Left ventricular dysfunction due to diffuse multiple vessel coronary artery spasm can be concealed in dilated cardiomyopathy
Abstract
Aims
Many patients with idiopathic dilated cardiomyopathy (DCM) have been diagnosed on the basis of the exclusion of significant coronary stenosis and the presence of left ventricular (LV) dysfunction. In the present study, we investigated the possibility that coronary multispasm is one of the mechanisms leading to diffuse idiopathic DCM-like LV dysfunction.
Methods and results
Forty-two patients with severely depressed LV function but without significant coronary stenosis were enrolled (baseline LV ejection fraction, 33 ±11%). An acetylcholine (ACh) provocation test was performed at the time of coronary angiography. In patients with a positive ACh provocation test (n = 20), coronary angiography revealed multivessel diffuse coronary spasm with marked electrocardiogram changes. In patients with a negative ACh provocation test (n = 22), significant findings compatible with idiopathic DCM were more frequently observed on magnetic resonance imaging (MRI) or in LV biopsies compared with the ACh-positive group (MRI, 73% vs. 12%; and LV biopsy, 71% vs. 0%, respectively; P < 0.01). In the ACh-positive group, LV function significantly improved after the administration of calcium channel blockers (LV ejection fraction, 34 ±12% vs. 54 ±10%; and brain natriuretic peptide, 803 ± 482 pg/mL vs. 69 ± 84 pg/mL, at baseline and 1 year, respectively; P < 0.01).
Conclusions
Our results raise the possibility that patients with LV dysfunction due to repeated coronary multispasm are being diagnosed as idiopathic DCM, and that calcium channel blockers may prove to be a promising therapeutic strategy in those patients.
Introduction
In coronary spasm, sudden extreme coronary vasoconstriction produces a transient reduction in blood flow, resulting in myocardial ischaemia.1,2 In addition to causing angina, coronary spasms may lead to major adverse cardiac events, such as acute coronary syndrome, sudden cardiac death, and critical arrhythmia.3–6 Because there is a greater prevalence of coronary spasm in Japanese than Western populations, coronary spasms may have a greater influence on cardiac events in Japanese patients.2,6,7
Idiopathic dilated cardiomyopathy (DCM) is diagnosed on the basis of the exclusion of coronary artery disease, such as significant coronary stenosis and old myocardial infarction, in patients with left ventricular (LV) dysfunction. It has been thought that there is no relationship between coronary spasm and idiopathic DCM because work-up tests, such as the acetylcholine (ACh) provocation test to prove coronary spasm, are usually not performed after a diagnosis of idiopathic DCM has been made. However, in recent years, small studies have reported a correlation between coronary spasm and idiopathic DCM, demonstrating that up to one-third of idiopathic DCM patients may experience coronary spasm.8,9 Furthermore, according to a report from Japan published in 2009, multiple coronary spasms may result in transient heart failure in a small percentage of patients with heart failure of unknown origin.10 Therefore, we hypothesized that the broad diagnosis of idiopathic DCM may conceal patients with congestive heart failure or LV dysfunction due to coronary spasm.
Current evidence in the literature proves the efficacy of beta-blockers in the treatment of LV dysfunction, such as idiopathic DCM, but the value of calcium channel blockers has not been reported.11–13 There is a possibility that calcium channel blockers may prove to be key drugs if coronary spasm affects idiopathic DCM-like LV dysfunction.
Therefore, the aims of the present study were to: (i) examine the frequency of coronary spasm in patients with congestive heart failure or LV dysfunction, such as idiopathic DCM, using the ACh provocation test; and (ii) follow the clinical course after a chosen treatment in patients with and without coronary spasm by evaluating cardiac function.
Methods
Study subjects
The present study was an observational, prospective study. Between January 2007 and December 2011, 300 consecutive patients with congestive heart failure or LV dysfunction were admitted to our hospital. All patients underwent coronary angiography for the work-up of causes; 192 were found to have coronary artery disease, 66 had valvular diseases, and the remaining 42 had disease of other aetiology. Those 42 patients classified as ‘other aetiologies’ without significant coronary artery stenosis or simple valvular diseases underwent an ACh provocation test.
The present study was approved by our institution's ethics committee, and all patients provided written informed consent prior to participation.
