P1299: OUTCOMES OF YOUNG ADULTS (AGED ≤40 YEARS) WITH NEWLY DIAGNOSED MULTIPLE MYELOMA AFTER UPFRONT AUTOLOGOUS STEM CELL TRANSPLANT
Abstract Topic: 22. Stem cell transplantation - Clinical
Background: There is growing recognition that young adults with cancer have unique biological characteristics, clinical features, and treatment outcomes. Multiple myeloma (MM) is primarily a disease of the elderly with a median age of diagnosis between 65–70 and fewer than 2% of patients are less than 40 years of age at diagnosis. There is a paucity of data regarding adolescent and young adult (AYA) MM patients undergoing autologous hematopoietic stem cell transplantation (auto-HCT), which is standard of care for eligible patients with newly diagnosed MM.
Aims: We sought to evaluate the long-term outcomes of young adult MM patients, aged ≤40 years, who underwent auto-HCT at MD Anderson Cancer Center.
Methods: We conducted a single-center chart review-based analysis. We searched for MM patients 15-40 years of age who received upfront auto-HCT between 1989 to 2021. Progression free survival (PFS) and overall survival (OS) were estimated using Kaplan-Meier method and differences between groups were assessed using the log-rank test. Associations with survival outcomes were determined using Cox proportional hazards regression models. Response post transplant was included in the models as a time-dependent covariate.
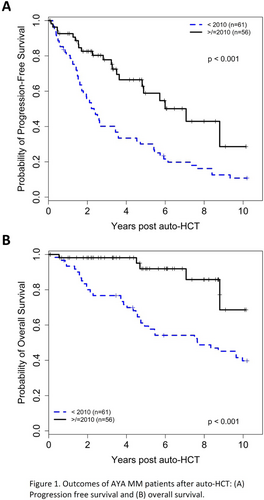
Results: A total of 117 patients were included in our analysis. Median age was 37 (range 22-40) years and 69 (59%) patients were male. There were 61 (52%) and 56 (48%) patients who underwent auto-HCT before and after 2010, respectively. High-risk cytogenetic abnormalities were found in 15% of the patients. As expected by the young age of the cohort, most patients had a low burden of comorbidities (HCT-CI ≤ 3, 73%). Following induction and prior to auto-HCT, 12 (10%) and 52 (44%) of patients achieved at least complete response (CR) or very good partial response (VGPR), respectively (Table 1). Median follow-up in survivors was 72.6 (range 0.9-238) months. Day 100 and best post-transplant responses were ≥CR in 32% and 56%, and ≥VGPR in 63% and 77% of patients, respectively. For the entire cohort, median PFS was 43.1 (95% CI 31.2–65.0) months and median OS was 146.6 (95% CI 100.0-208.1) months. Patients transplanted after 2010 had better median PFS [(84.9 months 95% CI 57.8-not reached (NR)) vs. (28.2 months 95% CI 20.5-41.3), p<0.001; Figure 1A] and OS [(NR 95% CI 105.6-NR) vs. (91.8 months 95% CI 56.0-146.6), p<0.001; Figure 1B] compared to those transplanted prior to 2010.
In multivariable analysis, achieving ≥CR as best post-transplant response was associated with improved PFS (HR 0.56, 95% CI 0.32-0.95, p=0.033), and achieving ≥VGPR as best post-transplant response was associated with improved OS (HR 0.24, 95% CI 0.12-0.47, p<0.001). Three patients (3%) developed a second primary malignancy (colon cancer, bladder cancer and melanoma, n=1 each).
Summary/Conclusion: In this single center retrospective analysis of young adult MM patients aged ≤40 years undergoing upfront auto-HCT, depth of response following transplant was associated with improved survival outcomes. Those who underwent auto-HCT in more recent years had better PFS and OS, consistent with the continued improvement in therapy for the general MM population. OS in this younger cohort following upfront auto-HCT exceeded that reported in older patients and should be considered in assessing the efficacy of novel therapies, such as CAR-T cells and bispecific antibodies.
Keywords: Multiple myeloma, Autologous hematopoietic stem cell transplantation, Age