Meta-analysis of randomized controlled trials evaluating left ventricular vs. biventricular pacing in heart failure: effect on all-cause mortality and hospitalizations
Abstract
Aim
Randomized controlled trials (RCTs) showed that biventricular (BiV) pacing reduces heart failure (HF) hospitalizations and mortality in patients with New York Heart Association (NYHA) class III–IV HF, left ventricular (LV) dysfunction, and wide QRS. We performed a systematic review and meta-analysis of the RCTs comparing LV-only vs. biventricular (BiV) pacing in candidates for cardiac resynchronization therapy (CRT).
Methods and results
The systematic review selected five RCTs (out of 1888 analysed reports) with a cumulative number of 372 patients randomized to BiV pacing and 258 to LV-only pacing. The meta-analysis shows that BiV pacing is not superior to LV-only pacing and that these two pacing modalities do not differ with regard to death or heart transplantation [LV-only vs. BiV pacing odds ratio (OR) 1.24, 95% confidence interval (CI) 0.57–2.70 with the fixed effect model, OR 1.25, 95% CI 0.48–3.24 with the random effect model]. Specific data on hospitalizations were available only in two RCTs with a cumulative number of 127 patients randomized to BiV and 123 to LV-only pacing. The meta-analysis shows that BiV pacing is not superior to LV-only pacing and that these two pacing modalities do not differ with regard to this outcome (LV-only vs. BiV pacing OR 0.86, 95% CI 0.49–1.50 with the fixed effect model, OR 0.86, 95% CI 0.49–1.50 with the random effect model).
Conclusions
Biventricular pacing is not superior to LV-only pacing, and these two pacing modalities appear to achieve similar efficacy in candidates for CRT for moderate to severe HF, in terms of all-cause mortality and hospitalizations during follow-up.
Introduction
A series of randomized controlled trials (RCTs) showed that biventricular (BiV) pacing improves clinical outcomes and reduces heart failure (HF) hospitalizations and mortality in symptomatic patients with chronic HF and New York Heart Association (NYHA) class III–IV despite optimal medical therapy, left ventricular ejection fraction (LVEF) ≤35%, and QRS ≥120 ms. The results of these studies were analysed in a meta-analysis of RCTs, published by McAlister et al. in 2007, where cardiac resynchronization therapy (CRT) with BiV pacing decreased hospitalizations by 37% and mortality by 22% vs. controls.1
The mechanism by which BiV pacing improves systolic function, symptoms, and outcome are complex, but generally they are mainly related to correction of electrical/mechanical dyssynchrony. For this reason the electrical therapy for treating selected patients with HF has been named CRT. The possibility of obtaining haemodynamic and clinical benefits in HF patients with left bundle branch block by left ventricular (LV)-only pacing has been tested since the initial pioneering phase of research on CRT.2–4 A series of observational studies and a few randomized studies aimed to compare the efficacy of BiV stimulation and LV-only stimulation in patients with moderate to severe HF.
A very recent meta-analysis compared BiV vs. LV-only pacing considering a series of functional cardiac endpoints (exercise capacity, peak oxygen consumption, quality of life, NYHA class, LVEF, and remodelling), but did not provide a comparison on hard endpoints, such as mortality and hospitalizations.5
The aim of the present study is to provide a meta-analysis of the RCTs, comparing BiV vs. LV-only pacing in patients with moderate to severe HF with LV dysfunction and a wide QRS complex, and considering the effect of these two pacing modalities on patient outcomes (mortality or heart transplantation, hospitalizations).
Methods
Evidence acquisition: search strategy and study selection
We analysed studies that involved human subjects. We systematically searched MEDLINE, the Cochrane Central Register of Controlled Trials, and the National Library of Medicine Gateway. The search terms included ‘biventricular pacing AND left ventricular pacing’. We considered studies published between 1994 and July 2011.
We selected studies according to the following criteria: participants followed for at least 1 month after implant, patients with HF in NYHA functional class III or IV despite optical medical therapy, and patients in sinus rhythm with an approved indication for implantation of a CRT device. We excluded studies that considered patients with atrial fibrillation. We included in this meta-analysis RCTs that reported outcome data on mortality for patients who received CRT delivered through BiV stimulation vs. patients with LV-only stimulation, with data available for the first period after randomization (in order to avoid a carryover effect we excluded studies where data on outcome were not limited to the first randomization phase but included also phases of crossover to the alternative pacing mode).