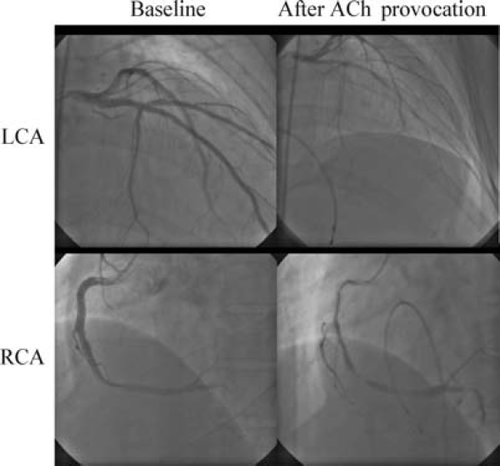
Acetylcholine provocation test
The ACh provocation test was performed as follows. First, a temporary pacing electrode was inserted into the right ventricle because the administration of ACh, especially in the right coronary artery, may cause transient episodes of severe bradycardia. Then, angiography of the left and right coronary arteries was performed in an appropriate projection that ensured the best separation of the branches of each coronary artery. Following these baseline measures, 20, 50, or 100 μg of ACh in 5 mL of physiological saline (37°C) was injected into the left coronary artery over a period of 20 s. Coronary angiography was performed 1 min after the start of each injection. The different doses of ACh were administered at 5 min intervals. Doses of 20 or 50 μg of ACh (in 5 mL of saline) were injected into the right coronary artery over a period of 20 s. Angiography of the right coronary artery was performed at the same time as that of the left coronary artery. Finally, isosorbide dinitrate was injected into each coronary artery and angiography was performed while the coronary arteries were maximally dilated.
In an ACh provocation test, coronary spasm is defined as a transient total or subtotal occlusion (>90% stenosis) of the coronary arteries with signs of myocardial ischaemia, such as ischaemic ST segment changes on electrocardiography (ECG).2
Left ventricular angiography
Left ventricular angiography (LVG) was performed just before ACh provocation at the same time during each ACh provocation test. Each segmental wall motion was evaluated in accordance with the American Heart Association classification,14 and scored as follows: normokinesis, 1 point; hypokinesis, 2 points; akinesis, 3 points; dyskinesis or aneurysmal, 4 points. Left ventricular ejection fraction (LVEF), left ventricular end-diastolic volume index (LVEDVI), and left ventricular end-systolic volume index (LVESVI) were also measured.
Coronary riskfactors
In the present study, the coronary risk factors were considered to be hypertension, dyslipidaemia, diabetes mellitus, and a history of smoking. Hypertension was defined as systolic blood pressure >140 mmHg, diastolic blood pressure >90 mmHg, or when patients were already being treated with antihypertensive medication.15 Dyslipidaemia was defined as total cholesterol (TC) >220 mg/dL, LDL-cholesterol (LDL-C) >140 mg/dL, HDL-cholesterol (HDL-C) <40 mg/dL, and triglyceride (TG) >150 mg/dL, or when patients were already being treated with antidyslipidaemic drugs.16,17 Diabetes mellitus was defined using the World Health Organization criteria.18 A history of smoking was defined as current smoking or having smoked 100 or more cigarettes in the past, irrespective of the time span.19
Laboratory examinations
After blood sampling, haemoglobin, creatinine, brain natriuretic peptide (BNP), TC, LDL-C, HDL-C, TG, fasting plasma glucose, and glycated haemoglobin (HbA1c) levels were determined. These parameters were routinely examined on admission. In addition, estimated glomerular filtration rate was determined according to age, sex, and creatinine level.20
Electrocardiogram examinations
Electrocardiograms were performed every 1–3 days during the period of hospitalization, and performed again at 1 month and 1 year in the outpatient clinic. Ischaemic findings on the ECG were defined as transient ST elevation ≥1 mm, ST depression ≥1 mm, or the new appearance of a negative T wave of ≥2 mV recorded in at least two contiguous leads on the 12-lead ECG. The time course of ischaemic changes was defined as positive when the aforementioned ischaemic findings changed during the treatment period.
Echocardiography
Echocardiography was performed at baseline, and at 1 month and 1 year after the start of medical treatment such as calcium channel blockers or beta-blockers. ‘E’ was defined as early filling peak velocity on mitral inflow measured by pulsed-Doppler focus. ‘e'’ was defined as peak early mitral annular velocity by tissue Doppler imaging. LV end-diastolic dimension (LVEDd), LV end-systolic dimension (LVESd), and LV wall thickness were measured by M-mode echocardiography. LVEF was measured using the biplane Simpson method.
