Stereotactic Radiosurgery for Glomus Jugulare Tumors†
Presented at the 102nd Annual Meeting of the American Laryngological, Rhinological and Otological Society, Inc., Palm Desert, California, April 26, 1999.
Abstract
Objectives/Hypothesis: Surgery is considered to be the mainstay of treatment for glomus jugulare tumors. A subset of patients are poor surgical candidates based on age, medical problems, tumor size, or prior treatment failure. The purpose of this study was to review our results with stereotactic radiosurgery (gamma knife treatment) in this group of patients, with particular attention to adverse reactions and symptom relief.
Study Design: Retrospective review and phone survey.
Methods: Charts were reviewed for size and location of tumor, history of previous treatment, symptoms before and after treatment, amount of radiation received, acute and late complications, and functional level before and after treatment. Pretreatment and posttreatment magnetic resonance imaging scans were also reviewed. Identified patients were then contacted for a phone interview.
Results: Eight patients were identified. Phone interviews were conducted with four patients. Four patients had failed previous treatment. Follow-up ranged from 7 to 104 months. One patient experienced an acute complication: intractable vertigo requiring hospitalization. No patient experienced delayed cranial neuropathies. No patient reported worsening of any of the following symptoms: pulsatile tinnitus, hearing loss, facial weakness, hoarseness, or difficulty swallowing. Three patients reported improvement in their pulsatile tinnitus. Two patients reported improvement in hearing loss, and one patient each reported improvement in vertigo and difficulty swallowing.
Conclusions: Preliminary results suggest that stereotactic radiosurgery is useful to control symptoms and may be delivered safely in patients with primary or recurrent glomus jugulare tumors who are poor surgical candidates.
INTRODUCTION
Glomus jugulare tumors arise from the paraganglionic tissue found in the adventitia of the jugular bulb. These tumors typically occur in older patients but can be found in young adults, especially in those with familial inheritance. The treatment of glomus jugulare tumors is controversial, but has generally been surgical in nature, with radiotherapy reserved for those patients with recurrent disease or unresectable tumors. External beam radiation therapy has been found to curtail growth of glomus tumors and reduce patient symptoms with acceptable complication rates.1-3
Stereotactic radiosurgery (gamma knife treatment) is a radiotherapy technique that uses a very focused, large, single dose of radiation under stereotactic guidance. Stereotactic radiosurgery is believed to shorten overall treatment time, decrease costs, and decrease complications because less normal tissue is radiated. Several preliminary studies have shown stereotactic radiosurgery to provide symptom relief with minimal adverse effects in patients with glomus jugulare tumors.4, 5 Our purpose in performing this study was to assess whether stereotactic radiosurgery provided symptom relief with an acceptable complication rate.
MATERIALS AND METHODS
Between February 1990 and March 1998 eight patients with glomus jugulare tumors were treated with stereotactic radiosurgery in an attempt to provide symptom relief. The charts of these patients were reviewed for patient age, tumor size, history of prior treatment, symptoms before and after treatment, functional level before and after treatment, and acute and late complications. Attempts were made to contact the identified patients for a phone interview to assess specific information concerning pretreatment symptoms, posttreatment symptoms, and the time course of any change in symptoms. Posttreatment magnetic resonance imaging (MRI) scans obtained at yearly intervals after treatment were reviewed and compared with the pretreatment scans to assess changes in tumor size.
