The impact of a self-management group programme on health behaviour and healthcare utilization among congestive heart failure patients
Abstract
Aims
The ‘Chronic Disease Self-Management Programme’ (CDSMP) emphasizes patients’ responsibility for the day-to-day management of their condition(s) and has shown favourable effects on health behaviour and healthcare utilization among various groups of patients with chronic conditions. However, the effects of the CDSMP among congestive heart failure (CHF) patients are unknown. We therefore aimed to assess the effects of the CDSMP on health behaviour and healthcare utilization in patients with CHF.
Methods and results
This randomized, controlled trial with 12 months of follow-up included 317 CHF patients with a slight to marked limitation of physical activity. Control patients (n = 131) received usual care, consisting of regular checkups at an outpatient clinic. Intervention group patients (n = 186) received usual care and participated in a 6-week self-management group programme. Favourable effects on walking for exercise and other physical activities such as aerobic, stretching, and strength exercises, sports, and gardening were reported in the intervention group immediately after completion of the programme. The effect of the programme on other physical activities extended to 6 months of follow-up. No favourable effects were found for the other outcomes.
Conclusion
The CDSMP significantly improved physical activity among CHF patients for up to 6 months after the end of the programme; however, it did not affect other health behaviour outcomes or healthcare utilization.
Introduction
Congestive heart failure (CHF) is a major public health concern, due to ageing of the population the prevalence and incidence of CHF is likely to increase dramatically over the coming years, imposing an enormous burden on society in terms of mortality, morbidity, and associated healthcare costs.1 Efficient management of CHF therefore remains a challenge for both patients and healthcare providers. Congestive heart failure patients face severe symptoms such as fatigue, shortness of breath, and exercise intolerance due to cardiac dysfunction. This substantially affects their physical functioning, quality of life, and mortality rates.2,3 Furthermore, patients need to make considerable adjustments to their life style to prevent CHF exacerbations by, for example, adhering to a dietary sodium and fluid restriction, taking prescribed medications, and staying physically active. For this reason, patients are encouraged to take responsibility for the day-to-day management of their disease as patients’ own self-care abilities are crucial in CHF management.4,5 Unfortunately, many patients fail to adhere to the complex treatment regimen. A downward spiral of functional deterioration and non-compliance may then lead to increased healthcare utilization and a progressive decline in the condition of the patient.5–8
The ‘Chronic Disease Self-Management Programme’ (CDSMP) is a generic cognitive-behavioural group programme, which deals with medical, social, and emotional management of a chronic condition.9 An important assumption of the programme is that patients can learn to take responsibility for the day-to-day management of their disease(s),9,10 which seems crucial for CHF patients. The programme aims to teach patients how to deal with the medical consequences of their disease, to remain socially active in daily life, and to deal with the emotional consequences of being chronically ill.9 The CDSMP is based on Bandura's self-efficacy theory.11 Self-efficacy refers to the belief that one is capable of performing intended behaviours successfully and is considered a powerful determinant of behavioural change.11,12 In his theory, Bandura11 recognizes four different sources of self-efficacy: enactive mastery experiences that serve as indicators of people's capability; vicarious experiences that alter efficacy beliefs through comparison with others; social persuasion to strengthen people's beliefs; and physiological and affective states from which people may judge their capabilities. Enhancing self-efficacy expectancies among CHF patients may be very important, as there are indications that low levels of self-efficacy predict functional decline.13
Since the 1990s, the CDSMP has been widely disseminated and evaluated within and outside the USA, both in mixed and homogeneous patient groups.10,14–31 However, the effectiveness of the programme on health behaviour and particularly on healthcare utilization is inconclusive, since some studies showed favourable results,10,14 whereas others reported limited15–20 or no substantial evidence21–25 of effectiveness. These inconclusive findings on health behaviour and healthcare utilization cannot be ascribed to differences in measurement instruments, since all studies used measures comparable to those used by Lorig et al.10 Other evaluation studies, however, did not assess healthcare utilization and/or health behaviour at all.26–31 Furthermore, the effect of the programme on health behaviour and healthcare utilization among CHF patients, in particular, has not yet been assessed. We therefore conducted a randomized, controlled trial to assess the effects of the CDSMP on health behaviour and healthcare utilization in CHF patients with a slight to marked limitation of physical activity.