Cardiac magnetic resonance imaging
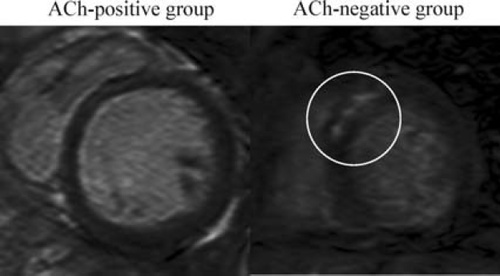
Cardiac magnetic resonance imaging (MRI) was performed on 32 of the 42 hospitalized patients. Delayed enhancement (DE) of gadolinium in the subendocardium or transmural myocardium was defined as an ischaemic pattern of DE, whereas DE in the mid-wall of the myocardium, without involvement of the subendocardium, was defined as a cardiomyopathy-type pattern.21
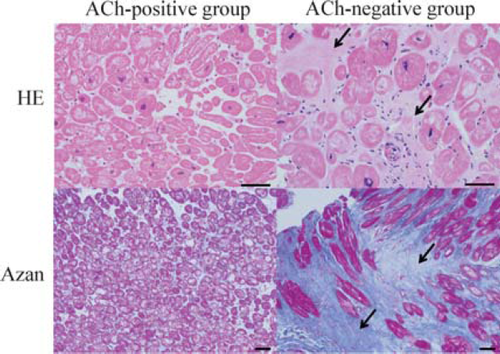
Endomyocardial biopsy
Endomyocardial biopsy was performed in 17 of the 42 patients at the same time as coronary angiography. Small myocardial pieces were obtained from the LV and fixed immediately in formalin. Subsequently, the myocardial biopsies were used for pathological investigations.
Administration of calcium channel blockers or beta-blockers
In the present study, to improve LV dysfunction, patients were administered appropriate doses of calcium channel blockers for inhibition of coronary spasm and/or appropriate doses of beta-blockers based on previous studies of the treatment of LV dysfunction. Cardiac function after treatment was analysed by echocardiography and laboratory examinations.
Statistical analysis
Significant differences were determined using the Mann–Whitney U-test or Wilcoxon's matched-pairs signed-rank test, as appropriate. Differences in frequencies were analysed using Fisher's exact probability test. Comparisons of parameters over time within each group were made by one-way analysis of variance (ANOVA), followed by Tukey's multiple comparison test. Comparisons of parameters over time between the two groups were made by two-way repeated-measures ANOVA. All data are expressed as the mean ± SD. P < 0.05 was considered significant.
Results
Characteristics of patients grouped according to results of the acetylcholine provocation test
Twenty of 42 patients (48%) were found to have significant coronary spasm on the ACh provocation test. All 42 patients in the present study were divided into two groups on the basis of the results of the ACh provocation test: those in whom the results of the ACh provocation test were positive (ACh-positive group, n = 20) and those in whom the results were negative (ACh-negative group, n = 22). In all patients in the ACh-positive group, diffuse spasm was provoked in more than two vessels, including the left anterior descending artery, during the ACh provocation test (Figure 1). In particular, most of the spasms were induced not focally, but diffusely. Furthermore, 75% of patients in the ACh-positive group had not experienced typical angina chest pain prior to their admission, and 35% did not have typical chest pain even during the ACh provocation test (Table 1). Ventricular fibrillation or ventricular tachycardia and recurrent congestive heart failure did not occur during the ACh provocation test or hospital stay.
| Patient no. | Chest pain | ECG | Angiographic findings | Dose of ACh (μg) | |||
|---|---|---|---|---|---|---|---|
| LAD | LCX | RCA | LCA | RCA | |||
| 1 | – | STD | D | D | D | 100 | 20 |
| 2 | – | STD | D | D | D | 50 | 20 |
| 3 | – | STD | D | D | D | 20 | 20 |
| 4 | + | STE | D | D | X | 50 | X |
| 5 | – | STE | D | D | D | 20 | 20 |
| 6 | – | STE | D | D | X | 20 | X |
| 7 | – | STD | D | D | D | 50 | 50 |
| 8 | – | STD | D | D | N | 50 | 50 |
| 9 | + | STD | D | D | F | 50 | 50 |
| 10 | – | STD | D | D | D | 50 | 20 |
| 11 | – | STD | D | D | D | 50 | 50 |
| 12 | + | STE | D | D | D | 50 | 20 |
| 13 | – | STD | D | N | D | 50 | 50 |
| 14 | – | STE | D | F | X | 50 | X |
| 15 | + | STD | D | D | N | 100 | 50 |
| 16 | – | STD | D | D | X | 50 | X |
| 17 | + | STD | D | N | D | 100 | 50 |
| 18 | + | STE | D | D | X | 20 | X |
| 19 | – | STD | D | D | D | 50 | 20 |
| 20 | + | STD | D | D | X | 50 | X |
- a ECG, electrocardiography; LAD, left anterior descending artery; LCA, left coronary artery; LCX, left circumflex artery; RCA, right coronary artery.
