Continuous central haemodynamic measurements during the six-minute walk test and daily life in patients with chronic heart failure
Abstract
Aims
To compare haemodynamic responses during the 6-min walk test (6MWT) and daily living activities in heart failure (HF) patients.
Methods and results
Eighteen HF patients received an implantable haemodynamic monitor, which continuously measured heart rate (HR), estimated pulmonary artery diastolic pressure (ePAD), and several right ventricular (RV) pressure parameters. During the 6MWT, haemodynamics were assessed at rest and peak exercise. Ambulatory values were measured as the daily minimum, maximum, and median, averaged over the 14-day period surrounding each 6MWT. During the 6MWT, HR increased from 71 ± 17 to 101 ± 20 b.p.m. and ePAD from 20 ± 5 to 34 ± 8 mmHg. Daily minimum values were significantly lower and daily maximum values higher compared with rest and peak exercise. Patients with a walked distance above the median (402 m) had lower resting HR (64 ± 10 vs. 77 ± 20, P = 0.001) and ePAD (18 ± 4 vs. 21 ± 7, P = 0.022) compared to patients with walked distances below the median; values at peak exercise were similar. This pattern was also observed during the ambulatory periods.
Conclusion
Ranges of HR and RV pressures are significantly larger during daily living activities compared with 6MWT in HF patients. Haemodynamic characteristics of patients with greater exercise capacity include lower resting HR and RV pressures and are similar during the 6MWT and daily life.
Introduction
Chronic heart failure (HF) is a common condition affecting approximately 2% of Western populations with a marked increase among the elderly.1 HF is often associated with severe and disabling symptoms such as dyspnoea, fatigue, and limited exercise tolerance. While dyspnoea and fatigue are difficult to quantify objectively, exercise tolerance can be measured by standardized test procedures. Accordingly, the response of clinical symptoms and functional parameters to exercise is commonly used to classify HF disease severity2 and plays an important role in risk stratification and the choice of appropriate treatment strategies.3–5 The six-minute walk test (6MWT) is widely used in routine practice and clinical trials6 as a simple tool to assess functional capacity in HF patients and is thought to reflect the activity of daily living better than the evaluations at peak exercise.7–9 Furthermore, the distance covered during 6 min of walking has been shown to be highly reproducible,10 correlate with patient symptoms,10 and has been identified as an independent predictor of morbidity and survival in patients with left ventricular (LV) dysfunction.11
However, it remains unclear, whether this ‘snapshot picture’ from an artificial laboratory test truly reflects the exercise levels a HF patient is exposed to during his activities of daily living. Likewise, despite the important role of cardiac-filling pressures in the pathophysiology of HF,12 it is not known if the responses of heart rate (HR) and filling pressures to submaximal exercise are comparable to the haemodynamic response during ambulatory conditions. Thus far, owing to the obvious limitations of invasive haemodynamic studies, it has not been possible to readily address these issues by means of serial right heart catheterization. Recently, an implantable haemodynamic monitor (IHM) has been shown to yield reliable central haemodynamic information in HF patients over time.13,14 In addition to its potential to guide HF treatment,15–17 the IHM offers a unique opportunity for serial assessments of central haemodynamic values during exercise tests.18
The aim of this study was to compare the haemodynamic responses to the 6MWT, with those continuously recorded during daily living activities in patients with chronic HF. We hypothesized that this information would be valuable to better understand the relation between haemodynamic changes observed during a standard exercise test and those experienced during ambulatory conditions and to further elucidate the impact of central haemodynamic measurements on exercise tolerance in patients with HF.
Methods
Patient population
Patients were recruited from a multicentre, prospective, non-randomized trial investigating the accuracy and reliability of an investigational IHM (Chronicle®; Model 9520, Medtronic, Inc.) system over time.14,15 All patients had chronic HF for >3 months and were not expected to undergo heart transplantation within 12 months of study enrolment. Patients were excluded if they had any known uncorrected congenital heart disease, tricuspid or pulmonic stenosis, a mechanical right heart valve prosthesis, a previously implanted device in which transvenous leads remained in the heart, a terminal illness unrelated to their HF with life-expectancy <1 year, or if they were unable to give consent. The study conformed to the principles outlined in the Declaration of Helsinki. Local Ethics Committees approved the protocol and all patients gave their written consent to the study. Patients included in this sub-analysis performed two to four consecutive walk tests within the first 10 months of follow-up and had at least 14 days of continuous ambulatory haemodynamic data measurements available in the period immediately before and after each walk test. Before implantation of the IHM, standard Doppler echocardiography was performed and patient status was assessed including NYHA functional class and blood pressure.