Methods
Study design
Effectiveness of the CDSMP was assessed in a two-group randomized controlled trial with 12 months of follow-up. CHF outpatients were recruited from six hospitals in the Netherlands. Data on health behaviour and healthcare utilization were collected by means of telephone interviews at baseline, directly after the end of the programme, and 6 and 12 months after the start of the programme. The telephone interviews were independently conducted by trained interviewers blinded to group allocation. Twenty-one CDSMP classes were conducted between October 2004 and January 2006 in 11 consecutive cycles, with at least one class and a parallel control group in each cycle. Per cycle and hospital, patients were randomly allocated to the intervention or control group by means of a computerized allocation procedure after completion of the baseline measurement. The randomization procedure was performed by an independent researcher using SPSS 12.0 for Windows. Control patients received usual care, consisting of regular checkups with the cardiologist and/or the CHF nurse specialist at an outpatient clinic. Patients allocated to the intervention group received the self-management group programme in addition to usual care. In each cycle, in which one or more CDSMP classes were planned, the time to recruit patients for the study was limited. As a consequence, equally large, parallel, control groups could not be created, as at least eight patients per cycle were allocated to the intervention group, for reasons of group dynamics. As the group process is very important in the CDSMP,32 at least eight participants are required to participate in the classes, according to Lorig et al.15 Therefore, based on the total number of recruited patients per cycle, 59% of the patients were allocated to the intervention group and 41% to the control group through the full recruitment period to ensure sufficiently large CDSMP classes.33
Based on the sample size calculation, 360 patients needed to be included in the study. The sample size calculation was based on figures on self-efficacy expectancies12 (one of the primary outcome variables in the study protocol34) as derived from a Dutch study among newly diagnosed older CHF patients.13 To detect a mean difference of at least 4.0 points on self-efficacy expectancies between the two study groups (SD = 11.8; equivalent to an effect size of 0.34), a net number of 274 patients needed to be available for longitudinal analyses to achieve a power of 80% at an alpha of 0.05. Approximately 360 patients needed to be included in the study as we assumed a drop-out rate of 25% during the trial. The trial conformed to the principles outlined in the Declaration of Helsinki35 and was approved by the Medical Ethics Committee of Maastricht University/University Hospital Maastricht.34
Participants
Congestive heart failure outpatients received written information about the study if they (i) had been diagnosed with CHF based on systolic dysfunction (left ventricular ejection fraction (LVEF) <40%, NYHA Classes II and III) or diastolic dysfunction (NYHA Classes II and III), as diagnosed by the patients' primary cardiologist according to the CHF guidelines.36 Patients with diastolic dysfunction were eligible after being admitted at least once in the hospital based on cardiac decompensation after CHF diagnosis. In addition, patients were eligible if they: (ii) had been a CHF patient for at least 6 months at the start of the intervention period, which was considered an appropriate time interval for the CHF diagnosis and therapeutic decisions to have been made; (iii) were able to understand, write, and speak Dutch; and (iv) were willing to give informed consent to participate in the study. Patients were excluded if they were participating in other studies. Eligible patients underwent a baseline measurement after signing the informed consent form and before randomization.