- b In chest pain findings, – indicates that no remarkable chest pain occurred, and + indicates that the patient felt chest pain. In the ECG findings, STE indicates ST segment elevation and STD indicates ST segment depression or T wave inversion. In angiographic findings, D indicates diffuse coronary spasm, F indicates that spasm was recognized focally in coronary arteries, N indicates that no remarkable spasm was recognized, and X indicates that an acetylcholine provocation test was not performed.
At baseline, there were no significant differences in cardiac function, as evidenced by LVEF, LVEDd, LVESd, LV mass index, and BNP concentrations, between the ACh-positive and ACh-negative groups (Table 2). However, there were significant differences between the two groups with regard to the prevalence of hypertension and a history of smoking. The percentage of patients with a history of smoking, which includes not only current smokers but also experimental smokers, was higher in the ACh-positive group (75% vs. 27%, P < 0.05), and the prevalence of current smoking was also higher in the ACh-positive group (55% vs. 18%, P < 0.05). These findings mean that patients in the ACh-positive group had more coronary risk factors than those in the ACh-negative group.
| ACh-positive (n = 20) | ACh-negative (n = 22) | P-value | |
|---|---|---|---|
| Age (years) | 61 ± 14 | 63 ± 11 | NS |
| No. of men (%) | 15 (75) | 15 (68) | NS |
| Coronary risk factors | |||
| Hypertension | 16 (80) | 9 (41) | <0.05 |
| Dyslipidaemia | 11 (55) | 10 (45) | NS |
| Total cholesterol (mg/dL) | 170 ± 37 | 176 ± 42 | NS |
| HDL-C (mg/dL) | 43 ± 11 | 49 ± 14 | NS |
| LDL-C (mg/dL) | 108 ± 27 | 112 ± 39 | NS |
| Triglyceride (mg/dL) | 94 ± 52 | 107 ± 88 | NS |
| Diabetes mellitus | 7 (35) | 5 (23) | NS |
| Smoking | 15 (75) | 6 (27) | <0.05 |
| Haemoglobin (g/dL) | 13.8 ± 1.3 | 14.0 ± 2.4 | NS |
| eGFR (mL/min/1.73m2) | 68 ± 18 | 69 ± 26 | NS |
| BNP (pg/mL) | 863 ± 514 | 686 ± 572 | NS |
| Electrocardiography | |||
| LBBB | 3 (15) | 5 (23) | NS |
| LVH | 1 (5) | 4 (18) | NS |
| Atrial fibrillation | 5 (25) | 4 (18) | NS |
| Echocardiography | |||
| LVEF (%) | 32 ± 11 | 34 ± 11 | NS |
| LVEDd (mm) | 60 ± 7 | 61 ± 9 | NS |
| LVESd (mm) | 50 ± 9 | 49 ± 10 | NS |
| RWT | 0.37 ± 0.07 | 0.39 ± 0.11 | NS |
| LVMI (g/m2) | 171 ± 41 | 174 ± 36 | NS |
| E (cm/s) | 85 ± 37 | 85 ± 25 | NS |
| e' (cm/s) | 5 ± 2 | 5 ± 2 | NS |
| E/e' | 17 ± 7 | 17 ± 7 | NS |
| Haemodynamics | |||
| mRAP (mmHg) | 5 ± 3 | 6 ± 3 | NS |
| mPAP (mmHg) | 19 ± 6 | 22 ± 8 | NS |
| PCW (mmHg) | 10 ± 5 | 14 ± 8 | NS |
| CI (L/min per m2) | 2.2 ± 0.4 | 2.5 ± 0.7 | NS |
| Observation period (days) | 199 ± 177 | 220 ± 247 | NS |
- a Data are presented as the mean ± standard deviation or as the number of patients in each group with percentages given in parentheses, as appropriate.