Implantable haemodynamic monitoring system
The IHM system used in this study has been described elsewhere.14,19,20 In brief, it consists of a memory device implanted in the subcutaneous pre-pectoral area. The pressure sensor lead (Model 4328A, Medtronic, Inc.) was positioned in the right ventricle (RV) with the tip in a high septal or outflow tract position. Signal processing detected HR, RV diastolic pressure (RVDP, pressure measured at the detection of R-wave), RV systolic pressure (RVSP, maximum pressure), RV pulse pressure (RVPP = RVSP − RVDP) and the maximum rate of pressure increase or decrease (max ± dP/dt). Also, the pressure at max + dP/dt was determined to estimate pulmonary artery diastolic pressure (ePAD) according to the methods validated previously.21–23
Haemodynamic variables were measured continuously (24 h a day) in a beat-to-beat fashion and stored as the median, and 6th and 94th percentile over intervals of 6 or 25 min, depending on the follow-up schedule. During the 6MWT, high-resolution data storage (2 s) was used. Each patient was provided with an external pressure reference device (Model 2805, Medtronic, Inc.) to correct the absolute pressure measured by the IHM for ambient atmospheric pressures upon device interrogation.
Six-minute walk tests
Six-minute walk tests were conducted in a standardized fashion according to the instructions published by Lipkin et al.8 Patients performed one test on each occasion as recommended in recent guidelines24 and were advised to take their medication as usual on the day of the 6MWT. Prior to the 6 min walk, patients remained quiet in resting supine position for at least 10 min. Haemodynamic values from the last 60 s of this resting period were averaged (REST). Peak exercise values (PEAK) were defined as the mean of 21 cardiac cycles taken at the end of exercise. The average interval between the walk tests was 2.3 ± 1.6 months with a minimum of 13 days. At the PEAK of the 6MWT, patients rated their self-perceived level of exertion using the 15-point Borg scale ranging from ‘6’ (very, very light effort) to ‘20’ (exhaustion).25
Ambulatory data
For the comparison between haemodynamic values during 6MWT and ambulatory activities, data recorded by the IHM during the 7-day period immediately before and 7 days after each 6MWT were analysed, excluding the day of exercise. There was no significant difference between ambulatory haemodynamic values 7 days before and 7 days after the 6MWT. Therefore, values of haemodynamic variables representing the ambulatory daily median, daily minimum (6th percentile), and daily maximum (94th percentile) from the 14 days surrounding each 6MWT were averaged to account for daily variability.
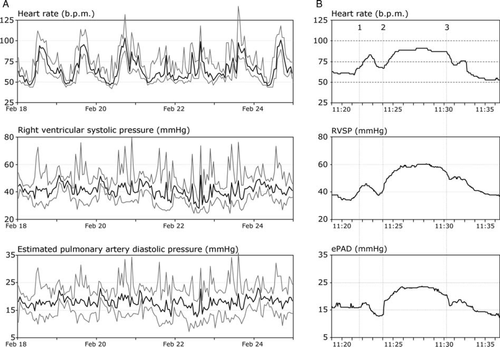
The daily range of ambulatory haemodynamic values was calculated as the difference between the daily minimum and maximum values and averaged over the 14 days. It was surmised that minimum and maximum values would be reflective of the average haemodynamic boundaries of rest and peak stress experienced during activities of daily living. A representative example showing haemodynamic trends during ambulatory periods and a 6MWT in one patient is given in Figure 1.