Intervention
The CDSMP is a structured self-management programme and consists of six weekly group sessions of two and a half hours each. The programme incorporates skills mastery, reinterpretation of symptoms, modelling, and social persuasion to enhance self-efficacy expectancies.9,32 Skills mastery includes goal-setting and action-planning and takes up about 25–35% of each session. Patients are supported in action-planning through telephone calls with co-participants. Furthermore, patients are encouraged to set an exercise goal and to make a personal exercise plan during the programme. Reinterpreting symptoms helps to relieve symptom problems such as shortness of breath by, for example, breathing exercises and relaxation techniques. Through action-planning and reinterpreting symptoms, the intervention takes into account patients’ individual beliefs and cognitions about their illness. Finally, by modelling and social persuasion, participants are expected to become motivated to change their behaviours and beliefs.9
At the start of the programme, patients received the CDSMP reference book Living a healthy life with chronic conditions.37 The CDSMP classes were led by a cardiac nurse specialist (‘professional leader’) and a CHF patient (‘peer leader’). Cardiac nurse specialists (n = 9) participated in the programme to decrease the potential burden on the peer leaders (n = 9), to ensure continuity of the programme, and to facilitate implementation of the programme in regular Dutch healthcare. The CDSMP classes were held between October 2004 and January 2006 alongside usual work at the hospital. The peer leaders acted as role models for the other CHF patients in the class. All leaders in the study received training on the CDSMP protocol for 4 days prior to the intervention period in accordance with CDSMP training policies for programme dissemination (http://patienteducation.stanford.edu/licensing/). The training was provided by one of the authors (E.S.) and a CHF nurse specialist from the University Hospital Maastricht, who had both been instructed as master trainers at Stanford University in March 2004.34 Among other things, the leaders learned how to facilitate the process of action planning and problem solving and how to introduce cognitive symptom management techniques to the participants in the classes.
Measurements
Smoking and drinking behaviour, body mass, and physical activity were used to measure health behaviour. Smoking and drinking behaviour were assessed by asking the patients whether and how much they smoked (cigarettes, cigars or pipes) or drank alcoholic beverages at baseline and at each follow-up. Based on this we calculated the mean number of cigarettes/cigars/pipes smoked and the mean number of alcoholic drinks per week. Body mass was used as a proxy for nutritional habits and was assessed from the patients weight (in kilograms) and height (in metres). Body mass index (BMI) (kg/m2) was then calculated.38
Physical activity level was measured using a modified version of the ‘Physical Activities Scale’ and comprised questions about the frequency of the following three categories: walking for exercise, swimming, and bicycling.39 A fourth category called ‘other physical activities’ was added to the scale based on open-ended questions, in which patients could mention alternative activities. First, from all variously mentioned physical activities walk-related activities were included in the ‘walking for exercise’ category (e.g. walking the dog and shopping). Exercising on a home trainer was added to the ‘bicycling’ category. All other mentioned physical activities were then grouped on intensity level. As a result, ‘other physical activities’ included aerobic, stretching and strength exercises, sports, and gardening, as these were considered to be practised on a moderate level and therefore comparable with walking for exercise, swimming, and bicycling. At each assessment, patients were asked about the total number of minutes they had spent on walking for exercise, swimming, bicycling, and other physical activities in the preceding month.
Healthcare utilization was measured from the self-reported number of contacts with a general practitioner, cardiologist, other medical specialists, or CHF nurse specialist (telephone-based contacts and face-to-face contacts), hospital admissions, days in the hospital, days admitted to a rehabilitation centre, and visits to accident and emergency departments. No distinction was made between CHF- and non-CHF-related hospital admissions, as no valid differentiation between the two types could be made based on patients’ self-reports. At baseline, patients were asked about their healthcare utilization in the past 6 months. At each follow-up assessment, healthcare utilization was measured by asking the patient about healthcare utilization in the preceding month. This resulted in one summary score for each category of healthcare utilization for the total follow-up period.
Statistical analysis
Differences in background characteristics and outcomes at baseline between the intervention and control group were compared by means of χ2 tests, Mann–Whitney U tests, and t-tests for independent samples. Differences in the outcome variables were analysed with Mann–Whitney U tests, with the exception of BMI which was analysed with t-tests for independent samples. Body mass index was logarithmically transformed prior to the analyses. Data were analysed according to the intention-to-treat principle. In addition, per-protocol analyses were performed in which intervention group patients were included if they had attended at least four of the six programme sessions. All analyses were based on two-sided tests, and the results were considered significant if P < 0.05. SPSS for Windows version 12.0.1 was used.