- b ACh, acetylcholine; BNP, brain natriuretic peptide; CI, cardiac index; E, early diastolic transmitral flow velocity; e', mitral annulus velocity; eGFR, estimated glomerular filtration rate; HDL-C, high-density lipoprotein-cholesterol; LBBB, left bundle branch block; LDL-C, low-density lipoprotein-cholesterol; LVEDd, left ventricular end-diastolic dimension; LVEF, left ventricular ejection fraction; LVESd, left ventricular end-systolic dimension; LVH, left ventricular hypertrophy; LVMI, left ventricular mass index; mPAP, mean pulmonary arterial pressure; mRAP, mean right atrial pressure; NS, non-significant; PCW, pulmonary capillary wedge pressure; RWT, relative wall thickness.
Findings on left ventricular angiography
Left ventricular angiography was not performed in four patients in the ACh-positive group and in one patient in the ACh-negative group so as to avoid aggravating renal dysfunction by overload of contrast agents. Thus, LVG was performed in 16 patients in the ACh-positive group and 21 patients in the ACh-negative group. There were no significant differences in LVEF, LVEDVI, LVESVI, and segment wall motion scores between the two groups (Table 3). Furthermore, our results demonstrated that LV wall motion was diffusely depressed in both groups. These findings suggest that coronary spasm was occurring in multiple coronary vessels in the ACh-positive group, which is consistent with the results of the ACh provocation test shown in Table 1.
| ACh-positive group (n = 16) | ACh-negative group (n = 21) | P-value | |
|---|---|---|---|
| LVEF (%) | 34 ± 9 | 36 ± 8 | NS |
| LVEDVI (mL/m2) | 170 ± 67 | 180 ± 54 | NS |
| LVESVI (mL/m2) | 115 ± 57 | 117 ± 42 | NS |
| Segmental wall motion score | |||
| #1 | 2.2 ± 0.5 | 2.0 ± 0.5 | NS |
| #2 | 2.4 ± 0.5 | 2.3 ± 0.4 | NS |
| #3 | 2.3 ± 0.6 | 2.3 ± 0.4 | NS |
| #4 | 2.1 ± 0.6 | 2.2 ± 0.4 | NS |
| #5 | 2.1 ± 0.6 | 2.2 ± 0.5 | NS |
| #6 | 2.4 ± 0.5 | 2.2 ± 0.4 | NS |
| #7 | 1.9 ± 0.4 | 2.2 ± 0.6 | NS |
| Sum of #1–#7 | 15 ± 3 | 15 ± 2 | NS |
- a Left ventricular angiography (LVG) was not performed in four patients in the ACh-positive group and in one patient in the ACh-negative group so as not to aggravate renal dysfunction by overload of contrast agents. Thus, LVG was performed in 16 patients in the ACh-positive group and 21 patients in the ACh-negative group. Segmental wall motion was scored as follows: normokinesis, 1 point; hypokinesis, 2 points; akinesis, 3 points; dyskinesis or aneurysmal, 4 points.
- b ACh, acetylcholine; LVEDVI, left ventricular end-diastolic volume index; LVEF, left ventricular ejection fraction; LVESVI, left ventricular end-systolic volume index; NS, non-significant; sum of #1–#7, sum of each segmental wall motion score.
Findings on magnetic resonance imaging and left ventricular biopsy
In the present study, MRI and LV biopsy were performed only in those patients who understood the risks and signed the appropriate consent forms. Thus, of the 42 patients in the study, only 32 underwent MRI, and an LV biopsy was performed in 17. There was no bias or significant differences between the patients who underwent these examinations and those who did not.
Magnetic resonance imaging revealed delayed gadolinium enhancement in the mid-wall of the myocardium without subendocardial involvement less frequently in the ACh-positive group (2/17 patients; 12%) than in the ACh-negative group (11/15 patients; 73%; P < 0.01; Figure 2).
In the ACh-positive group, LV biopsy revealed no fibrous changes or evidence of degeneration compatible with idiopathic DCM (0/10 patients; 0%); however, in the ACh-negative group, five of seven patients (71%) exhibited these changes (P < 0.01; Figure 3).
Furthermore, there were no MRI findings indicative of myocarditis, such as oedematous changes of the myocardium, in any of the 32 patients examined, and there were no findings on LV biopsy of inflammatory cell infiltrate, interstitial oedema, or contract band necrosis in any of the 17 patients.
