Outcomes of Older Patients with NPM1 Mutated and FLT3-ITD Negative Acute Myeloid Leukemia Receiving Allogeneic Transplantation
This study was supported by Deutsche José Carreras Stiftung e.V. (04R/2016 [SS], PS15/15 [J. Grimm]), Verein Zusammen gegen den Krebs e.V. [SS].
The authors declare no conflict of interest.
Supplemental Digital Content is available for this article.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Website (www.hemaspherejournal.com).
Abstract
Supplemental Digital Content is available in the text
At diagnosis most acute myeloid leukemia (AML) patients are older (>60 years) and outcomes in this group are generally inferior compared to younger patients. Mutations in the nucleophosmin 1 (NPM1) gene are common and associate with a more favorable prognosis in younger and older AML patients.1 The European LeukemiaNet (ELN) classifies AML patients with NPM1 mutations and absence of FLT3-ITD (NPM1 mut/FLT3-ITDneg) into the favorable genetic risk group.2 Due to the favorable prognosis an allogeneic hematopoietic stem cell transplantation (HSCT) in first complete remission (CR) is generally not recommended in these patients.3 However, in younger NPM1-mutated AML patients there is growing evidence that, depending on donor availability, HSCT in CR1 may be superior to consolidating chemotherapy or autologous HSCT.4, 5 In older NPM1 mut/FLT3-ITDneg AML patients the best consolidation treatment is still under debate.
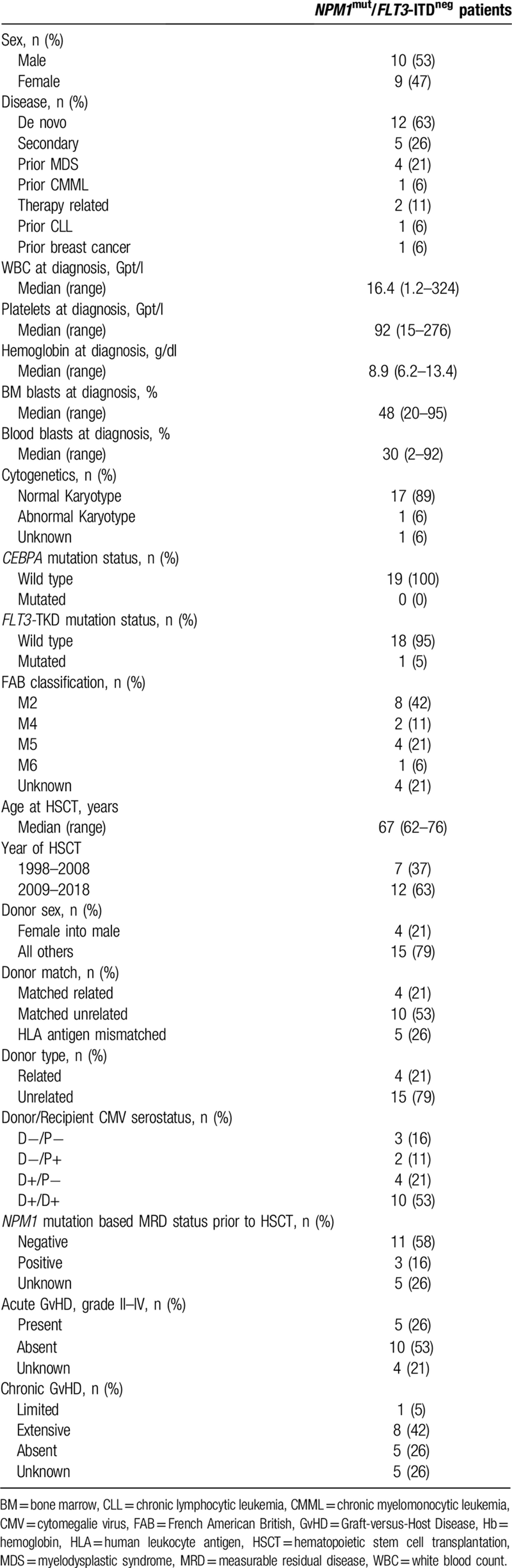
We identified 157 AML patients 60 years or older who were not eligible for myeloablative HSCT or an autologous transplantation and who received NMA-HSCT in CR1 between 1998 and 2018 at our center. Thirty-one patients harbored a NPM1 mutation and 19 were NPM1 mut/FLT3-ITDneg (Table 1). The median age at HSCT in these 19 patients was 67 (range 61–76) years. Twelve patients had de novo AML, while five patients had AML secondary to a myeloid neoplasm (4 patients after myelodysplastic syndrome, and 1 patient after chronic myelomonocytic leukemia), 2 patients had treatment-related AML (1 patient after chronic lymphocytic leukemia, and 1 patient after breast cancer). Seventeen patients had a normal karyotype, one had a trisomy 8 and trisomy 21, one karyotype was unknown. For nine patients next-generation targeted amplicon sequencing was performed at diagnosis. Additional mutations were detected in all but 1 patient (2 mutations in 2 patients, three mutations in 3 patients, and 4, 5, and 6 mutations in 1 patient each). The most commonly detected additional mutations were in DNMT3A (detected in 6 patients), NRAS (detected in 2 patients) and BCOR, IDH1, IDH2, PTPN11, SRSF2, and TET2 (detected in 2 patients each). NPM1-mutation based measurable residual disease (MRD) was available in 14 patients, 11 patients were NPM1 MRDneg and three patients were NPM1 MRDpos at HSCT.