Statistical methods
Statistical analysis was performed using standard commercial software (Excel, Microsoft, Seattle, USA) and Statistica (Statsoft, Tulsa, USA). Data are given as mean ± SD or median ± percentile where appropriate. For comparisons of haemodynamic responses by patient characteristics (age, gender, baseline NYHA class), the results from all consecutive 6MWT and the corresponding ambulatory periods were averaged for each patient (n = 18). For comparisons of responses in patients with a walking distance below or above the median of 402 m and between patients in NYHA class I/II vs. III, the two-sided unpaired Student's t-test was applied using all individual tests (n = 62). Simple correlation analysis was used to determine the relation between walking distance or Borg symptom score and haemodynamic variables. The coefficient of variation (CV) was calculated using variance analysis. A P-value of <0.05 was considered statistically significant.
Results
Of the 32 patients included in the main study,14,15 18 fulfilled the criteria for inclusion in the present report (Table 1). These 18 patients performed 62 walk tests within 218 ± 68 days of follow-up after the IHM implant. Nine patients performed four tests each, eight patients did three tests, and one patient did two tests. There were no significant differences in baseline haemodynamic values between patients in NYHA class I/II (n = 8) compared with those in NYHA class III (n = 10).
| Number of patients | 18 |
|---|---|
| Sex (M/F) | 12/6 |
| Age (years) (range) | 57 ± 11 (40–75) |
| LVEF (%) (range) | 26 ± 8 (14–35) |
| NYHA class I/II/III (n) | 1/7/10 |
| HF aetiology, ischaemic (n) | 9 |
| Blood pressure, systolic (mmHg) | 113 ± 24 |
| Blood pressure, diastolic (mmHg) | 65 ± 8 |
| Heart rate (b.p.m.) | 76 ± 17 |
| Respiratory rate (1/min) | 17 ± 3 |
| Body mass index (kg/m2) | 29 ± 6 |
| Medication use (n) | |
| β-Blockers | 14 |
| ACE-I | 18 |
| Loop diuretics | 15 |
- a M, male; F, female; LVEF, left ventricular ejection fraction; NYHA, New York Heart Association; HF, heart failure; ACE-I, angiotensin-converting enzyme-inhibitor. Baseline characteristics were assessed before implantation of the implantable haemodynamic monitor.
Six-minute walk test
Patients walked on average 383 ± 98 m in the 6MWT and perceived their exertion as 12.6 ± 3.0 on the Borg scale, which reflects a moderate level of exertion (‘somewhat hard’). The walked distance covered by each individual during the repeated tests varied little over time as indicated by a mean CV of 10.5%. Similarly, Borg scale values showed little variation of 11.3%. The eight patients in NYHA class I/II at the time of testing had a longer walked distance (410 ± 58 m) compared with the 10 patients in class III (357 ± 113 m). However, this difference did not reach statistical significance.
During the resting period preceding the 6MWT, pressures were moderately elevated, as expected in this group of patients with chronic HF (Table 2). During the 6MWT, HR increased by 45% to a maximum of 102 ± 21 b.p.m. corresponding to 61% of the age-matched predicted maximal HR for these patients.26 Furthermore, the RVSP, RVDP, and ePAD increased by 58%, 93%, and 72% during the 6MWT, respectively, while RV + dP/dtmax increased by 95%. The magnitude of pressure increase during the 6MWT (n = 62) correlated with the walked distance, yielding Pearson correlation coefficients (r) of 0.45, 0.56, and 0.46 for RVSP, RVDP, and ePAD, respectively (all had P < 0.001).
| 6 min Walk test | Ambulatory | |||
|---|---|---|---|---|
| Rest (mean ± SD) | Peak (mean ± SD) | Daily minimum (mean ± SD) | Daily maximum (mean ± SD) | |
| HR (b.p.m.) | 70.4 ± 17.0 | 102.1 ± 21.0 | 59.3 ± 12.2* | 108.2 ± 17.5* |
| RVSP (mmHg) | 37.7 ± 13.7 | 59.5 ± 15.2 | 31.0 ± 10.1* | 68.0 ± 17.5* |
| RVDP (mmHg) | 8.4 ± 4.1 | 16.2 ± 5.9 | 4.8 ± 4.0* | 25.2 ± 7.7* |
| RVPP (mmHg) | 28.2 ± 11.6 | 41.7 ± 12.3 | 21.5 ± 7.5* | 49.1 ± 14.9* |
| ePAD (mmHg) | 19.6 ± 5.9 | 33.8 ± 8.1 | 16.0 ± 5.1* | 43.1 ± 9.7* |
| dP/dtmax (mmHg/s) | 336 ± 93 | 657 ± 219 | 269 ± 79* | 777 ± 252* |
- * P < 0.05; 6-min walk rest vs. ambulatory daily minimum and 6-min walk peak vs. ambulatory daily maximum. HR, heart rate; RVSP, right ventricular systolic pressure; RVDP, right ventricular diastolic pressure; RVPP, right ventricular pulse pressure; ePAD, estimated pulmonary artery diastolic pressure.