Literature search and results
Medline
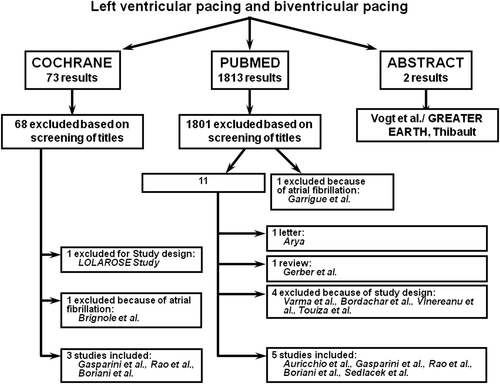
From 1813 citations, we identified 12 studies based on screening of the title. One of these was excluded because it considered patients with atrial fibrillation; three citations were excluded because they concerned acute studies. We then excluded a review and a letter between authors. The final list of studies includes five trials: Auricchio et al.,6 Gasparini et al.,7 Rao et al.,8 Boriani et al.,9 and Sedláček et al.10
Cochrane
From 73 citations, we identified five studies based on screening of the title. We excluded one of these because of the study structure and another one because it dealt with patients with atrial fibrillation. We thus selected a remaining group of three trials: Gasparini et al.,7 Rao et al.,8 and Boriani et al.9
The flow chart of the search strategy and selection of the trials is shown in Figure 1.
We included the randomized study reported by Auricchio et al.,6 where patients with NYHA III–IV HF, implanted with an epicardial lead for LV pacing, were randomized to BiV pacing or to univentricular pacing, the latter selected on the basis of an acute haemodynamic study resulting in selection of LV-only pacing in 90% of cases and right ventricular pacing in 10% of cases. This randomized study included a first phase of 4 weeks followed by a crossover. For the present meta-analysis, only data on assessment of outcome (mortality) at 1 month (before crossover) were considered, in order to avoid a carryover effect.
The study by Rao et al.8 randomized patients to three arms, i.e. LV-only pacing, BiV pacing with simultaneous right and left ventricular pacing, and BiV pacing with sequential BiV pacing. In view of the aims of this systematic review and meta-analysis, the arm randomized to LV-only pacing was compared with the other two arms.
The study by Thibault et al. (GREATER-EARTH) was a randomized double-blind, crossover trial comparing LV-only with BIV pacing, where, after a run-in period of 2–8 weeks, patients were randomized to LV-only pacing followed by crossover to BiV pacing or vice versa, for consecutive 6 month periods.11 The final report, recently published, did not include data on mortality and hospitalization for the first randomized phase, but only for the whole study period.12 Since our aim, similarly to what was done in evaluating the previous study by Auricchio et al.,6 was to consider only the first randomized phase before crossover, in order to exclude a carryover effect, this study was not included in our meta-analysis.
Data extraction and analysis
The meta-analysis was performed with both the inverse variance method (fixed effect) and the DerSimonian–Laird method (random effect). The assessment of publication bias was carried out by funnel plot and by Begg's test. To investigate the influence of each individual study on the overall meta-analysis summary, we used Metaninf. Statistical heterogeneity was quantified using the I2 statistic. All results are reported with 95% confidence intervals (CI).