Donors were human leukocyte antigen matched related (n = 4), matched unrelated (n = 10) or had at least one antigen mismatch (n = 5). All patients received peripheral blood NMA-HSCT with 3 × 30 mg/m2 fludarabine and 2 Gy total body irradiation.6 Immunosuppression was cyclosporine A and mycophenolat mofetil (2 and 3 g per day after related or unrelated HSCT, respectively). Median follow up after HSCT was 5.2 (range 1.5–12.5) years.
Prior to HSCT, all but 1 patient (who received 2 cycles of azacitidine) received intensive induction chemotherapy before HSCT. One patient suffered graft rejection 37 days after HSCT and received a second HSCT. At 2 years patients in this NMA-HSCT treated cohort of older NPM1 mut/FLT3-ITDneg AML had a relapse rate of 11% (95% Confidence Interval (CI) 2%–29%) and an OS of 68% (CI 50%–93%, Fig. 1). The 2-year NRM was 21% (CI 6%–42%). However, at 5 years NRM rose to 43% (CI 18%–67%) and OS dropped to 46% (CI 27%–80%), while the relapse rate remained at 11%. The 2 patients suffering relapse after HSCT had detectable NPM1-mutation based MRD prior to HSCT. Grade II-IV GvHD and III-IV acute GvHD occurred in 33% and 13%, respectively. Extensive chronic GvHD was observed in 57%. Causes of deaths were relapse (n = 2), GvHD (n = 3), infection (n = 3) and one fatal ventricular arrhythmia (for detailed patient information see Supplemental Table S1, Supplemental Digital Content, http://links.lww.com/HS/A57).
Even with the low number of patients, our results also demonstrate that the long-term consequences of HSCT, including GvHD and prolonged immunosuppression and the impact on OS - especially in older AML patients - should not be underestimated.
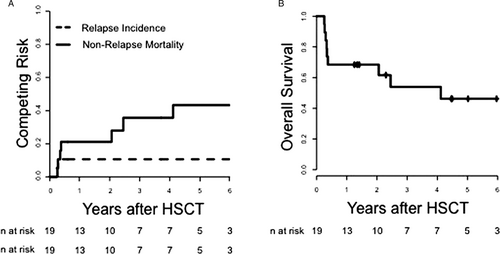
(A) Relapse Incidence, Non-Relapse Mortality, and (B) Overall Survival of older AML patients (>60 years) with NPM1 mutation and absence of FLT3-ITD receiving NMA-HSCT in first complete remission (n = 19).
In a recent report, Aldoss et al published a retrospective analysis of 17 older (>60 years) NPM1 mut/FLT3-ITDneg AML patients who underwent HSCT in CR1.7 The median age in this study was 66 (range 61–73) years with the majority of patients harboring a normal karyotype. All but 1 patient, who received azacitidine alone, were treated with intensive induction chemotherapy followed by HSCT. Patients received reduced-intensity conditioning (RIC) with fludarabine and melphalan; 1 patient underwent non-myeloablative conditioning (NMA) with fludarabin, cyclophosphamid and total-body irradiation. Outcome results of this analysis were very favorable with a 2-year overall survival (OS) and disease free survival (DFS) of 88% and 81%, respectively, a 2-year non-relapse mortality (NRM) of 12% and a 2-year relapse rate of 7%. Acute grade II-IV graft-vs-host disease (GvHD) and III-IV acute GvHD occurred in 27% and 13%, respectively.
Considering results from historical non-transplant reports for this age group (≥608, 9 or ≥6510 years) HSCT-based consolidation demonstrated improved outcomes.7-10 A possible biological background for these findings may be the presence of an allogeneic immune response mediated by CD4+ and CD8+ donor T lymphocytes against the mutated region of NPM1.11, 12 These results may challenge the general perception of chemotherapy consolidation as an adequate approach in older favorable-risk AML and also affects the question about the best time-point of HSCT in these patients.
The patients included in our analysis had similar characteristics as the patients analyzed by Aldoss et al (Supplemental Table 1, Supplemental Digital Content, http://links.lww.com/HS/A57).7 However, the main differences between the 2 studies are in the conditioning regimen applied (RIC vs NMA) and the GvHD prophylaxis. Limitations of our analysis are particularly the number of included patients and a potential selection bias towards HSCT.
Even though the outcomes observed in our NMA-HSCT treated group of older NPM1 mut/FLT3-ITDneg AML patients are not as favorable as the group of patients analyzed by Aldoss et al treatment results still compare favorably to the outcomes observed in historical non-transplant patients consolidated with chemotherapy alone.7-10
Both studies demonstrated low relapse rates and a more favorable outcome of older NPM1 mut/FLT3-ITDneg AML patients consolidated with HSCT, challenging the paradigm of a chemotherapy-based consolidation being sufficient in this older patient group. Certainly, the recent introduction of MRD analyses into the clinical practice may further refine the patient subpopulation that benefit from HSCT and emerging new therapies – for example, the combination of venetoclax and hypomethylating agents - may modulate the prognosis in this patient group. However, a randomized multi-center clinical trial – with adequate follow-up - would be desirable to identify those patients who benefit from an early HSCT in this group. Furthermore, the question of the best conditioning regimen for these patients (eg, NMA vs RIC) and whether a modification of conditioning regimens and/or GvHD prophylaxis might improve outcomes remains to be answered and should be addressed.
Acknowledgements
The authors thank Janet Bogardt, Annette Jilo, Ines Kovacs, Kathrin Wildenberger, Scarlett Schwabe, Christine Günther, Daniela Bretschneider, Evelin Hennig, and Christel Müller for their assistance.