Because repeated 6MWT might induce a training effect, we performed separate analysis of the first and second 6MWT (36 tests, 18 patients). There was no significant difference in the walked distance (378 ± 92 m vs. 364 ± 125 m; ns) and all haemodynamic values at rest, peak exercise, and during the corresponding ambulatory periods were similar between the two tests. Furthermore, gender and age may impact the walked distance and results from the Borg scale. However, in our study, female (n = 6) and male (n = 12) patients had a similar walked distance (366 ± 108 m and 388 ± 90 m; ns) and Borg score (12.8 ± 2.8 vs. 12.0 ± 2.7; ns). There was no correlation between age and the walked distance (r = 0.001) or Borg score (r = 0.019).
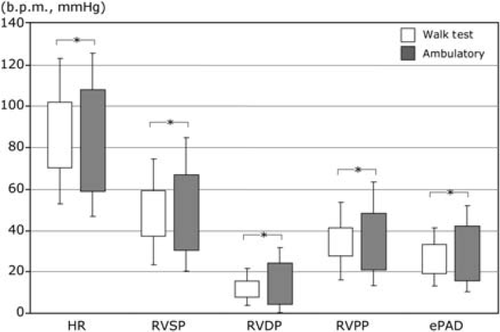
Comparison of ambulatory haemodynamic response and walk tests
The minimum and maximum haemodynamic values measured from the implantable monitor during 6MWT and the ambulatory periods are shown in Table 2 and Figure 2. For all variables, ambulatory minimum values were significantly lower and ambulatory maximum values significantly larger compared with corresponding REST and PEAK values during the 6MWT. Accordingly, the ambulatory range between minimum and maximum HR was 54% larger when compared with 6MWT, and the ambulatory range was 67%, 154%, and 87% larger with regard to RVSP, RVDP, and ePAD, respectively.
Patients with a lower HR during the ambulatory periods had a better exercise capacity resulting in a negative correlation between the median ambulatory HR and the walked distance (r = −0.62; P < 0.001; n = 64). Likewise, both the daily minimum HR (r = −0.61; P < 0.001) and the daily maximum HR (r = −0.32; P = 0.013) were associated with a longer walked distance, while the daily range of HR and ambulatory pressure ranges were not.
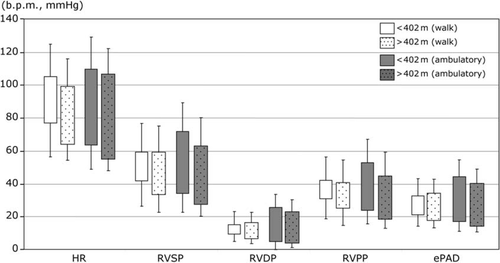
Patients with short vs. long walk distances
To further elucidate the relationship between exercise capacity and haemodynamic measurements, the responses from the 6MWT in which patients' walked distances were below the median of 402 m (n = 30) were compared to those tests with walked distances >402 m (n = 32). Table 3 and Figure 3 show a significantly greater increase of HR and pressures during the 6MWT in tests where the patients walked >402 m (P < 0.05). This was generally because of significantly lower REST values (Table 3), while there was no difference between PEAK values.