Changes in cardiac function following medical treatment
The efficacy of medical treatment in improving cardiac function was evaluated by using BNP and LVEF as indices of cardiac function. Angiotensin-converting enzyme inhibitors or angiotensin receptor blockers had been administered to 12 of 20 patients (60%) in the ACh-positive group and to 18 of 22 patients (82%) in the ACh-negative group. There were no significant differences in the rate of administration of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers between these two groups.
The types and doses of calcium channel blockers and beta-blockers administered to patients in the two groups are indicated in Table 4. There were no significant differences in the rate of baseline usage of beta-blockers (15% in the ACh-positive group vs. 14% in the ACh-negative group) and calcium channel blockers (10% vs. 27%) between these two groups. Furthermore, there were no significant differences in the rate of baseline usage of diuretics, spironolactone, and aspirin between the ACh-positive and ACh-negative groups (20% vs. 18%, 5% vs. 4%, and 5% vs. 9%, respectively; all P > 0.05). After the ACh provocation test, calcium channel blockers were administered more frequently to patients in the ACh-positive group than in the ACh-negative group (100% vs. 23%, respectively; P < 0.01). Fewer patients in the ACh-positive group were administered beta-blockers than in the ACh-negative group (55% vs. 95%, respectively; P < 0.01). In addition, there was no significant difference in the rate of administration of statins at baseline (5% in the ACh-positive group vs. 18% in the ACh-negative group) and after follow-up (30% vs. 18%) between these two groups. There was no significant difference in the duration of medical treatment between the ACh-positive and ACh-negative groups (range, 91–1144 days; median time, 406 days; mean ± SD, 399 ± 158 days vs. range, 162–880 days; median time, 337 days; mean ± SD, 384 ± 180 days, respectively; P > 0.05).
| ACh-positive group | ACh-negative group | |||
|---|---|---|---|---|
| No. of patients (%) | Mean (±SD) dose (mg) | No. of patients (%) | Mean (±SD) dose (mg) | |
| Beta-blockers | ||||
| Carvedilol | 3 (15) | 2.9 ± 1.9 | 14 (64) | 7.1 ± 6.4 |
| Bisoprolol | 8 (40) | 2.2 ± 0.6 | 7 (32) | 3.2 ± 1.2 |
| Not used | 9 (45) | – | 1 (4.5) | – |
| Calcium channel blockers | ||||
| Benidipine | 11 (55) | 7.4 ± 1.2 | 3 (14) | 4.7 ± 1.2 |
| Nifedipine | 1 (5) | 40 | – | – |
| Amlodipine | 1 (5) | 5 | 1 (4.5) | 2.5 |
| Azelnidipine | 1 (5) | 15 | 1 (4.5) | 16 |
| Diltiazem + nifedipine | 3 (15) | 200 + 20 | – | – |
| Benidipine + nisoldipine | 1 (5) | 6 + 10 | – | – |
| Benidipine + nifedipine | 2 (10) | 8 + 20 or 40 | – | – |
| Not used | 0 (0) | – | 17 (77) | – |
- a ACh, acetylcholine.
Four patients in the ACh-positive group and four patients in the ACh-negative group dropped out of the follow-up study during the observation period because of transition to other hospitals. Therefore, 16 patients in the ACh-positive group and 18 patients in the ACh-negative group were analysed. BNP was significantly reduced in both the ACh-positive group and the ACh-negative group even after 1 month of medical treatment, and this reduction was maintained for at least 1 year (ACh-positive group, 803 ± 482 vs. 104 ± 62 vs. 69 ± 84 pg/mL; ACh-negative, 688 ± 599 vs. 205 ± 197 vs. 143 ± 142 pg/mL; baseline vs. 1 month vs. 1 year, respectively; Figure 4A). There was no significant difference in the degree of improvement in BNP levels during the follow-up period between the two groups.
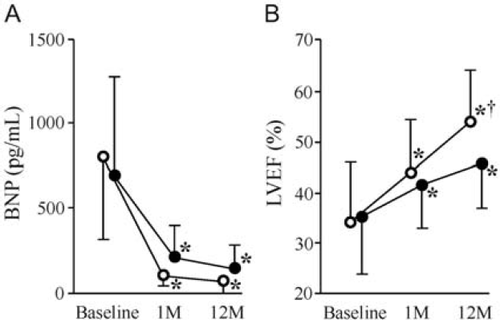
Baseline LVEF in all patients in the present study was 33 ± 11%. LVEF improved gradually both in the ACh-positive group and in the ACh-negative group (ACh-positive group, 34 ±12% vs. 44 ±11% vs. 54 ±11%; ACh-negative group, 35 ±11% vs. 41 ±9% vs. 46 ±9%; baseline vs. 1 month vs. 1 year, respectively; Figure 4B). There was no significant difference in the degree of improvement in LVEF during the follow-up period between the two groups.