Results
The main characteristics of the five RCTs we considered for this meta-analysis on survival and the characteristics of the patients enrolled in these studies are shown in Table 1. All these studies enrolled only patients in NYHA class III–IV, except the study by Gasparini et al.,8 which included NYHA class II patients (38% of enrolled patients). All these studies were funded by the industry, except that by Sedláček et al.10
| Author (year) | Blinding | Design | Study group (no. of patients) | Age | Ischaemic aetiology [no. of patients (%)] | NYHA III (%) or mean NYHA class | QRS (ms) | LVEF (%) |
|---|---|---|---|---|---|---|---|---|
| Auricchio et al. (2002)6 | Single blind | Random, crossover | All (42) | 60 ± 7 | 12 (29) | 36 (86) | 175 ± 32 | 21 ± 7 |
| BiV (24) | 59 ± 7 | 10 (42) | 21 (88) | 174 ± 30 | 21 ± 6 | |||
| LV (17) | 60 ± 5 | 1 (6) | 14 (82) | 178 ± 34 | 20 ± 7 | |||
| Gasparini et al. (2006)7 | Single blind | Random, parallel | All (69)a | 66.7 (7.4) | 44 (63.8) | 43 (62.3) | 172 (28) | 25.2 (6.2) |
| BiV (33)a | 66.9 (7.6) | 19 (57.6) | 19 (57.6) | 176 (25) | 25.8 (6.2) | |||
| LV (36)a | 66.5 (7.3) | 25 (69.4) | 24 (66.7) | 169 (31) | 24.6 (6.2) | |||
| Rao et al. (2007)8 | Double blind | Random, parallel | LV (101) | 67.4 ± 9.6 | 67 (66) | 98 (97) | 165 ± 15 | 22.6 ± 6.6 |
| Sequential BiV (104) | 66.6 ± 10.5 | 70 (67) | 100 (96) | 167 ± 16 | 22.4 ± 6.7 | |||
| Simultaneous BiV (101) | 66.2 ± 10.6 | 58 (57) | 101 (100) | 168 ± 15 | 23.2 ± 7.1 | |||
| Boriani et al. (2010)9 | Double blind | Random, parallel | All (176) | 66 ± 9 | 92 (52) | 165 (94) | 161 ± 20 | 25 ± 6 |
| BiV (90) | 66 ±10 | 48 (53) | 84 (93) | 160 ± 19 | 26 ± 6 | |||
| LV (86) | 66 ± 9 | 44 (51) | 81 (94) | 162 ± 20 | 25 ± 6 | |||
| Sedláček et al. (2010)10 | Double blind | Random, parallel | BiV (16) | 59.56 ± 6.83 | NA | Mean 3.13 ± 0.39 | 187 ± 25 | 20.7 ± 0.8 |
| LV (17) | 62.05 ± 12.13 | NA | Mean 3.21 ± 0.36 | 195 ± 9 | 21.3 ± 1.0 |
- a Data are shown as the mean ± standard deviation or as median (interquartile range).
- b BiV, biventricular; LV, left ventricular; LVEF, left ventricular ejection fraction; NA, not available; NYHA, New York Heart Association.
- a Data on randomized patients excluding crossover, dropouts, and deaths.
As shown in Table 2, these studies differed either with regard to the primary and secondary endpoints taken into account or with regard to length of follow-up. As shown, the cumulative number of randomized patients was 372 for BiV pacing and 258 for LV-only pacing.
| Author, year | Primary endpoint | Other endpoints | FU (months) | Eligible patients | Excluded patients | Patients randomized to BiV | Patients randomized to LV | Patients withdrawn from BiV | Patients withdrawn from LV |
|---|---|---|---|---|---|---|---|---|---|
| Auricchio et al. (2002)6 | Peak VO2; 6MWT | NYHA; QOL | 1 | 42 | 1 | 24 | 17 | 0 | 0 |
| Gasparini et al. (2006)7 | LVEF; 6MWT | Arrhythmic events; mortality; hospitalizations | 12 | 102 | 28 | 37 | 37 | 4 | 1 |
| Rao et al. (2007)8 | Peak VO2; end-diastolic LV volume | End-systolic LV volume; mitral regurgitation | 6 | 360 | 54 | 205 | 101 | 9 patients overall (BiV or LV) | |
| Boriani et al. (2010)9 | NYHA; end-diastolic LV volume | LVEF; 6MWT; QOL | 6 | 186 | 10 | 90 | 86 | 1 | 1 |
| Sedláček et al. (2010)10 | NYHA, QOL | LVEF; end-systolic LV volume; mitral regurgitation; 6MWT; peak VO2 | 12 | 40 | 7 | 16 | 17 | 0 | 0 |
- a Data are shown as mean ± standard deviation or as median (interquartile range).
- b BiV, biventricular; FU, follow up; LV, left ventricular; LVEF, left ventricular ejection fraction; 6MWT, 6 min walking test; NYHA, New York Association functional class; QOL. quality of life.