RESULTS
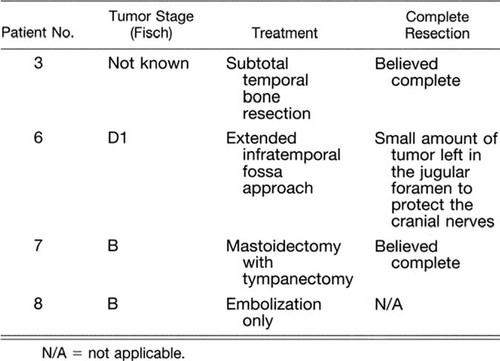
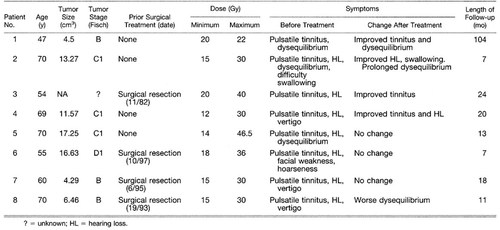
Of the eight patients identified, four were poor surgical candidates secondary to multiple medical problems or advanced age. Three patients refused surgical management. One patient underwent stereotactic radiation therapy after surgery to treat a small area of residual tumor centered at the jugular foramen in an effort to preserve cranial nerve function. Four patients had recurrent or residual tumors after prior treatment. Three patients had previous surgery and one patient had embolization of her tumor only (Table I). Four patients underwent a phone interview. One patient was deceased from causes unrelated to his glomus tumor. Three patients were unavailable for follow-up and information was obtained from their charts. The average patient age at time of treatment was 61.9 years (range, 45-70 y). Mean follow-up was 27 months (range, 7-102 mo). The mean tumor volume was 9.81 cm2 (range, 17.25-4.29 cm2). Patient information is summarized in Table II.
The mean maximal dose of radiation was 33 Gy (range, 22-46.5 Gy). The mean marginal dose of radiation was 16.3 Gy (range, 12-20 Gy).
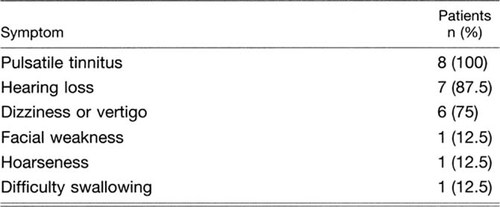
Preoperative symptoms are summarized in Table III. All patients had pulsatile tinnitus before treatment. After treatment, no patient reported worsening of any of the following symptoms: pulsatile tinnitus, hearing loss, facial weakness, hoarseness, or difficulty swallowing. One patient reported increased balance disturbance after treatment, which required her to use a cane for 11 months. Her instability has improved, and she is now able to ambulate without assistance.
Three patients reported improvement in their pulsatile tinnitus. In two patients the improvement was noted within 6 months. In one patient improvement continued over 4 years, with eventual resolution of the tinnitus. Two patients reported improvement in hearing loss within 3 months of treatment. One patient reported improvement in vertigo over a 6-month period. One patient reported improvement in swallowing within 4 weeks of treatment.
Two of the eight patients were employed before treatment. Both returned to their jobs in the same capacity after stereotactic radiosurgery.
One patient experienced an acute complication: intractable vertigo requiring admission to the hospital for several days. This patient had persistent dysequilibrium, which responded to vestibular rehabilitation and resolved 11 months after treatment. No patients experienced delayed worsening of cranial nerve function.
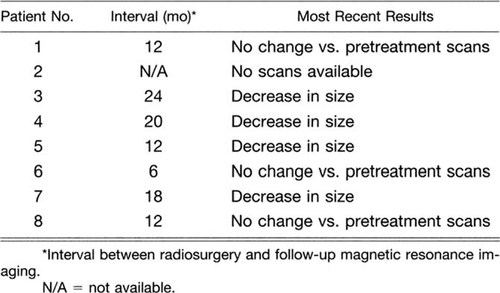
Seven patients had follow-up MRI scans or MRI scan reports available for review. The MRI scans were generally obtained at yearly intervals after stereotactic radiosurgery. Three of seven tumors remained stable in size and four decreased in size (Table IV).
DISCUSSION
Glomus jugulare tumors are indolent, locally destructive lesions arising from the paraganglionic tissue surrounding the jugular bulb. Surgery with preoperative embolization is considered by most to be the mainstay of treatment, especially in young patients. Postoperative cranial neuropathies are common and can serve to limit functional capacity after surgery.6-8 This postoperative morbidity has led to an increase in the use of radiotherapy for the treatment of glomus jugulare tumors, especially in elderly patients or those with very large tumors.
Standard fractionated radiotherapy has been shown to reduce tumor size in up to 61% of cases and decrease clinical symptoms in as many as 71% of patients.2, 9, 10 However, the reduction in tumor size averages only 23%.9 Glomus tumors are known to be relatively radioresistant, with radiation-induced fibrosis found mainly in the vessels supplying the tumor cells.11 The presence of viable tumor cells after radiotherapy has been associated with unpredictable long-term behavior of the lesion, especially before the availability of megavoltage radiotherapy.1 The side effects of external beam radiotherapy include radiation-induced second malignancy and osteoradionecrosis of the temporal bone.1, 3 Radiotherapy does appear to result in a decreased incidence of posttreatment cranial nerve palsies as compared with surgery. Radiotherapy may be advantageous over surgical resection for elderly patients, patients in poor health, patients with large tumors with intracranial extension, and patients with recurrent lesions.