Effects of medical treatment on electrocardiogram findings
At baseline, the ECG showed downward-sloping ST-T waves in leads I, aVL, V5, and V6. After 1 month of treatment, these downward-sloping ST-T waves were mildly improved, and downward-sloping ST-T waves or inverted T waves were newly recognized in leads II, aVF, V2, V3, and V4. After 1 year of treatment, all ECG findings were almost normalized, and the deep S waves in leads V2 and V3 and tall R waves in leads V5 and V6 had disappeared. Changes in ECG findings from baseline to 1 year are shown in Table 5. The time course of ischaemic changes seen on ECG were recognized more frequently in patients in the ACh-positive group than those in the ACh-negative group (85% vs. 14%, respectively; P < 0.01). The percentage of patients with a baseline ECG with some ischaemic findings which changed to a normalized ECG after 1 year was higher in the ACh-positive group than in the ACh-negative group (56% vs. 11%, respectively; P < 0.01).
| ACh-positive group, no. of patients (%) | ACh-negative group, no. of patients (%) | |||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | During hospitalization | After 1 month | After 1 year | Baseline | During hospitalization | After 1 month | After 1 year | |
| LBBB | 3 (15) | 3 (15) | 3 (15) | 2 (13) | 5 (23) | 5 (23) | 5 (23) | 5 (28) |
| STE | 3 (15) | 3 (15) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| STD | 6 (30) | 1 (5) | 7 (35) | 4 (25) | 8 (36) | 7 (32) | 8 (36) | 6 (33) |
| TWI | 0 (0) | 13 (65) | 2 (10) | 0 (0) | 0 (0) | 2 (9) | 0 (0) | 0 (0) |
| NSTC | 8 (40) | 0 (0) | 2 (10) | 1 (6) | 4 (18) | 4 (18) | 3 (14) | 2 (11) |
| Normal | 0 (0) | 0 (0) | 6 (30) | 9 (56) | 5 (23) | 4 (18) | 6 (27) | 5 (28) |
- a ACh, acetylcholine; LBBB, left bundle branch block; NSTC, non-specific ST-T change; STD, ST depression; STE, ST elevation; TWI, T wave inversion.
Discussion
The present study demonstrates that: (i) there are certain patients with idiopathic DCM-like LV dysfunction due to coronary multispasm; (ii) the MRI and LV biopsy findings in these patients are not compatible with idiopathic DCM; and (iii) the LV function in these patients improves significantly following the administration of calcium channel blockers.
In coronary spasm, sudden excessive coronary vasoconstriction produces a transient reduction in blood flow, resulting in myocardial ischaemia.1,2 ACh dilates blood vessels when the vascular endothelium is normal but, if there is endothelial detachment or injury, ACh contracts blood vessels.22,23 Thus, the ACh provocation test documents coronary spasm in patients with coronary spastic angina with high sensitivity and specificity.24,25 In the present study, the ACh provocation test revealed coronary spasm in 48% of patients who had idiopathic DCM-like LV dysfunction without significant coronary stenosis. Patients in the ACh-positive group were more likely to exhibit ischaemic changes on the ECG and were less likely to have myocardial fibrosis or degeneration on cardiac MRI or biopsy than patients in the ACh-negative group. Furthermore, patients in the ACh-positive group were more likely to have coronary risk factors such as hypertension and a history of smoking. These findings suggest that the main cause of LV dysfunction in the ACh-positive group was myocardial ischaemia due to coronary multispasm. Conventionally, many of the patients with diffuse LV dysfunction but without significant coronary stenosis and specific myocardial diseases (e.g. hypertrophic cardiomyopathy, cardiac amyloidosis, cardiac sarcoidosis, etc.) have been diagnosed as having idiopathic DCM.26 It has been thought unlikely that coronary spasm causes chronic LV dysfunction, because coronary spasm is commonly thought to be transient. In fact, many of the patients in the ACh-positive group in the present study had not experienced typical angina chest pain prior to their admission to hospital and they did not have typical chest pain even during the ACh provocation test. This suggests that coronary spasm related to LV dysfunction is an almost silent ischaemia, and so coronary spasm has been overlooked as an aetiology of LV dysfunction. In patients with coronary spastic angina, it has been demonstrated that chest pain is recognized in only ∼30% of the patients with episodes of ischaemic ST change on ECG, and many events of coronary spasm are asymptomatic.27 Patients with myocardial hibernation or myocardial stunning have not always described their chest pain.28 These findings raise the possibility that patients with myocardial hibernation or stunning due to chronic or repeated coronary spasm find it hard to describe chest pain, which is consistent with the high incidence of patients without chest pain in the ACh-positive group in our study. In recent years, a correlation between coronary spasm and idiopathic DCM has been reported in small studies, in which approximately one-third of idiopathic DCM patients were found to have coronary spasms.8,9 Furthermore, according to a report published in 2009, multiple coronary spasm may be the cause of transient heart failure in a small percentage of patients with heart failure of unknown origin.10 The results of the present study suggest that diffuse spasm in multiple coronary vessels is one of the mechanisms leading to idiopathic DCM-like LV dysfunction. Therefore, our findings may raise the possibility that patients with congestive heart failure or LV dysfunction due to chronic or repeated coronary spasm are not being identified as a separate group and, instead, are being diagnosed conventionally as having idiopathic DCM.