| Walk distance | |||
|---|---|---|---|
| <402 m (n=30) | >402 m (n=32) | ||
| Rest 6-min walk | |||
| HR (b.p.m.) | 77.0 ± 20.5 | 64.2 ± 9.9 | 0.001 |
| RVSP (mmHg) | 42.1 ± 15.4 | 33.6 ± 10.7 | 0.009 |
| RVDP (mmHg) | 9.8 ± 4.6 | 7.1 ± 3.0 | 0.005 |
| RVPP (mmHg) | 31.1 ± 12.2 | 25.4 ± 10.5 | 0.035 |
| ePAD (mmHg) | 21.4 ± 6.9 | 17.9 ± 4.3 | 0.022 |
| Peak 6-min walk | |||
| HR (b.p.m.) | 105.4 ± 24.6 | 99.0 ± 16.7 | ns |
| RVSP (mmHg) | 59.6 ± 14.9 | 59.4 ± 15.6 | ns |
| RVDP (mmHg) | 15.6 ± 5.7 | 16.8 ± 6.1 | ns |
| RVPP (mmHg) | 42.5 ± 11.0 | 41.0 ± 13.6 | ns |
| ePAD (mmHg) | 33.0 ± 7.7 | 34.5 ± 8.4 | ns |
| Daily minimums ambulatory | |||
| HR (b.p.m.) | 63.9 ± 14.8 | 55.1 ± 7.0 | 0.001 |
| RVSP (mmHg) | 34.5 ± 11.6 | 27.7 ± 7.3 | 0.008 |
| RVDP (mmHg) | 5.2 ± 4.9 | 4.3 ± 2.9 | ns |
| RVPP (mmHg) | 24.3 ± 8.3 | 18.8 ± 5.7 | 0.005 |
| ePAD (mmHg) | 17.6 ± 6.0 | 14.5 ± 3.6 | 0.028 |
| Daily maximums ambulatory | |||
| HR (b.p.m.) | 109.9 ± 19.5 | 106.5 ± 15.6 | ns |
| RVSP (mmHg) | 72.8 ± 17.3 | 63.6 ± 16.9 | 0.042 |
| RVDP (mmHg) | 26.9 ± 7.9 | 23.6 ± 7.2 | 0.099 |
| RVPP (mmHg) | 53.5 ± 14.2 | 45.0 ± 14.6 | 0.017 |
| ePAD (mmHg) | 45.5 ± 10.4 | 40.8 ± 8.6 | 0.074 |
| Daily median ambulatory | |||
| HR (b.p.m.) | 82.6 ± 16.9 | 71.8 ± 8.8 | 0.001 |
| RVSP (mmHg) | 51.4 ± 15.1 | 41.4 ± 11.1 | 0.004 |
| RVDP (mmHg) | 14.7 ± 5.7 | 11.8 ± 3.5 | 0.035 |
| RVPP (mmHg) | 35.7 ± 11.1 | 28.9 ± 10.1 | 0.011 |
| ePAD (mmHg) | 30.0 ± 8.6 | 24.6 ± 4.6 | 0.006 |
- a HR, heart rate; RVSP, right ventricular systolic pressure; RVDP, right ventricular diastolic pressure; RVPP, right ventricular pulse pressure; ePAD, estimated pulmonary artery diastolic pressure.
Interestingly, the same pattern of lower HR and pressures in the group with a longer walked distance was also observed during the ambulatory periods surrounding each 6MWT. Thirty-two ambulatory periods from patients with 6MWT >402 m compared with 30 ambulatory periods in those with 6MWT <402 m had significantly lower daily minimum values of HR, RVSP, RVPP, and ePAD. In addition, they showed significantly lower daily maximum values of RVSP and RVPP and a trend towards a lower maximum ePAD (P = 0.074). Since both daily minimum and maximum pressures were lower, the magnitude of daily ranges was not different between the two groups.
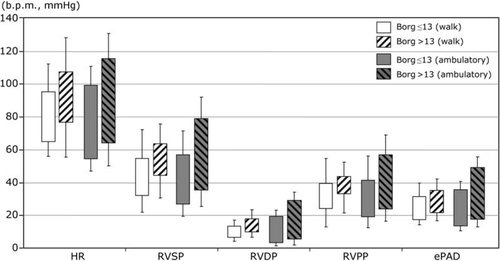
Borg symptom score
Patients with shorter walked distance in their 6MWT also perceived a higher level of exhaustion as indicated by their levels on the Borg scale obtained at each test (r = −0.31; P = 0.015; n = 62). For further analysis, we divided our patients into two groups with an average post-walk Borg score above or below the median (≤13; n = 9 and >13; n = 9, respectively). Patients reporting a higher degree of exhaustion at the end of their walk tests were characterized by higher HRs and pressures both at rest and after the 6MWT (Figure 4). A similar pattern was observed during the corresponding ambulatory periods. In particular, patients with more exercise-related symptoms according to the Borg score reached higher maximum values of HR during both the 6MWT (r = 0.55, P = 0.017) and the ambulatory periods (r = 0.62, P = 0.006). Likewise, there were correlations between the Borg score and cardiac-filling pressures (ePAD) both during the 6MWT (r = 0.47, P = 0.048) and the ambulatory periods (r = 0.75, P < 0.001).