Results
Participants and baseline characteristics
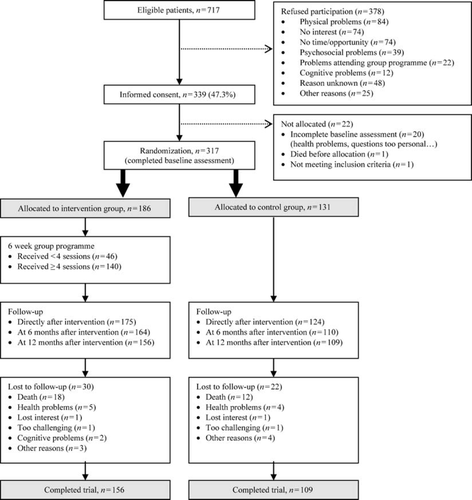
A total of 717 patients were eligible for participation in the trial, of whom 339 (47.3%) signed the informed consent form and underwent the baseline assessment. The remaining 378 patients refused or were unable to participate in the study, mainly due to physical problems, not being interested, or not having the time or the opportunity to participate in the study (Figure 1). Of the 339 patients, 317 completed the baseline assessment, of these 186 patients were allocated to the intervention group and 131 patients to the control group. A total of 265 patients (83.6%) completed the trial (baseline measurement plus at least the 12 month follow-up measurement), of these 156 patients were in the intervention group and 109 in the control group (83.9% and 83.2%, respectively). The reasons that patients were ‘lost to follow-up’ were comparable in both groups; death was the main reason in both the intervention and control groups (n = 18; 9.7% and n = 12; 9.2%, respectively).
Baseline characteristics were comparable for the intervention and control groups (Table 1). With regard to the outcome measures, patients in the intervention group tended to drink less alcohol per week and tended to spend less time on other physical activities per month at baseline compared with patients in the control group. However, these differences were not statistically significant (Table 2).
| Background characteristics | Control group (n = 131) | Intervention group (n = 186) | P-value |
|---|---|---|---|
| Males, n (%) | 89 (67.9) | 141 (75.8) | 0.122 |
| Age in years at time of inclusion, mean (SD) | 66.8 (10.1) | 66.6 (11.0) | 0.882 |
| Middle educational level, n (%)a | 90 (68.7) | 119 (64.3) | 0.207 |
| Not employed, n (%) | 113 (86.3) | 169 (90.9) | 0.198 |
| Not living alone, n (%) | 89 (67.9) | 124 (66.7) | 0.812 |
| NYHA class II CHF, n (%) | 91 (69.5) | 120 (64.5) | 0.358 |
| Number of active diseases, mean (SD)13 | 3.0 (1.5) | 3.0 (1.6) | 1.00 |
| Cognitive status (0–41)b, mean (SD)c | 32.4 (3.1) | 32.7 (3.3) | 0.407 |
- a Middle educational level: attended secondary (vocational) education.
- b Underlined score indicate the most favourable score.
- c Cognitive status as measured with the Telephone Interview for Cognitive Status (TICS).
