients diagnosed with CALR-mutated MPN have a satisfactory management with current antiplatelet and cytoreductive therapies, though some MF patients fail to respond to the currently available therapy. CALR mutation status does not significantly influence the outcome of treatment with ruxolitinib, as shown by retrospective analysis of CALR-mutated patients in the COMFORT-II trial.89 In contrast, CALR mutations, particularly type I, are associated with a better overall survival and spleen response in patients treated with momelotinib, a JAK1/2 inhibitor.90, 91 Similarly, CALR mutations were found to be an independent factor for lower non-relapse mortality (NRM), improved progression free survival (PFS), and OS following allogenic bone marrow transplant in patients with MF, despite the large proportion of CALR-positive patients with intermediate-high and high risk scores at the time of transplantation.92 In another series of patients, those with CALR mutations were found to have a higher probability of clearing the minimal residual disease after transplant as compared to JAK2 V617F and MPL-mutated patients93; this is regarded as a strong predictor of PFS.94, 95 This is in line with recent findings that type I-like CALR mutations independently predict a better outcome in allogeneic bone marrow transplants, leading to the inclusion of type I-like CALR mutations as an independent variable in MIPSS70, a prognostic system for transplantation in patients with MF.96
There has also been interest in exploiting mutant CALR antigenicity as a target for cancer immunotherapy.97, 98 Cultured CD4+ T-cells from a patient with mutated CALR were able to recognize and kill autologous CD34+ HSCs, leading the authors to speculate that vaccinating patients with mutant CALR epitopes could induce the immune system to eliminate mutation-bearing HSCs.98 A further analysis of mutant CALR associated neo-antigens identified a subset of potential interest for immunotherapy.99
Future directions
In the 6 years since the first description of CALR mutations in ET and MF patients, significant insight has been gained into their biochemical and cell biological consequences and their clinical implications. It is clear that the primary mechanism of CALR-driven transformation lies in its interaction with MPL, which triggers JAK2-dependent signaling pathways, although it remains to be seen whether mutant CALR may also act through other pathways, such as Ca2+ signaling or transcriptional regulation.
Mouse models of CALR mutations consistently exhibit ET and MF-like phenotypes and can be used in the development of new targeted therapies. These models also raise new questions concerning the fundamental biology of CALR mutations. First, while both type I and type II mutations are associated with disease in humans and produce autonomous cell growth in several cell lines, only the former give rise to a consistent thrombocytosis phenotype in mice. Secondly, in contrast to ET and MF patients, CALR mutations do not confer a strong competitive advantage to HSCs. Further exploration of these intriguing observations will serve to illuminate the mechanisms by which CALR mutations cause disease.
Improved technologies and decreasing costs of sequencing have led to the generation of a wealth of genomic data on patients with MPNs. A knowledge bank approach has revealed a new genomic classification of the MPNs based on their underlying biological causes and has also allowed the development of personalized prognoses for individual patients.60 Furthermore, single-cell approaches tracking somatic mutations are now being used in humans to examine clonal dynamics in healthy, steady-state hematopoiesis. Extension of these techniques to hematopoiesis in MPN, particularly at multiple time points through disease progression and treatment, will further illuminate the mechanisms underlying these diseases.