Discussion
The present study compares changes in central haemodynamic variables during the 6MWT with those obtained during activities of daily living, continuously measured by an implantable haemodynamic monitor in patients with chronic HF. For all analysed haemodynamic variables, ambulatory minimum values were significantly lower than resting values before the 6MWT, and ambulatory maximum values were significantly higher than those measured at peak exercise. This implies that the haemodynamic response to the 6MWT represents only a portion of the physiological variation of the haemodynamic load experienced during daily living activities in HF patients. However, certain patterns of haemodynamic response observed during the ambulatory periods were related to findings in the 6MWT. This novel observation supports the usefulness of the 6MWT to reflect daily living activities and the potential utility of the ambulatory haemodynamic data to reflect findings from the 6MWT.
Ambulatory haemodynamic ranges were measured as the difference between daily 6th and 94th percentile values, meaning that the lowest and highest 6% of HR and pressure values were filtered from the analysis. Thus, our findings are not sensitive to haemodynamic outliers caused by transient haemodynamic provocations such as orthostatic reflexes, coughing, or arrhythmia. Furthermore, ambulatory haemodynamic variables were averaged over a 14-day period to account for daily variability. Therefore, we likely underestimated the magnitude of haemodynamic ranges experienced during daily living and the true differences between ambulatory haemodynamic responses and those during the 6MWTs may be even larger.
Our findings may provide further insight into HF exercise physiology. Common haemodynamic examinations carried out with the patient at supine rest and/or during standard exercise tests are usually bound to the artificial laboratory environment and do not adequately represent what might be considered as the ‘haemodynamic reality’ of the patient. Certainly, standardized tests are useful to compare results between patients and to document changes in functional capacity in the same individual over time. However, it seems important to bear in mind, that the real life haemodynamic levels of HF patients away from the clinic are quite different.
In this study, HR, RVSP, and ePAD increased by 44%, 57%, and 71% during the 6MWTs. The blunted response in PEAK HR, reaching only 62% of the predicted maximum, may in part be explained by chronotropic incompetence, which is common in HF patients owing to electrophysiological alternations or medication with β-blockers. In addition, HF patients often have blunted baroreflex responses that might limit HR responses during stress.27,28 However, patients who had a lower maximum HR performed better on the 6MWT and had less exertional fatigue during exercise, suggesting that chronotropic incompetence was not the primary reason for a limited exercise capacity. In contrast to previous invasive exercise studies in HF, which identified HR as an important determinant of exercise tolerance,29 our patients were treated with β-blockers and were not assessed at their maximum workload.
Ohlsson and coworkers18 were the first to use implanted haemodynamic monitors during 6MWT. They recorded similar haemodynamic changes corresponding to 65–77% of the HR, RVSP, and ePAD responses measured during maximal bicycle exercise. This reflects the principle of the sub-maximal 6MWT, where patients adjust the level of exercise to the degree of incapacitating symptoms. Instead of comparing the maximum workload, the walked distance is measured and can be compared over time. Other reports indicate that the walked distance correlates with NYHA functional class and prognosis in HF.10,11,30 In this study there was no significant difference in walked distance between groups of NYHA classes, possibly owing to the small sample size. However, the walked distance correlated with an increase of RVSP, RVDP, and ePAD achieved during the tests.