| Control group (n = 131) | Intervention group (n = 186) | P-value | |||
|---|---|---|---|---|---|
| Mean (SD) | Median | Mean (SD) | Median | ||
| Smoking (number cigarettes per week) | |||||
| Baseline | 13.5 (40.7) | 0.0 | 10.2 (29.6) | 0.0 | 0.587 |
| Direct follow-up | 11.7 (37.0) | 0.0 | 9.0 (26.3) | 0.0 | 0.893 |
| 6 month follow-up | 8.4 (25.1) | 0.0 | 9.6 (28.8) | 0.0 | 0.902 |
| 12 month follow-up | 9.7 (27.9) | 0.0 | 10.0 (29.8) | 0.0 | 0.878 |
| Drinking (number alcoholic drinks per week) | |||||
| Baseline | 3.7 (6.3) | 0.0 | 2.8 (5.0) | 0.0 | 0.063 |
| Direct follow-up | 3.7 (6.2) | 0.0 | 3.6 (6.9) | 0.0 | 0.492 |
| 6 month follow-up | 3.9 (6.6) | 0.0 | 3.3 (6.5) | 0.0 | 0.122 |
| 12 month follow-up | 3.7 (6.2) | 0.0 | 3.2 (5.8) | 0.0 | 0.639 |
| Body mass indexa | |||||
| Baseline | 26.6 (4.1) | 26.6 | 27.0 (5.0) | 26.2 | 0.560 |
| Direct follow-up | 26.6 (4.2) | 26.5 | 27.0 (5.0) | 26.1 | 0.549 |
| 6 month follow-up | 27.0 (5.4) | 26.6 | 27.0 (5.3) | 26.0 | 0.979 |
| 12 month follow-up | 27.0 (4.0) | 26.9 | 27.2 (5.8) | 26.2 | 0.853 |
| Walking for exercise (min./month) | |||||
| Baseline | 563.3 (713.8) | 270.0 | 572.4 (791.0) | 315.0 | 0.877 |
| Direct follow-up | 588.1 (681.7) | 360.0 | 772.0 (998.0) | 540.0 | 0.034 |
| 6 month follow-up | 531.0 (780.4) | 270.0 | 753.3 (1050.1) | 450.0 | 0.068 |
| 12 month follow-up | 552.8 (706.5) | 315.0 | 628.2 (762.7) | 360.0 | 0.269 |
| Swimming (min/month) | |||||
| Baseline | 41.7 (181.4) | 0.0 | 22.2 (67.0) | 0.0 | 0.258 |
| Direct follow-up | 30.1 (141.8) | 0.0 | 33.8 (109.6) | 0.0 | 0.331 |
| 6 month follow-up | 52.8 (205.7) | 0.0 | 26.8 (86.5) | 0.0 | 0.217 |
| 12 month follow-up | 51.1 (196.3) | 0.0 | 47.8 (181.5) | 0.0 | 0.991 |
| Bicycling (min/month) | |||||
| Baseline | 209.1 (423.0) | 0.0 | 260.9 (526.0) | 0.0 | 0.872 |
| Direct follow-up | 220.8 (382.8) | 0.0 | 302.3 (520.4) | 40.0 | 0.176 |
| 6 month follow-up | 228.5 (471.7) | 0.0 | 280.6 (604.2) | 0.0 | 0.675 |
| 12 month follow-up | 233.5 (469.5) | 0.0 | 290.7 (614.0) | 25.0 | 0.356 |
| Other physical activities (min/month)b | |||||
| Baseline | 146.0 (846.2) | 0.0 | 144.0 (580.5) | 0.0 | 0.076 |
| Direct follow-up | 93.7 (219.1) | 0.0 | 224.5 (597.6) | 0.0 | 0.006 |
| 6 month follow-up | 86.3 (198.0) | 0.0 | 205.9 (649.5) | 0.0 | 0.036 |
| 12 month follow-up | 141.9 (309.7) | 0.0 | 282.5 (937.0) | 0.0 | 0.248 |
- a Analysed with t-tests for independent samples after logarithmic transformation. Unadjusted mean scores, SDs, and median scores are presented.
- b Other physical activities: aerobic, stretching and strength exercises, sports, and gardening.
Outcomes
Table 2 shows the effects of the CDSMP programme on health behaviour outcomes. No significant effects on smoking or drinking behaviour or body mass were found. Immediately after the end of the programme, patients in the intervention group walked for significantly more minutes per month and spent significantly more minutes per month for other physical activities compared with control patients. The mean time spent on walking increased by 25 min per month in the control group and 200 min per month in the intervention group. In terms of other physical activities such as aerobic, stretching and strength exercises, sports, and gardening, the mean time spent on these activities decreased by 52 min per month in the control group but increased by 81 min per month in the intervention group. The favourable effect on other physical activities extended to 6 months of follow-up (Table 2). No favourable long-term effect on walking for exercise was found. Furthermore, no significant differences between intervention and control group patients were found for swimming or bicycling (Table 2).