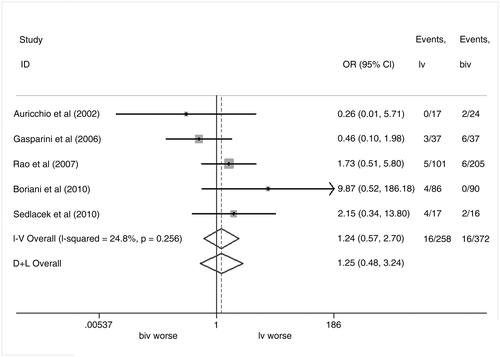
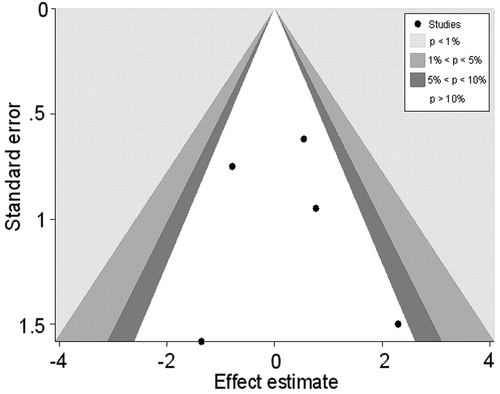
Data on patient outcomes in terms of death or heart transplantation are summarized in Table 3. The results of the meta-analysis on the effect of BiV vs. LV-only pacing in terms of death or heart transplantation are shown in Figure 2. The forest plot (fixed effect, as well as random effect model methods) shows that BiV pacing is not superior to LV-only pacing and that these two pacing modalities do not differ with regard to this outcome [LV-only vs. BiV pacing odds ratio (OR) 1.24, 95% CI 0.57–2.70 with the fixed effect model, OR 1.25, 95% CI 0.48–3.24 with the random effect model]. No statistically significant heterogeneity was observed [test for heterogeneity χ2 =5.32 (df = 4), P = 0.256; I2 = 24.8%; test for overall effect z = 0.54, P = 0.589]. Analysis of the funnel plot showed no publication bias (Figure 3).
| Author, year | Patients randomized to BiV | Patients randomized to LV-only | ||
|---|---|---|---|---|
| Alive/death or heart transplantation | Not hospitalized/hospitalized | Alive/death or heart transplantation | Not hospitalized/hospitalized | |
| Auricchio et al. (2002)6 | 22/2 | NA | 17/0 | NA |
| Gasparini et al. (2006)7 | 31/6 | 26/11 | 34/3 | 28/9 |
| Rao et al. (2007)8 | 199/6 | NA | 96/5 | NA |
| Boriani et al. (2010)9 | 90/0 | 24/66 | 82/4 | 66/20 |
| Sedláček et al. (2010)10 | 14/2 | NA | 13/4 | NA. |
- a BiV, biventricular, LV, left ventricular.
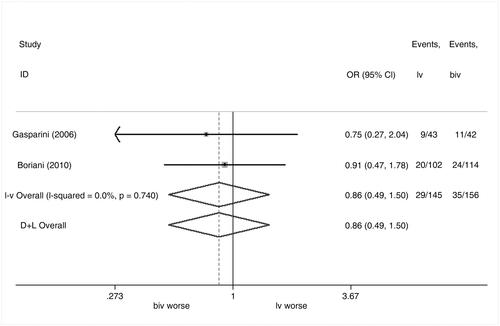
Specific data on hospitalizations following randomization to BiV or LV-only pacing were available only in the RCTs reported by Gasparini et al.7 and by Boriani et al.9 (Table 3). In detail, in the study reported by Gasparini et al.,7 11 out of 37 patients randomized to BiV pacing and 9 out of 37 patients randomized to LV-only pacing were hospitalized. In the RCT by Boriani et al.,9 24 out of 90 patients randomized to BiV pacing and 20 out of 86 patients randomized to LV-only pacing were hospitalized.
