P457: COMPLEX CARYOTYPE IS AN INDEPENDENT RISK FACTOR IN TP53-MUTATED AML
Background: Two of the most powerful markers of adverse risk in AML are complex karyotype (CK) and TP53 mutations (TP53mut). We have shown that co-occurence of both alterations identifies a particularly adverse subgroup (Rausch et al, ASH 2022). Others have reported that biallelic TP53 alterations (biTP53) identify a very adverse subgroup (Fenwarth et al, ASH 2022, Stengel et al, Blood Adv 2023). These findings result in the question whether the negative prognostic impact of CK coexisting with TP53mut is merely a proxy for biTP53.
Aims: We aim to characterize the influence of TP53 allelic status and CK in AML.
Methods: We studied 1,118 newly diagnosed AML patients (median age 57 years; range, 18–86 years) who received cytarabine-based induction chemotherapy in two subsequent multicenter phase III trials of the German AML Cooperative Group between 1999 and 2012. No patient received FLT3 inhibitors or gemtuzumab ozogamicin during first-line treatment. Median follow-up for of survivors was 98 months. A TP53mut with variant allele frequency (VAF) <60% and without TP53-associated cytogenetic changes (-17, del17p, other 17p abnormalities; TP53cyto), or TP53cyto without TP53mut were considered monoallelic TP53 alterations (monoTP53). A TP53mut with VAF <60% coexisting with TP53cyto or a TP53mut with VAF ≥60% were considered biallelic alterations (biTP53).
Results: Of 1118 patients, 99 had TP53mut (40 monoTP53, 59 biTP53) (Table 1). Of 101 patients with CK, 16 had TP53cyto, 19 had a TP53mut and 42 had both. Only 23 had a CK without TP53 alteration (Table 1). Results are also shown for 1105 patients intensively treated on trials of the AMLSG.
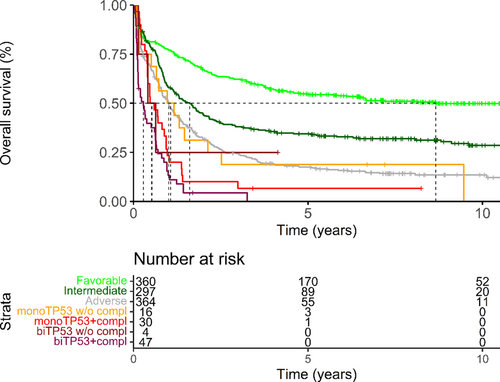
Those with biTP53 had worse outcomes than ELN-2022 adverse-risk patients without TP53 alteration (5y OS 0% v 18%, p=0.0007). Those with monoTP53 achieved similar outcomes to TP53-unaltered adverse risk cases (5y OS 13%, p=0.18). In our small analysis, their outcomes were not significantly better than those of biTP53 (p=0.057).
| TP53mut | no TP53cyto, no CK |
TP53cyto w/o CK |
CK w/o TP53cyto |
TP53cyto and CK |
|---|---|---|---|---|
| AMLCG cohort | ||||
| none | 995 (89%) | 2* (<1%) | 23 (2%) | 16* (1%) |
| VAF<60% | 15* (1%) | 1† (<1%) | 9* (<1%) | 16† (1%) |
| VAF>60% | 3† (<1%) | 0† (<1%) | 11† (1%) | 26† (2%) |
| AMLSG cohort | ||||
| none | 929 (81%) | 6* (<1%) | 68 (%) | 19* (2%) |
| VAF<60% | 13* 1(%) | 0† (<1%) | 13* (1%) | 18† (2%) |
| VAF>60% | 2† (<1%) | 1† (<1%) | 12† (1%) | 24† (2%) |
- * monoTP53, †biTP53
An exploratory analysis shows similar 5y OS of biTP53 with (0%) and without CK (0%) as well as monoTP53 with CK (8%) while all three groups seem to do worse than monoTP53 without CK (19%) or adverse-risk unrelated to TP53 (18%; Figure). BiTP53 with CK did significantly worse than monoTP53 without CK (p=0.004) or adverse cases without TP53mut or TP53cyto (p=0.0005).
The validation cohort confirmed these findings. Here, biTP53 with and without CK as well as monoTP53 with CK have worse 5-year OS (0% for all) than monoTP53 without CK (17%) or adverse-risk unrelated to TP53 (26%). BiTP53 with CK performed significantly worse than monoTP53 without CK (p=0.02) or adverse cases without TP53mut or TP53cyto (p<0.0001).
In a cox-model for OS which included age, sex, AML type, WBC count, BM Blast count, monoTP53, biTP53 and CK, CK remained independently prognostic (HR for death 1.6; CI 1.2-2.3).
Summary/Conclusion: In this large cohort of fit AML patients those with biTP53 – most of which also had CK - had worse outcomes than those with monoTP53, which is in line with previous reports. However, monoTP53 with CK did just as badly as biTP53. This finding not only confirms the independent adverse impact of CK for TP53mut patients, it also establishes monoTP53 with CK as another very high risk group besides biTP53.
Keywords: ELN, Complex aberrant karyotype, TP53, AML