In the present study, all the patients in the ACh-positive group were treated with calcium channel blockers. Meanwhile, in the ACh-negative group, 95% of patients were treated with beta-blockers. LVEF and BNP improved significantly in both groups, and there was no significant difference in the degree of improvement in LVEF or BNP during the follow-up period between the two groups. Furthermore, LV dilatation and depressed LV systolic function, as shown on echocardiography, were markedly improved, and the ischaemic changes and findings of LV overload on the ECG were improved and almost normalized following calcium channel blocker treatment in patients in the ACh-positive group. These findings suggest that the calcium channel blockers played an important role in the improvement of LV dysfunction in the ACh-positive group, and that functional recovery in the ACh-positive group treated with calcium channel blockers was comparable with that in the ACh-negative group treated with beta-blockers. Calcium channel blockers counteract the action of coronary spasm,29–31 and this may be the mechanism underlying the improvements in LV dysfunction in the ACh-positive group. It is well known that beta-blockers are effective in improving LV dysfunction in conditions such as idiopathic DCM.11,12 However, calcium channel blockers are not included in the guidelines for the treatment of this sort of LV dysfunction.26,32,33 The findings of the present study suggest that the existence of coronary spasm should be considered when diagnoses of idiopathic DCM-like LV dysfunction are being made and that treatment with calcium channel blockers may be appropriate if the LV dysfunction is found to be related to coronary spasm. Thus, current guidelines for the treatment of LV dysfunction may have to be reconsidered to take into account the possible role of calcium channel blockers.
Finally, our results suggest that non-invasive examinations, such as ECG and MRI, are effective in the assessment of the possible involvement of multiple vessel coronary artery spasm in the aetiology of idiopathic DCM-like LV dysfunction, and that invasive coronary angiography, including the ACh provocation test, and treatment with calcium channel blockers may need to be considered if the results of the non-invasive examinations strongly indicate the possibility of multiple vessel coronary artery spasm.
Limitations
There are limitations to the present study. First, the observation period was relatively short and, secondly, the study was performed in a small number of subjects. A study with a longer observation period and performed in a larger number of patients is needed to confirm the findings of the present study and to ensure their accuracy. Thirdly, the positive rate of the ACh test in this study was relatively high (∼48%), and it has been demonstrated that the incidence of spasm in Japanese patients with recent myocardial infarction was also high (∼60%).7 These findings can be related to the high incidence of Japanese patients who have spasm. Thus, it may raise the possibility that the positive rate of the ACh test in Caucasian patients with idiopathic DCM-like LV dysfunction is different from that of Japanese patients. Fourthly, the MRI study and myocardial biopsy were not performed in all of the study patients. To this end, this study was not randomized, and the results of this study have not proved that a similar improvement could not be achieved with conventional treatment including beta-blockers. Therefore, a randomized controlled trial using calcium channel blockers is necessary to re-evaluate the optimum treatment of LV dysfunction.
Conclusion
In conclusion, a subgroup of patients who have been diagnosed as having idiopathic DCM may, indeed, have LV dysfunction due to coronary multispasm. Based on the results of the present study, the use of calcium channel blockers appears to be a good therapeutic strategy in these patients.
Conflict of interest: none declared.