The results of the meta-analysis on the effect of BiV vs. LV-only pacing in terms of hospitalizations are shown in Figure 4. The forest plot shows that BiV pacing is not superior to LV-only pacing and that these two pacing modalities do not differ with regard to this outcome (LV-only vs. BiV pacing OR 0.86, 95% CI 0.49–1.50 with the fixed effect model, OR 0.86, 95% CI 0.49–1.50 with the random effect model). No statistically significant heterogeneity was observed [test for heterogeneity χ2 0.11 (df = 1), P = 0.740; I2 = 0.0%; test for overall effect z = 0.53, P = 0.593].
Discussion
The present article is the first systematic review and meta-analysis focused on the comparison between two alternatives pacing modalities for CRT, BiV and LV-only pacing, performed to estimate the effect of these two pacing modalities on hard patient outcomes (all-cause mortality or heart transplantations and hospitalizations). CRT can in fact be achieved through BiV pacing, through LV-only pacing, or through triple-site pacing,13,14 although no studies on hard endpoints are available with regard to the last option.
The results of this meta-analysis show that BiV pacing is not superior to LV-only pacing and that these two pacing modalities do not appear to differ with regard to mortality and hospitalizations during post-implant follow-up. Data on survival after CRT were reported in all of the five RCTs we selected, and no significant heterogeneity of the effect emerged in the meta-analysis. This results is noteworthy since the positive effect of BiV pacing on the mortality of HF patients was a crucial step in the validation, acceptance, and coverage of CRT.1
Several thousand patients were enrolled in RCTs focused on assessing the efficacy of BiV pacing vs. control treatment in patients with moderate to severe HF (NYHA III–IV)1 and more recently in patients with mild heart failure (NYHA I–II).15 In contrast, only ~630 patients were enrolled in RCTs comparing the efficacy of BiV with LV-only pacing in moderate to severe HF. These studies have important differences regarding the primary endpoint (usually an echocardiographic measure of ventricular function). None of the studies comparing BiV with LV-only pacing included all-cause mortality or hospitalizations as primary endpoints. As already stressed, a single RCT powered to compare these two pacing modalities is hard to plan and will encounter difficulties in obtaining financial support.7 We can reasonably estimate that an RCT specifically designed to test the non-inferiority of LV pacing compared with BiV pacing in terms of all-cause mortality in a 1-year follow-up (with a 15% expected mortality in BiV-treated patients) would require an overall population of 316 patients (randomized 1:1 to each of the two pacing modes) by assuming a non-inferiority margin of 10%, while the overall sample size would increase to 1262 cases by assuming a non-inferiority margin of 5%.
The limited number of events found in published RCTs comparing LV-only with BiV pacing strongly supports the approach of a meta-analysis to estimate the comparative impact of these two pacing modalities in terms of clinical outcomes. In the present systematic review and meta-analysis we specifically derived data on all-cause mortality (and heart transplantation) and hospitalizations, respectively, from available trials, and a meta-analysis was performed on these two endpoints.
Interpretation of our meta-analysis on hospitalizations requires some caution, in view of the limitations of available data. In fact, the number of hospitalization after CRT device implantation was not reported by any of the trials, and no specific information on the causes of hospitalizations was available in most of the selected RCTs.
Other outcomes concerning quality of life and echocardiographic parameters were variably reported by the authors and were not the subject of this meta-analysis, since they had already been evaluated in a recent meta-analysis by Liang et al.5 These authors performed a meta-analysis on five trials considering a series of analysed outcomes including clinical status (6 min walk distance, peak oxygen consumption, quality of life, NYHA class), LV function (LVEF), and LV remodelling (LV end-systolic volume). The results showed that LV-only pacing achieved similar improvements in clinical status to BiV pacing, with a trend toward superiority of BiV vs. LV-only pacing for LV reverse modelling and systolic function, although without reaching statistical significance.