Regarding healthcare utilization, no significant differences were found between the control and intervention groups for the number of contacts with a general practitioner during the total follow-up period (both on average 4.6 contacts), contacts with a cardiologist (both on average 2.9 contacts), contacts with other medical specialists (on average 2.6 vs. 3.3 contacts, respectively), contacts with a CHF nurse specialist (telephone-based contacts; on average 1.5 vs. 2.0 contacts, respectively, and face-to-face contacts; on average 2.1 vs. 1.8 contacts, respectively), hospital admissions (both on average 0.4 admissions), days in the hospital (on average 3.7 vs. 4.9 days, respectively), and visits to accident and emergency departments (both on average 0.6 visits) (data not shown). Due to the fact that only a few patients had been admitted to a rehabilitation centre at baseline (n = 4 in the control group and n = 1 in the intervention group) and during follow-up (n = 1 in the control group and n = 4 in the intervention group), this outcome had to be excluded from the analyses.
The results of the per-protocol analyses (including control group patients and intervention group patients who attended at least four sessions; n = 271) were similar to the results of the intention-to-treat analyses (data not shown).
Discussion
This trial shows that the CDSMP substantially improved the time spent on walking for exercise among CHF patients immediately after the end of the programme. In addition, patients in the intervention group spent more time on other physical activities such as aerobic, stretching and strength exercises, sports, and gardening, directly after the programme and at 6 months of follow-up. No significant differences were found at 12 months of follow-up. In addition, the programme had no favourable effects on drinking or smoking behaviour, body mass, or healthcare utilization. Therefore, our results seem to be in line with previous studies, showing limited evidence of a beneficial effect of the CDSMP on health behaviour and healthcare utilization.15–20
The modest results on health behaviour and healthcare utilization might be explained by the fact that the contrast between the intervention and control group was too small for the detection of substantial additional effects of the programme. In the Netherlands, standard CHF care is at a relatively high level, since most Dutch hospitals including those in our study have a CHF management programme, which often comprises exercise programmes, behavioural interventions and regular checkups with education and counselling by a multidisciplinary team.40 One may consider that attention effects should be controlled for in the control group to make a clear comparison between the two study groups. However, attention through social support and exchanging personal experiences may be considered an essential component of the group intervention that is based on Bandura's self-efficacy theory.9,11 A second explanation might be the fact that the patients in the study already had low baseline levels of smoking and drinking, which makes it difficult to detect favourable effects of the programme. Most patients in the study were non-smokers or drank no more than the recommended maximum number of alcoholic beverages.36 Finally, the modest results on health behaviour may have been affected by patients’ emotional state, as emotional and symptom distress are associated with low motivation for behavioural change and physical inactivity.41,42 However, exploring the influence of emotional state on motivation for and maintenance of health behaviour change was beyond the scope of the present study.
The favourable short-term results of the programme on physical activity are consistent with the results of a feasibility study that was performed alongside this trial.43 This feasibility study showed that the percentage of participants who were still exercising according to their personal exercise plan fell from 78% directly after the end of the programme to 46% 1 year after attending the programme.43 Thus, in order to extend the short-term effects on physical activity, it seems important to increase long-term exercise adherence.
Duncan and Pozehl44 evaluated the additional value of nurse support on long-term exercise adherence among a small group of older CHF patients (n = 16; mean age = 66 years). Patients in the intervention and control groups underwent a 12 week group exercise programme and were instructed to do aerobic exercises at home; this was followed by a 12 week period of home-based exercise only. During both phases of the programme exercise, goals were set for the home-based exercise. However, patients in the intervention group were supported by a research nurse in terms of individualized graphic feedback and problem-solving techniques to improve exercise adherence. The study showed that exercise adherence was significantly improved during the second phase of the programme (i.e. home-based exercise only) in the patients who received nurse support when compared with control patients.44 This study gives an indication that nurse support may be effective in maintaining exercise adherence at home, which might be important in the follow-up period after attending a supervised programme. Motivational interviewing may also be considered an effective tool for enhancing exercise adherence. Brodie et al.45,46 evaluated an 8 week home-based programme that was based on motivational interviewing to explore ambivalence to physical activity and to integrate physical activity into the daily routine of older CHF patients (n = 92, of whom 60 completed follow-up; mean age = 78 years). Patients who attended the programme significantly improved physical activity at 5 months of follow-up, compared with patients who received standard recommendations regarding physical activity.45,46 Unfortunately, the studies of both Duncan and Pozehl44 and Brodie and co-workers45,46 comprised rather small sample sizes and did not study the long-term effectiveness of the programmes. Nevertheless, these studies give indications that supporting exercise on a daily level may improve exercise adherence among CHF patients.