Stereotactic radiosurgery delivers focused radiation in a single treatment, thereby lowering the amount of radiation exposure to normal tissue and increasing the treatment effect on slowly proliferating tissue.12 Several preliminary reports have evaluated the effectiveness of radiosurgery in the treatment of glomus tumors. Liscak et al.5 reported on 14 patients treated with stereotactic radiosurgery with an average follow-up of 20.5 months. They noted an improvement in tinnitus, vertigo, and ataxia in three patients and headache and nausea in two patients. Three patients were noted to have worsening of their hearing on the affected side. Foote et al.4 reported on nine patients treated with radiosurgery. They noted improvement in tinnitus and cranial nerve function in seven of their nine patients. Neither of these studies reported any acute or late complications, although follow-up was short in both studies.
Our results confirm those seen by Foote et al.4 and Liscak et al.5 Overall, our patients had larger tumors than both previous studies. Our mean maximal and minimal tumor doses were comparable to those of Foote et al. and Liscak et al. Improvement in one or more of the following symptoms was noted in four of eight patients: pulsatile tinnitus, hearing loss, vertigo, facial weakness, hoarseness and difficulty swallowing. We noted only one acute complication: acute vertigo, which required a short hospital stay. This patient had persistent dysequilibrium requiring aggressive vestibular rehabilitation, with eventual resolution after 11 months. One other patient did report an increase in balance dysfunction after treatment, which improved over an 11-month period. Most symptoms improved within 6 months of treatment. However, two patients required 11 months to note improvement in their balance disturbance, and one patient had gradual improvement of tinnitus over a 4-year period.
Our follow-up is not long enough to make conclusions about long-term complications. Delayed cranial neuropathies after stereotactic radiosurgery for acoustic neuromas have been known to occur as late as 3 years after treatment.13
Stereotactic radiosurgery appears to curtail the growth of glomus jugulare tumors and in some cases decrease the size of the tumor. Of seven patients with posttreatment MRI scans available for review, four had no increase in tumor size and three had a decrease in tumor size. These results must be interpreted with caution, given that our follow-up is short and glomus tumors are very slow-growing lesions. It is widely recognized that glomus tumors may start growing again many years after treatment with external beam radiation therapy. The exact incidence of re-initiation of growth remains unknown, because patients have not been systematically followed for 15 to 20 years after treatment. Whether stereotactic delivery systems provide better or worse results in this regard will not be known for many years, if ever.
Because neither external beam radiation nor stereotactic radiosurgery eliminates glomus tumors, their primary benefit to the patient rests in symptom relief, primarily relief of pulsatile tinnitus. It is noteworthy that only 37.5% of our patient population reported improvement in their pulsatile tinnitus. Although symptom relief was less than we had hoped, it should be stressed that in poor surgical candidates, any symptom relief is worthwhile, given the limited treatment options available.
CONCLUSION
We continue to believe that most glomus jugulare tumors should be managed with surgery, especially in young patients, despite the relatively high incidence of postoperative cranial neuropathy. Standard fractionated radiotherapy has been shown to halt the growth of glomus jugulare tumors and result in fewer postoperative cranial neuropathies than surgery. However, the risk of second malignancies and osteoradionecrosis makes primary radiotherapy less appealing in young patients. Stereotactic radiosurgery may decrease the above-mentioned risks by delivering focused radiation and thereby limiting the radiation dose delivered to normal tissue. Our preliminary results in a group of patients who had refused surgery or were poor surgical candidates owing to age or recurrence suggest that stereotactic radiosurgery decreases symptoms in many patients with minimal short-term complications. Tumor growth appears to have been halted or decreased in all patients with postoperative scans available, but follow-up was short. Stereotactic radiosurgery is a useful option to control symptoms and may be delivered safely in patients with primary and recurrent glomus jugulare tumors.