When patients were able to walk >402 m, resting RV and pulmonary arterial pressures were lower compared with patients who could only walk <402 m. This might either indicate better volume management and/or a lesser degree of LV dysfunction and HF severity in patients with lower filling pressures. Interestingly, both patient groups reached similar haemodynamic values at peak exercise. It might be speculated that these peak values represented a physiological limit during sub-maximal exercise beyond which a further increase in workload would have caused more severe symptoms. In fact, patients with higher cardiac-filling pressures (ePAD) at peak exercise reported more severe symptoms measured by the Borg score and a higher Borg score was also associated with a shorter walked distance. Furthermore, patients who started their 6MWT at lower filling pressures were able to perform a higher workload and to accomplish a longer walk with less dyspnoea and fatigue.
Patients with a better exercise capacity (walked distance >402 m) had lower daily minimum and median values of HR and RV pressures from their ambulatory data. In particular, the daily minimum and daily median HR was 8 and 10 b.p.m. lower among patients with a better exercise capacity. This is consistent with the well-known role of HR as a marker of cardiac autonomic control31,32 and its link to the severity and prognosis of HF.33 Another potential explanation for these differences is that some of the patients may have been more optimally treated with β-blockers or other cardiovascular medication, although there was no difference in drug prescriptions between patients walking more or less than 402 m.
An interesting observation in our study was that ambulatory haemodynamic differences between patient groups dichotomized by either walking distance or Borg score were consistent with findings during the 6MWT. Theoretically, individuals with less severe HF might have a more physically active lifestyle inducing larger ambulatory increases in HR and filling pressures. In contrast, we found that patients with better exercise capacity and minor exertional symptoms during the 6MWT had a more favourable haemodynamic profile during both the 6MWT and daily life, characterized by lower minimum and maximum levels of HR and RV pressures. This suggests that these patients generally experienced fewer limitations during their ambulatory activities while those with more severely compromised haemodynamics frequently approached their physiological limits in order to cope with the requirements of daily life.
Thus, despite the disparity of haemodynamic ranges between the 6MWT and the corresponding ambulatory periods, our data indicate that the walked distance and Borg symptom scores reflect the underlying haemodynamic condition of the patients both during the test and during daily living activities. This is in support of the rationale behind the 6MWT designed to represent daily living conditions in HF patients.9
During our study, subjects were remarkably stable without major clinical events or treatment changes, which is also consistent with the small variation in walking distance and Borg score over time. Therefore, we could not address the question whether individual changes over time in exercise capacity and haemodynamic values recorded by the IHM are directly interrelated. Such correlation has previously been observed by Sutcliffe and coworkers, who found that changes in PA diastolic pressure were the most powerful determinant of changes in peak VO2 in a large group of patients with severe HF, who were assessed by right heart catheterization at two points of time.34
Limitations
This study did not evaluate other measures of haemodynamic response, such as LV function or oxygen uptake, which are important predictors of exercise tolerance in HF. The sample size was limited to patients included in the main study.14,15 However, the use of continuously recorded haemodynamic data and serial 6MWT allowed us to increase the number of observations. Medication, in particular the use of β-blockers, has a major impact on the response of cardiac-filling pressures and HR to physical activity. For the purpose of this study, we surmised, this impact would be similar during the 6MWT and the corresponding ambulatory periods.
Conclusion
In HF patients, the ambulatory ranges of haemodynamic values are large and markedly exceed the changes associated with 6MWTs. Patients with lower HRs and filling pressures during ambulatory periods, also have better exercise tolerance during 6MWT (>402 m) and less symptoms on exertion (Borg≤13), thus verifying the usefulness of the 6MWT as a sub-maximal exercise test. In addition, the relation between ambulatory haemodynamic levels and the 6MWT suggests a potential role for ambulatory monitoring in the ongoing evaluation of functional status in patients with chronic HF.
The haemodynamic characteristics observed during the patient's daily living conditions are representative of the 6MWT findings which confirms the usefulness of the 6MWT as a submaximal exercise test and suggests a potential value of ambulatory monitoring in the evaluation of functional status in patients with chronic HF.
Funding
This study was sponsored by Medtronic, Inc., Minneapolis, MN, USA.
Conflict of interest: FB and CL receive research funding from and have worked as consultants for Medtronic. PBA and EE have worked as consultants for Medtronic. BK and TB are employees at Medtronic Inc, Minneapolis, MN.