Nurse specialists may have an explicit role in supporting long-term exercise adherence, perhaps even more than CHF peers. Although according to the CDSMP, CHF peers may be important in supporting behavioural change and adhering to these new behaviours, maintaining a self-support group consisting only of CHF peers may be challenging. In a feasibility study that was performed alongside this trial,43 we found that about 60% of the participants (n = 111) had called co-participants at least once for support, with an average of 2.5 calls during the 6 week programme (range 1–6). In addition, only a small group (n = 15) had kept in contact with one or more co-participants after 1 year of follow-up. Therefore, we consider nurse support on exercise adherence a better alternative when compared with the creation and maintenance of self-support groups of CHF peers. Enhancing exercise adherence at follow-up (i.e. after patients have attended the CDSMP class) could be included in outpatient CHF care during regular checkups. Nurse support could focus on continuing exercising according to plan and setting new goals to improve the integration of physical activity into patients' daily routines. In addition, nurse specialists may be able to adjust personal exercise goals if the patient's medical condition deteriorates or improves.
The present study has some limitations. First, all measures on health behaviour and healthcare utilization were self-reported. In addition, patients were questioned about their physical activities in the previous month, which may have been influenced by unforeseen circumstances like the weather or acute health problems. However, since both the intervention and control groups were measured in the same time period, it is unlikely that unforeseen fluctuations would have substantially influenced the results. Healthcare utilization was measured retrospectively, which may have resulted in some kind of recall-bias. Medical records were not reviewed to confirm the self-reports given by the patients. Finally, to obtain patients' BMI, height was recorded once at baseline, but weight was recorded at each assessment. A second limitation of the study is that the outcomes may have been affected by sample bias, as only about half of the eligible patients agreed to participate in the study (Figure 1). For example, about one-third of the non-participants (35.7%; n = 135) were physically or mentally unable to participate in the study. These patients may have been the most in need of targeting for behavioural change. However, one-third of the randomized patients in our study had NYHA Class III symptoms, indicating that our sample comprised symptomatic CHF patients as well. Therefore, we believe that the influence of sample bias on the basis of perceived health is somewhat limited.
Based on the results of our trial, we conclude that the CDSMP improves physical activity in the short term among CHF patients, but may need adaptations to affect healthcare utilization and to improve exercise adherence in the long term, in healthcare settings such as those in the Netherlands. Additional research is necessary to study whether adaptation of the CDSMP will increase effectiveness of the programme on health behaviour and healthcare utilization. In addition, future research should explore the influence of emotional and symptom distress on the motivation for and maintenance of health behaviour change.
Acknowledgements
We thank N. Steverink, H.A. Elzen, and J.P. Slaets from the University Medical Center Groningen, the Netherlands, for their willingness to share Dutch intervention materials. The Centre for Data and Information Management (MEMIC) of Maastricht University is acknowledged for their assistance in the data collection. We also thank all patients and practitioners of the University Hospital Maastricht, Atrium Medical Centre Heerlen, VieCuri Medical Centre Venlo, Laurentius Hospital Roermond, Maasland Hospital Sittard, and Elkerliek Hospital Helmond for their efforts that enabled evaluating the CDSMP among CHF patients in the Netherlands.
Funding
We thank the Netherlands Heart Foundation (2002B005) and the University Hospital Maastricht (PF 179) in the Netherlands for funding this research project. The project was conducted within the School for Public Health and Primary Care: CAPHRI of Maastricht University in the Netherlands in cooperation with Lorig et al. from Stanford University.
Conflict of interest: none declared.