The present meta-analysis supports the potential clinical value of LV-only pacing in candidates for CRT and may be of interest for a series of reasons. First, LV-only pacing may be one of the potential modalities in which a triple-chamber dedicated device, with (CRT-D) or without defibrillation capabilities (CRT-P), can be programmed, with the inherent advantage of saving battery consumption and extending device longevity. The extension of device longevity may be predicted in the range of 20% of device longevity9 and may be of financial and clinical importance, since device replacement is a costly procedure and is associated with complications, such as infections.16 Another reason in favour of LV-only pacing regards specific categories of patients (elderly patients with indication for CRT and frequent hospitalizations for HF, not requiring implantable cardioverter defribrillator back up) in whom atrial-synchronous LV-only pacing can be achieved with very simple and cheap solutions (i.e. a coronary sinus lead connected to a conventional DDD device). The latter technique, already used in practice,5 also with Autocapture,17,18 requires phrenic nerve stimulation at or near the output delivered in order for LV capture to be ruled out.19 As a matter of fact, the algorithms for managing phrenic nerve stimulation, based on change of the stimulation vectors,19 are not available in conventional DDD pacemakers. CRT-D through BiV is not uniformly implemented in clinical practice, and in Europe a wide variability in CRT implants have been reported.20 Since CRT-D devices are costly and implementation of CRT-D may be limited by financial contrasts, the possibility of adopting a cheaper pacing modality in some patients should be taken into consideration.21,22
The results of our meta-analysis on survival are limited by the relatively low number of patients enrolled in the selected RCTs. A recently published randomized study, GREATER-EARTH,11,12 was not included in the present meta-analysis because data on mortality and on hospitalization were not reported separately for every specific pacing mode (LV-only or BiV). for the first randomization period and for the phase after crossover. Despite this limitation, it is noteworthy that both all-cause mortality and hospitalization for HF were quite similar during LV-only and BiV pacing programming. For the evaluation of LV-only vs. BiV pacing it may be of interest to consider data on effectiveness reported by observational studies. Two comparative observational studies have been reported by Touiza et al.,23 and, as an abstract, by Vogt et al.,24 and may offer additional information on the outcome of the pacing modalities in the long term, despite the bias of their observational nature.
Touiza et al.22 and Vogt et al.24 reported comparative data on the outcome of patients implanted with a device delivering BiV pacing (15 and 299 patients, respectively) or LV-only pacing (18 and 100 patients, respectively), followed for 6 and 25 months, respectively. It is of interest to note that the proportion of patients who died or underwent heart transplantation was quite similar between the two pacing modalities, in line with our meta-analysis. In detail, death or heart transplantation was cumulatively observed in 53 out of 314 patients (16.8%) treated with BiV pacing and in 18 out of 118 patients (15.2%) treated with LV-only pacing. Although the application of formal meta-analytical methods to observational studies has been controversial, the number of published meta-analyses concerning observational studies has increased substantially.25 With all the limitations of such an approach, addition of the observational studies by Touiza et al.23 and Vogt et al.24 to the studies we selected (reaching an overall population of 376 patients treated with LV-only pacing and 686 patients treated with BiV pacing) results in the same conclusions as our previous meta-analysis. In detail, the two pacing modalities do not differ with regard to death or heart transplantation (LV-only vs. BiV pacing OR 0.98, 95% CI 0.61–1.57 with the fixed effect model, OR 0.98, 95% CI 0.61–1.59 with the random effect model) and no statistically significant heterogeneity was observed [test for heterogeneity χ2 =6.03 (df = 6), P = 0.419; I2 = 0.6%; test for overall effect z = 0.10, P = 0.920].
Conclusions
In summary, a meta-analysis of five RCTs, related to the comparison between CRT through conventional BiV pacing or LV-only pacing, shows that BiV pacing is not superior to LV-only pacing and that these two pacing modalities appear to achieve a similar efficacy in candidates for CRT for moderate to severe HF, in terms of all-cause mortality and hospitalizations during post-implant follow-up.
In view of these results LV-only pacing may be considered as an additional possibility for improving the outcome of HF patients who are candidates for CRT, with effects similar to conventional BiV pacing. This possibility, also achievable with rather simple pacing systems, may be attractive in an era of economic constraints, specifically in geographic areas where CRT-D is not adopted for financial reasons.20,21 This additional option deserves consideration in light of the trend for increasing implant rates across Europe26 and should be mentioned by consensus guidelines.27
Conflict of interest: L.P. has received research grants from Medtronic, Boston Scientific, St. Jude, and Sorin SpA. All other authors have no conflicts to declare.